Osteochondral Fragment Fixation in Transient Patellar Dislocation of an Adolescent: A Case Report
Vishal S Patil1, Mohammed Talha Muneer2, Setu Kaneria3
1 Professor and Head, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Sant Tukaram Nagar, Pimpri, Pune, Maharashtra, India.
2 Chief Resident, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Sant Tukaram Nagar, Pimpri, Pune, Maharashtra, India.
3 Senior Resident, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Sant Tukaram Nagar, Pimpri, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohammed Talha Muneer, 702, 7th Floor, Shankeshwar Darshan, Nehru Nagar Chowk, Pimpri, Pune-411018, Maharashtra, India.
E-mail: talha.m1432@gmail.com
Osteochondral Fractures (OCFs) of the patella are common in adolescents due to ligament laxity and weak osteochondral junctions. OCFs following patellar dislocation are particularly challenging in this age group. Magnetic Resonance Imaging (MRI) aids in comprehensive evaluation, and surgical fixation with bioabsorbable sutures is a reliable treatment option. Early intervention and proper rehabilitation are essential to ensure optimal outcomes and prevent long-term complications. The present case report details the presentation, diagnosis, surgical intervention and outcome of a 16-year-old male with an OCF following patellar dislocation. Examination revealed significant ligament laxity and patellar hypermobility, along with patella alta (Insall-Salvati ratio of 2.1) on the affected side. The neurovascular examination was normal. Initial X-rays showed no abnormalities; however, Computed Tomography (CT) and MRI scans revealed a displaced OCF fragment in the anterior intercondylar region, along with lateral patellar tilt, marrow contusion, chondral delamination and partial thickness tearing of the Medial Patellofemoral Ligament (MPFL). Surgical intervention involved open reduction and internal fixation using absorbable Vicryl sutures. Postoperatively, the patient was immobilised for six weeks, followed by a structured rehabilitation program. The patient achieved a full range of motion and restored knee function within six months, with satisfactory radiographic and functional outcomes. At the latest follow-up, the knee range of motion was from 0 degrees of extension to 130 degrees of flexion, with complete pain alleviation. OCFs of the patella in adolescents require timely diagnosis and intervention to prevent degenerative changes. MRI is essential for evaluating soft tissue injuries. Surgical fixation using bioabsorbable sutures provides effective treatment, offering strong fixation without the need for implant removal. Addressing associated injuries, such as MPFL tears, is crucial to prevent recurrent dislocation.
Absorbable Implants, Articular, Knee dislocation, Ligaments
Case Report
A 16-year-old male presented with complaints of dislocating his knee while walking, along with pain during ambulation. Physical examination of the joint revealed significant ligament laxity, with normal alignment and no varus or valgus deformity. The patellar slide and glide were observed to be up to 2 quadrants on the unaffected joint and up to 3 quadrants on the affected side, indicating hypermobility of the patella on the affected side. An additional finding of patella alta (Insall-Salvati ratio of 2.1) was noted on the affected side.
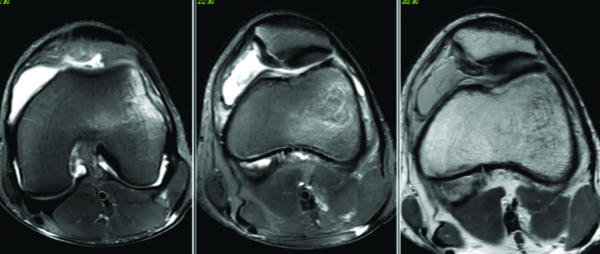
The neurovascular examination was non contributory. Anteroposterior (AP) and lateral roentgenograms of the left knee demonstrated no abnormalities [Table/Fig-1]. Furthermore, MRI and CT scans indicated a displaced OCF located in the anterior intercondylar region adjacent to the posterior border of Hoffa’s fat pad [Table/Fig-2,3]. Additionally, there was evidence of patella alta and small partial thickness tearing of the MPFL. An open reduction and internal fixation procedure was scheduled accordingly.
AP view and lateral view X-ray of left knee.

CT and 3D cuts of left knee showing displaced osteochondral fragment.
