Vesical Artery Embolisation in Management of Haematuria due to Radiation-induced Haemorrhagic Cystitis: A Case Report
Vishal Nandkishor Bakare1, Ritesh Kumar Sahu2, Ravi Arya3, Pratiksha Yadav4
1 Assistant Professor, Department of Interventional Radiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, Maharashtra, India.
2 Senior Resident, Department of Interventional Radiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, Maharashtra, India.
3 Senior Resident, Department of Interventional Radiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, Maharashtra, India.
4 Professor and Head, Department of Interventional Radiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratiksha Yadav, Professor and Head, Department of Interventional Radiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune-412303, Maharashtra, India.
E-mail: bakarevishal3@gmail.com
Radiation therapy is often utilised for the treatment of pelvic malignancies. Radiation-induced haemorrhagic cystitis can occur in such patients and may sometimes lead to uncontrolled haematuria. Various treatment modalities for managing this condition include urinary bladder irrigation, cystoscopy-guided procedures, hyperbaric oxygen therapy, fulguration, and other surgical techniques. Transarterial super-selective vesical artery embolisation has emerged as a modern management technique for patients with refractory radiation-induced haemorrhagic cystitis. Hereby, the authors present a case report of a 62-year-old elderly female patient diagnosed with radiation-induced haemorrhagic cystitis, which was refractory to continuous urinary bladder irrigation and medical management. She was successfully treated with super-selective vesical artery embolisation, resulting in complete resolution of haematuria, even on follow-up. This minimally invasive and effective modality can be utilised as a first-line therapy as well as in cases where other treatment options have failed.
Cystoscopy, Pelvic malignancies, Urinary bladder irrigation
Case Report
A 62-year-old female presented to the Emergency Department with chief complaints of blood in her urine and painful micturition for the past 4-5 days. There was no history of trauma, fever, or any anticoagulation medications. Her medical history included a diagnosis of cervical carcinoma, for which she underwent surgery and chemoradiation that concluded one year ago.
On clinical examination, the patient appeared thin, with a pulse of 110 beats per minute and a blood pressure of 100/70 mmHg. Severe pallor was noted, and her abdomen was soft. A pervaginal examination revealed no significant genital tract bleeding; however, blood clots were present in her urine. Blood investigations indicated a low haemoglobin level of 5.0 g/dL, a platelet count of 220,000/dL, and a normal coagulation profile and kidney function tests. The patient was stabilised haemodynamically and a blood transfusion was administered.
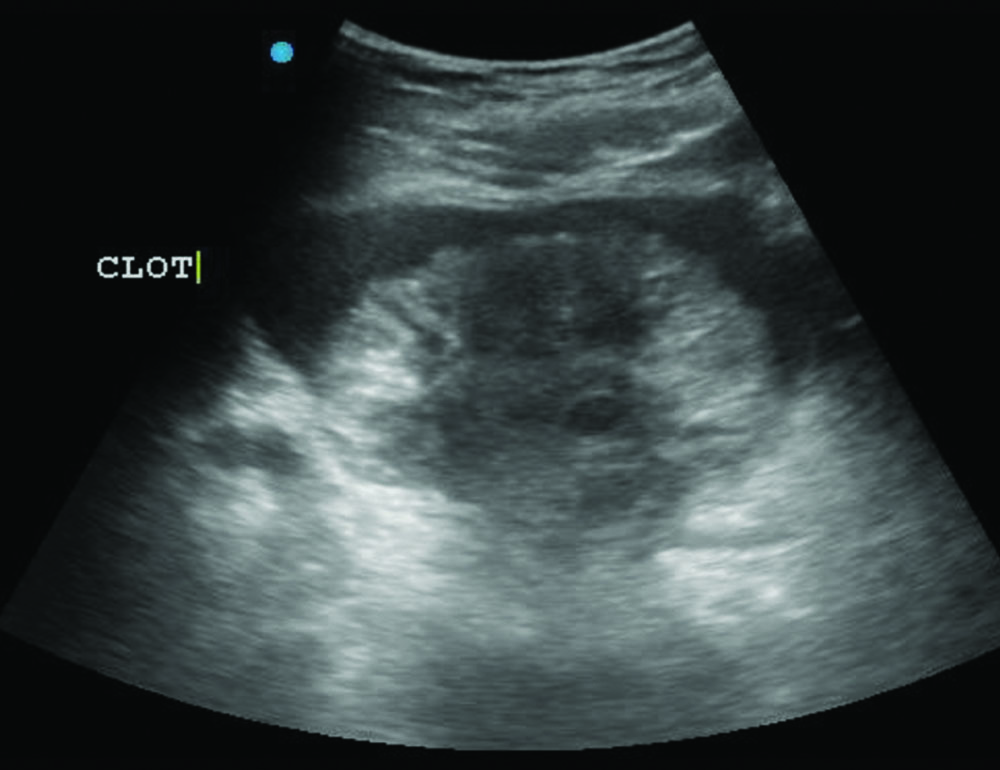
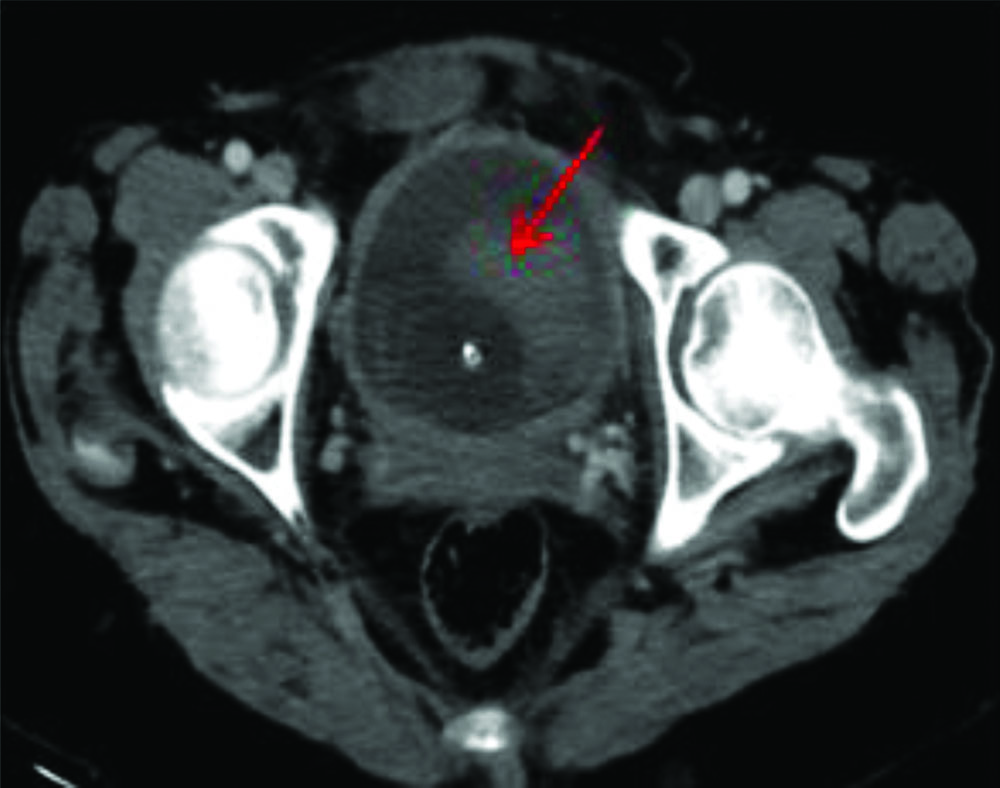
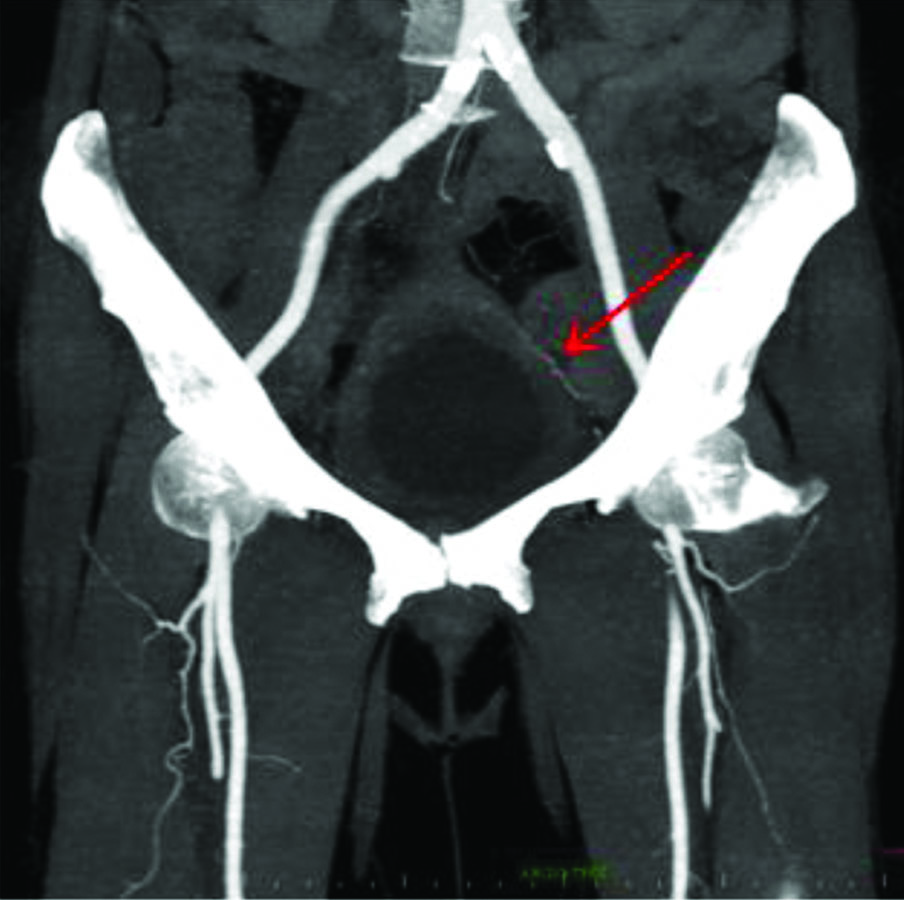
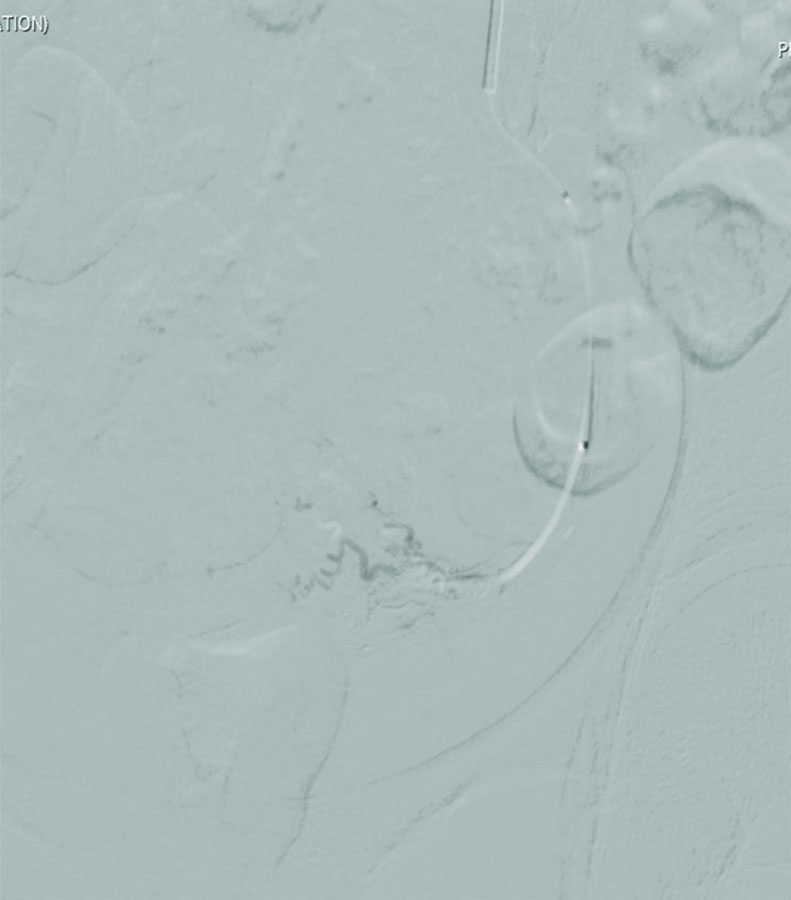
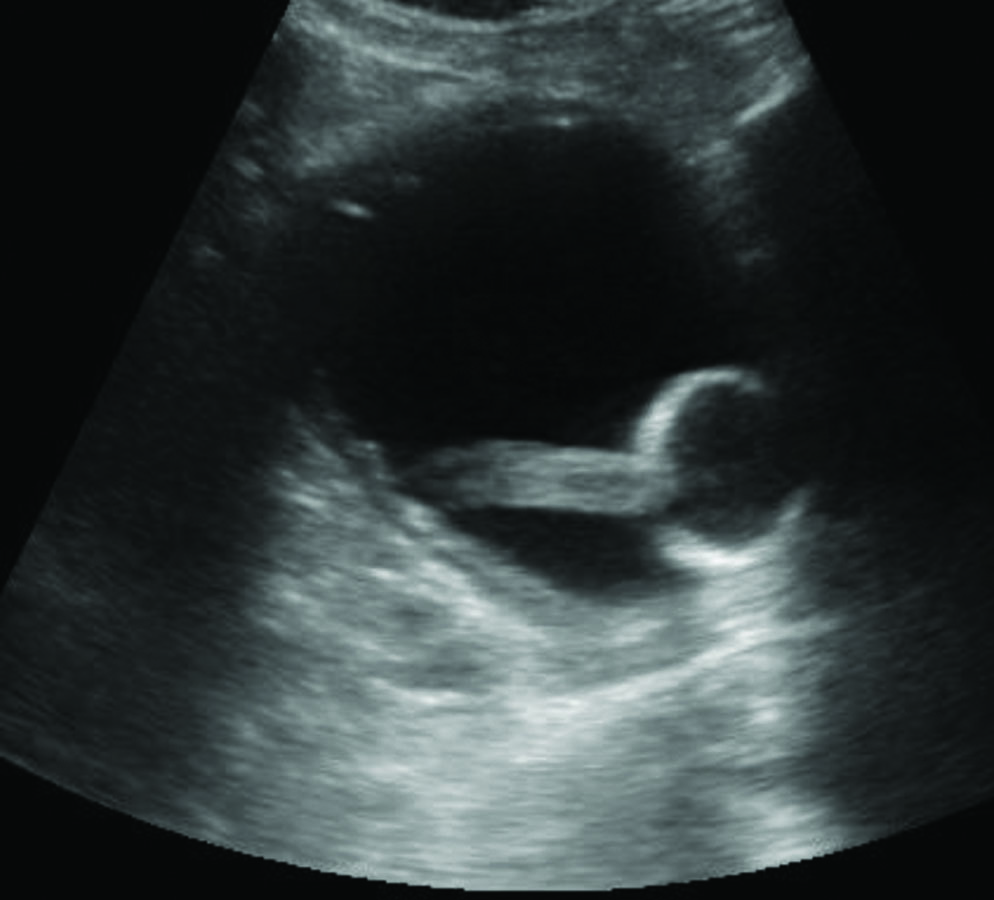
The ultrasound of the abdomen and pelvis revealed thickened walls of the urinary bladder, suggestive of chronic cystitis, along with a luminal clot [Table/Fig-1]. The Computed Tomography (CT) scan images confirmed the presence of blood clots inside the lumen of the urinary bladder. The hypertrophied left superior vesical artery seen on the CT angiography image has been depicted in [Table/Fig-2,3]. These findings were further confirmed via cystoscopy. Evacuation of the clot was performed, and bladder irrigation was initiated using a three-way catheter. However, there was persistent haematuria that led to a continuous decline in haemoglobin levels. The case was referred to the interventional radiologist, and a plan for transarterial super-selective vesical artery embolisation was established.