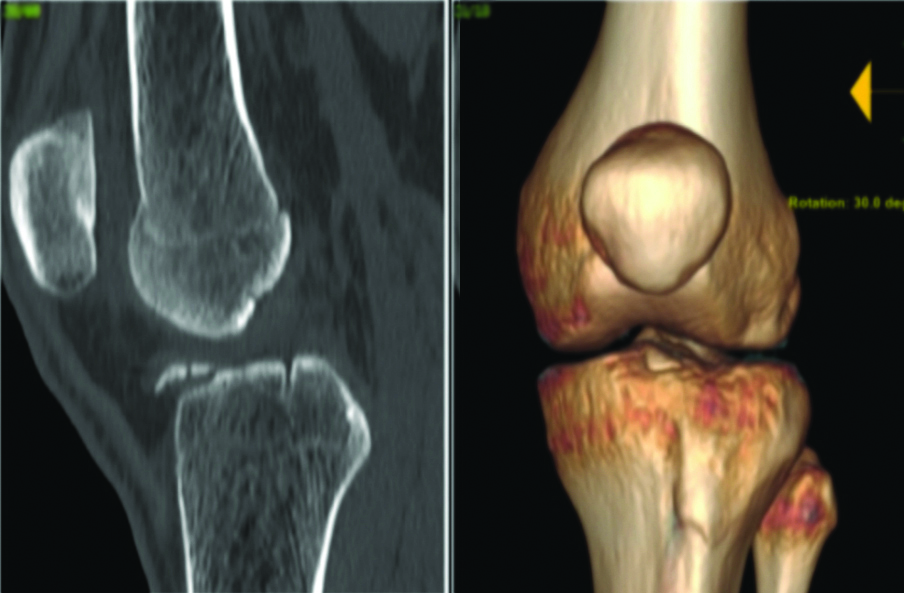
The X-ray report of the left knee indicated a normal joint space with an intact articular surface. The patella was reported to be normal, with no evidence of loose bodies. The MRI report revealed a complex array of issues affecting the patellofemoral joint. These include lateral patellar tilt and medial patellofemoral joint opening, as well as, marrow contusions on the medial patellar facet and the lateral non articular surface of the lateral femoral condyle. Chondral delamination was evident on the lower portions of the medial patellar facet and the median patellar ridge. Additionally, there was a displaced OCF fragment located in the anterior intercondylar region adjacent to Hoffa’s fat pad. The patient also exhibited Type C trochlear dysplasia per the Dejour classification [1] and patella alta. Partial thickness tears were noted in the MPFL and medial patellar retinaculum at their patellar insertions. Mild knee joint effusion was present. These findings underscore significant patellofemoral instability and associated chondral and osteochondral lesions, necessitating thorough assessment and tailored treatment planning.
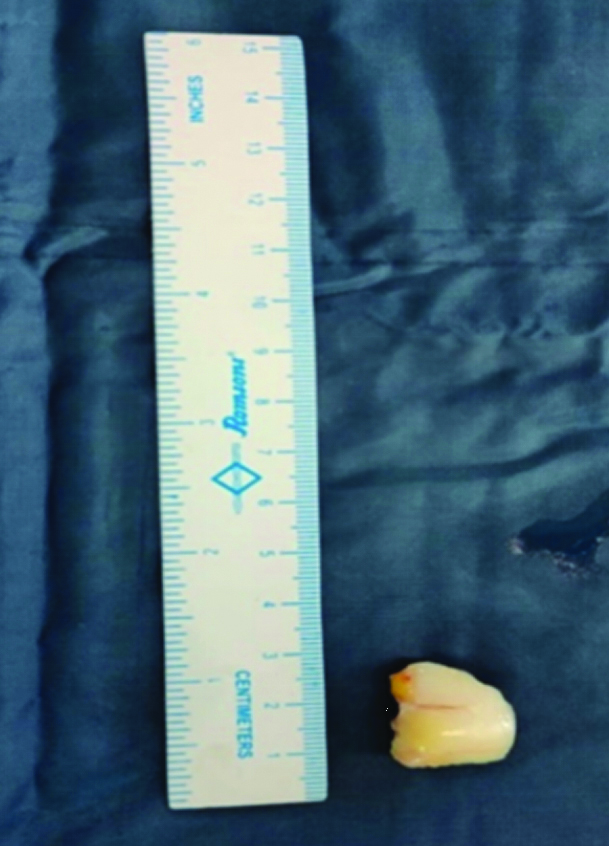
The procedure utilised a standard medial parapatellar approach, revealing an intact extensor mechanism. A substantial OCF fragment was identified and removed from the anterior intercondylar region [Table/Fig-4]. The loose body was affixed to the non articular region of the patella using absorbable Vicryl sutures [Table/Fig-5]. Postoperative AP and lateral X-rays were found to be acceptable. A medial imbrication procedure was performed by advancing the attachment of the quadriceps muscle over the patella. The osteosynthesis was assessed through meticulous flexion of the knee joint.
Osteochondral Fracture (OCF) fragment.
Fixation of the fracture fragment.

The patient underwent regular follow-up evaluations. Following the procedure, a long knee immobiliser was advised for six weeks, followed by active rehabilitation exercises to prevent quadriceps atrophy. The rehabilitation protocol included isometric quadriceps exercises during immobilisation, followed by progressive active quadriceps exercises with an increasing range of motion. Full range of motion and restoration of knee function were attained within six months. At subsequent follow-up appointments, satisfactory radiographic findings and functional outcomes were observed. The knee range of motion at the latest follow-up was from 0 degrees extension to 130 degrees flexion, with complete alleviation of pain.
Discussion
The OCF of the patella represents a prevalent condition encountered in orthopaedic surgery, occurring across all age groups [1]. Adolescents have been found to be more susceptible due to the generalised laxity of ligaments and a weak osteochondral junction biomechanically. Studies have indicated that the most common site of patellar OCF is the medial facet of the patella [2,3]. According to Seeley MA et al., patients with weight-bearing lateral femoral condyle injuries have lower short-term functional scores, indicating that the site of the injury affects the outcome [3].
In most cases, diagnostic confirmation can be achieved with AP and lateral knee radiographs [4]. Maintaining stability in the patellofemoral joint is paramount for avoiding premature knee osteoarthritis. Weber CD et al., proposed surgical intervention, specifically internal fixation, for any osteochondral flake fracture, advocating this approach for both paediatric and adult populations [5]. The fixation is usually performed in an acute setting (within two weeks) using internal fixation procedures with metal or bioabsorbable pins or compression screws through the fragment.
Metal devices require removal via a second surgery and can present mechanical issues, along with hardware prominence. In contrast, bioabsorbable devices do not require removal but may present tissue reactions, slow degradation and bone cyst formation. In first-time dislocators, along with the fixation of the fragment, it is necessary to adjuvantly repair the medial patellofemoral ligament, as it is usually torn or injured during a patellar dislocation.
Recurrent patellar dislocation can also be prevented by performing a medial imbrication procedure, which involves advancing the attachment of the quadriceps muscle over the patella, or by performing a Fulkerson procedure, which includes osteotomy along with anteromedialisation of the tibial tubercle, leading to elevation of the distal pole of the patella and reducing its contact with the knee joint during the early stages of flexion.
The authors requested computed tomography and MRI scans to gain a comprehensive understanding of the injury. The authors considered MRI to be a better imaging modality for evaluating the soft tissues of the knee. Several approaches have been reported in the literature for fixing OCF of the patella, each demonstrating success in various cases [6-9]. Several studies support the fixation of the fragment, which appears to be a logical treatment approach for a sizeable displaced osteochondral fragment [5,10]. Headless screws offer strong fixation and compression across the fracture fragment; however, they frequently necessitate subsequent surgery for removal. Suture-only techniques have been developed to circumvent the need for secondary implant removal and eliminate the use of metal screws [9]. Research has demonstrated that a suture-only technique provides sufficient fixation strength and is suitable for smaller osteochondral fragments that may not accommodate multiple screws [9]. One such study by Felus J et al., showed a 100% healing rate and satisfactory midterm clinical results obtained via suture fixation of Anteriorposterior Displaced (APD) related OCF in adolescents [11].
Diagnosing OCF in the knee poses challenges due to the vague nature of historical and clinical findings, compounded by the limited sensitivity of plain radiographs. Utilising MRI or arthroscopy becomes imperative to accurately pinpoint these fractures [12].