Ultrasound image showing the hyperechoic blood clot inside the urinary bladder.
Axial CT scan image showing the hyperdense blood clot inside the urinary bladder adjacent to the bulb of Foley’s catheter.
Coronal CT angiography image showing the prominent left superior vesical artery.
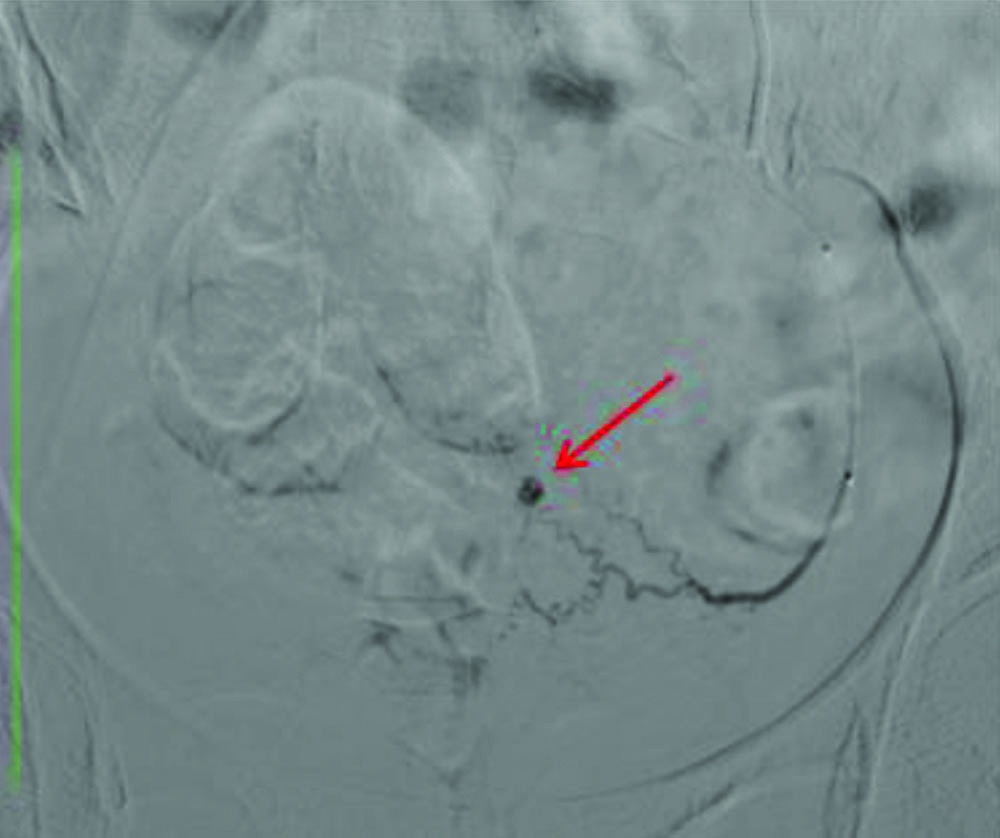
Under ultrasound guidance and local anaesthesia with an injection of 2% lignocaine, the right common femoral artery was cannulated with a 5 Fr vascular sheath. Subsequently, using a 5 Fr Cobra catheter, the left internal iliac artery was cannulated. The angiogram revealed an abnormal vascular blush and a pseudoaneurysm from branches of the superior vesical artery [Table/Fig-4]. Using a microcatheter, the left superior vesical artery was cannulated and embolised with 300-500 micron polyvinyl alcohol particles. The post-embolisation check angiogram revealed the absence of abnormal vascular blush, with no filling of the pseudoaneurysm, suggesting technical success of the procedure [Table/Fig-5].
Super selective left superior vesical artery Digital Subtraction Angiography (DSA) image showing its hypertrophied branches with pseudoaneurysm from one of the branches.
Post-embolisation super selective left superior vesical artery DSA image showing absence of pseudoaneurysm filling suggestive of successful embolisation.