According to Alosaimi MN et al., medial arthrotomy was deemed the optimal surgical approach due to the osteochondral fragment’s location and the opportunity to visualise the MPFL [2]. Addressing patellar fragments through this approach was deemed appropriate.
Conclusion(s)
The OCFs following patellar dislocation are challenging to diagnose and treat, especially in adolescents due to their unique anatomical and biomechanical characteristics. Early and accurate diagnosis using advanced imaging techniques such as MRI is crucial for appropriate management. Surgical fixation with bioabsorbable sutures offers a reliable and effective treatment option, minimising the need for secondary procedures. Addressing associated injuries, such as MPFL tears, is essential to prevent recurrent dislocations and long-term complications. The present case demonstrates the successful use of bioabsorbable sutures in achieving stable fixation and excellent functional outcomes. Timely intervention and structured rehabilitation are key to restoring full knee function and preventing degenerative changes.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 03, 2024
Manual Googling: Jun 22, 2024
iThenticate Software: Aug 01, 2024 (10%)
[1]. Dejour H, Walch G, Nove-Josserand L, Guier CH, Factors of patellar instability: an anatomic radiographic studyKnee Surg Sports Traumatol Arthrosc 1994 2(1):19-26.10.1007/BF015526497584171 [Google Scholar] [CrossRef] [PubMed]
[2]. Alosaimi MN, Almutairi MM, Alshahrani SM, Alqahtani MN, Alghamdi AS, Osteochondral fracture of the patella without soft-tissue injury and with no dislocation: A case reportInt J Surg Case Rep 2021 78:48-53.10.1016/j.ijscr.2020.11.151 [Google Scholar] [CrossRef]
[3]. Seeley MA, Knesek M, Vanderhave KL, Osteochondral injury after acute patellar dislocation in children and adolescentsJ Pediatr Orthop 2013 33(5):511-18.10.1097/BPO.0b013e318288b7a0 [Google Scholar] [CrossRef]
[4]. Unal M, Tatari H, The largest osteochondral fracture of patella, case reportAustin J Orthopade Rheumatol 2014 1(1):01-02. [Google Scholar]
[5]. Weber CD, Migliorini F, Hildebrand F, Reconstruction of large osteochondral lesions in the knee: Focus on fixation techniquesLife (Basel) 2021 11(6):01-17.10.3390/life11060543 [Google Scholar] [CrossRef]
[6]. Dines JS, Fealy S, Potter HG, Warren RF, Outcomes of osteochondral lesions of the knee repaired with a bioabsorbable deviceArthroscopy 2008 24(1):62-68. [Google Scholar]
[7]. Millington KL, Shah JP, Dahm DL, Levy BA, Stuart MJ, Bioabsorbable fixation of unstable osteochondritis dissecans lesionsAm J Sports Med 2010 38(10):2065-70. [Google Scholar]
[8]. Anderson CN, Magnussen RA, Block JJ, Anderson AF, Spindler KP, Operative fixation of chondral loose bodies in osteochondritis dissecans in the knee: A report of 5 casesOrthop J Sports Med 2013 1(2):2325967113496546 [Google Scholar]
[9]. Min Ng W, Mohamed Al-Fayyadh ZM, Kho J, Hui TS, Mohamed Ali RB, Crossing suture technique for the osteochondral fractures repair of patellaArthrosc Tech 2017 6(4):e1035-39. [Google Scholar]
[10]. Bhatt J, Montalban ASC, Wang KH, Lee HD, Nha KW, Isolated osteochondral fracture of the patella without patellar dislocationOrthopedics 2011 34(1):5410.3928/01477447-20101123-20 [Google Scholar] [CrossRef]
[11]. Felus J, Kowalczyk B, Starmach M, Wyrobek L, Osteochondral fractures in acute patellar dislocations in adolescents: Midterm results of surgical treatmentOrthop J Sports Med 2022 10(7):01-09. [Google Scholar]
[12]. Jalan D, Morey VM, Mittal R, Pannu CD, Transient patellar dislocation resulting in simultaneous osteochondral fractures of patella and lateral femoral condyle- A case reportJ Clin Diagn Res 2014 8(10):LD04-06. [Google Scholar]