Later, the left common femoral artery was cannulated, and the right internal iliac artery was catheterised. However, angiograms of the right internal iliac artery revealed no abnormal vascular blush or presence of pseudoaneurysm from the right superior or inferior vesical arteries. The haematuria reduced within 6-8 hours and stopped completely after 24 hours, which was confirmed on pelvic ultrasound [Table/Fig-6]. The patient experienced mild post-embolisation syndrome in the form of mild fever and suprapubic pain, for which medications were administered. The patient was discharged on the 5th postoperative day. After two weeks of follow-up, there was no haematuria, and a repeat cystoscopy revealed no ischaemic complications. The pelvic ultrasound also showed clear urine inside the lumen of the urinary bladder with no fresh blood clots.
Ultrasound image of the urinary bladder post 24 hours of embolisation showing no obvious blood clot inside the urinary bladder.
Discussion
Haemorrhagic cystitis is defined as a diffuse inflammation of the urinary bladder caused by infectious or non infectious factors, leading to bleeding from the bladder mucosa, which can be life-threatening in some cases [1]. The common cause of chronic haemorrhagic cystitis is radiation therapy for pelvic malignancies [1,2]. The reported incidence rate is approximately 3 to 15% [2]. The treatment modalities described in the literature for managing such cases include bladder irrigation, Hyperbaric Oxygen (HBO) therapy, intravesical instillation, fulguration, and surgical methods [3].
Pelvic malignancies, such as carcinoma of the endometrium and cervix, are commonly treated with external beam radiation. Among the late complications of pelvic radiation therapy is radiation cystitis, which can occur approximately 90 days after the initiation of radiation; however, a few cases have been reported beyond 10 years [4-7]. Radiation cystitis can be either acute or chronic. Acute radiation cystitis presents with urinary frequency, urgency, and dysuria. It is usually self-limiting and can last up to three months post-radiation [4-7]. Late radiation-induced haemorrhagic cystitis occurs six months to 20 years after radiation in about 6.5 to 10% of cases receiving radiation [4-7].
The main symptom of late radiation-induced haemorrhagic cystitis is haematuria [4]. It can range from mild and self-limiting to severe and life-threatening. Radiation leads to obliterative endarteritis of the bladder wall vessels, resulting in ischaemia and ulceration, which in turn leads to bleeding [4]. The primary finding on histopathology is microscopic progressive obliterative endarteritis. The bladder wall mucosa ulcerates due to ischaemia and begins to bleed. Simultaneously, neovascularity develops in the damaged areas. These new blood vessels are more fragile and can easily rupture with bladder distention, minor trauma, and irrigation. This process can lead to the formation of pseudoaneurysms in some patients [1].
In patients with haemorrhagic cystitis, initial measures include hemodynamic stabilisation and blood transfusion, followed by bladder irrigation [4,6]. Oral or intravesical drug therapy, fulguration, HBO therapy, vesical artery embolisation, or, rarely, cystectomy may be utilised [4-7]. Agents such as formaldehyde, silver nitrate, and carboprost have been instilled intravesically to stop bleeding [4]. HBO stimulates angiogenesis and fibroblast activity, aiding in the healing of the ulcerated mucosa; however, its long-term effectiveness is unknown, and availability in all centers is limited [4,6]. Cystoscopic fulguration of the bleeding points can effectively stop active bleeding [4,6]. Surgical treatments like urinary diversion or cystectomy are not commonly employed due to the associated high mortality and morbidity [6].
Transarterial superselective vesical artery embolisation has been utilised as primary therapy and in refractory cases of radiation-induced haemorrhagic cystitis [3-9]. Various case reports highlight the role of superselective vesical artery embolisation for haemorrhagic cystitis due to radiation, trauma, and malignancy [10,11]. Several studies in the literature indicate no major complications after superselective vesical artery embolisation with particles, glue, or a combination of both [12,13]. The present case underscores the role of transarterial superselective vesical artery embolisation in managing refractory haematuria due to radiation-induced haemorrhagic cystitis without any ischaemic complications. The preferred choice of Polyvinyl Alcohol (PVA) particles is 300-500 microns, as there is a lower risk of non targeted embolisation and tissue devascularisation [13]. When an active bleeding source or focal hypervascularity is identified, unilateral embolisation is usually sufficient, as in the above case; otherwise, a bilateral superselective approach is needed [12].
Conclusion(s)
There are numerous techniques for the treatment of radiation-induced haemorrhagic cystitis, but superselective embolisation of the vesical arteries is a suitable and efficient method for patients in whom other conventional modalities have failed to produce successful results.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 29, 2023
Manual Googling: Dec 07, 2023
iThenticate Software: Jan 10, 2024 (6%)
[1]. Manikandan R, Kumar S, Dorairajan LN, Hemorrhagic cystitis: A challenge to the urologistIndian J Urol 2010 26:159-66. [Google Scholar]
[2]. Nabi G, Sheikh N, Greene D, Marsh R, Therapeutic transcatheter arterial embolization in the management of intractable haemorrhage from pelvic urological malignancies: Preliminary experience and long-term follow-upBJU Int 2003 92:245-47. [Google Scholar]
[3]. Lee JE, Kwon JH, Bae J, Super-selective embolization of bilateral inferior vesical arteries for the management of radiation induced hemorrhagic cystitis refractory to conventional methodsIran J Radiol 2018 15:e64135 [Google Scholar]
[4]. Zwaans BM, Nicolai HG, Chancellor MB, Lamb LE, Challenges and opportunities in radiation-induced hemorrhagic cystitisRev Urol 2016 18:57-65. [Google Scholar]
[5]. Alesawi AM, El-Hakim A, Zorn KC, Saad F, Radiation-induced hemorrhagic cystitisCurr Opin Support Palliat Care 2014 8:235-40. [Google Scholar]
[6]. Smit SG, Heyns CF, Management of radiation cystitisNat Rev Urol 2010 7:206-14. [Google Scholar]
[7]. Crew JP, Jephcott CR, Reynard JM, Radiation-induced haemorrhagic cystitisEur Urol 2001 40:111-23. [Google Scholar]
[8]. Gowda GG, Vijayakumar R, Tigga MP, Endovascular management of radiation-induced hemorrhagic cystitisIndian J Palliat Care 2019 25(3):471-73.PMCID: PMC665953810.4103/IJPC.IJPC_6_1931413467 [Google Scholar] [CrossRef] [PubMed]
[9]. Loffroy R, Pottecher P, Cherblanc V, Favelier S, Estivalet L, Koutlidis N, Current role of transcatheter arterial embolization for bladder and prostate hemorrhageDiagn Interv Imaging 2014 95(11):1027-34.Epub 2014 Apr 1810.1016/j.diii.2014.03.00824746761 [Google Scholar] [CrossRef] [PubMed]
[10]. Cho CL, Lai MH, So HS, Kwok KK, Chan JC, Velayudhan V, Superselective embolisation of bilateral superior vesical arteries for management of haemorrhagic cystitisHong Kong Med J 2008 14:485-88. [Google Scholar]
[11]. De Berardinis E, Vicini P, Salvatori F, Sciarra A, Gentile V, Di Silverio F, Superselective embolization of bladder arteries in the treatment of intractable bladder haemorrhageInt J Urol 2005 12:503-05. [Google Scholar]
[12]. Delgal A, Cercueil JP, Koutlidis N, Michel F, Kermarrec I, Mourey E, Outcome of transcatheter arterial embolization for bladder and prostate hemorrhageJ Urol 2010 183(5):1947-53.Epub 2010 Mar 1910.1016/j.juro.2010.01.00320303518 [Google Scholar] [CrossRef] [PubMed]
[13]. Tsitskari M, Spiliopoulos S, Konstantos C, Palialexis K, Reppas L, Brountzos E, Long-term results of super-selective trans-catheter embolization of the vesical arteries for the treatment of intractable bladder haematuriaCVIR Endovasc 2020 3(1):97PMCID: PMC773289910.1186/s42155-020-00188-133306133 [Google Scholar] [CrossRef] [PubMed]