Non Operative Management of Complicated Appendicitis with Broad Spectrum Antibiotics in a Paediatric Patient: A Case Report
Vansh Vohra1, Jyoti Jain2, Dipesh Goel3, Shaik Kareemulla4, Wandeep Dagar5
1 Student Pharm D, Department of Pharmacy Practice, Maharishi Markandeshwar College of Pharmacy (Deemed to be University), Ambala, Haryana, India.
2 Student Pharm D, Department of Pharmacy Practice, Maharishi Markandeshwar College of Pharmacy (Deemed to be University), Ambala, Haryana, India.
3 Associate Professor, Department of Paediatrics, Maharishi Markandeshwar College of Pharmacy (Deemed to be University), Ambala, Haryana, India.
4 Associate Professor, Department of Pharmacy Practice, Maharishi Markandeshwar College of Pharmacy (Deemed to be University), Ambala, Haryana, India.
5 Clinical Pharmacist and Assistant Professor, Department of Pharmacy Practice, Maharishi Markandeshwar College of Pharmacy (Deemed to be University), Ambala, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Wandeep Dagar, MM College of Pharmacy, MM (Deemed to be University), Mullana, Ambala-133207, Haryana, India.
E-mail: wandeep100@gmail.com; vanshvohra7300@gmail.com
The therapy for complicated appendicitis presents a clinical challenge, as it is characterised by inflammation with a contained or localised perforation that results in the formation of an abscess. This case report describes the presentation, diagnosis, and effective non operative management of a 14-year-old girl with acute complex appendicitis. Investigations and clinical examination confirmed the presence of an appendicular abscess in the patient, who exhibited characteristic symptoms. The treatment course adhered to the Ochsner-Sherren protocol, which included fluid resuscitation, broad-spectrum intravenous antibiotics, and a Nil Per Oral (NPO) status. An ultrasound-guided aspiration of periappendicular pus indicated that an empirical upgrade to Piperacillin+Tazobactam was necessary. The patient showed improvement in all symptoms, including fever and abscess resolution, after the switch in antibiotics. This case adds to the increasing body of research that supports non operative therapy for complex appendicitis, particularly when assisted by diagnostic tools such as ultrasonography. The decision to forego emergency surgery aligns with current evidence advocating for conservative strategies, which demonstrate higher success rates and lower risks of postoperative complications. Although appendectomy remains the preferred treatment for perforated appendicitis without an abscess, this case highlights the viability and effectiveness of non operative interventions in certain situations. This report emphasises the significance of customised treatment strategies based on patient presentation and clinical response, contributing to the ongoing discussion regarding the best therapy for complex appendicitis.
Ochsner-Sherren regimen, Piperacillin-tazobactam, Surgery, Vermiform appendix
Case Report
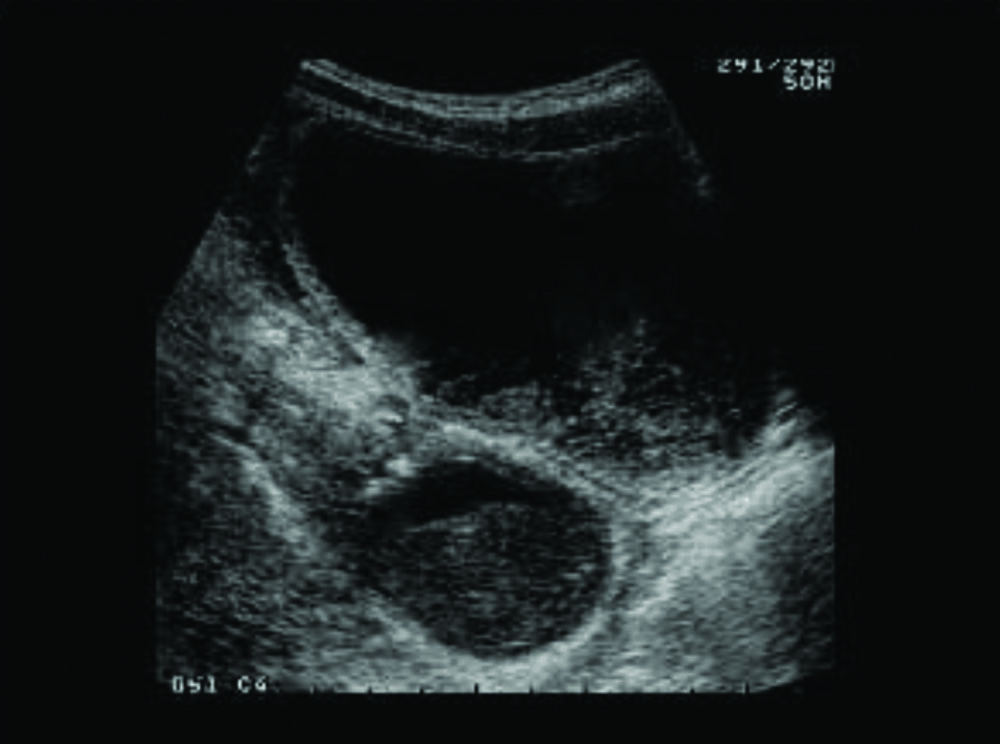
A 14-year-old girl arrived at the paediatric surgery department complaining of severe abdominal pain that had been present for 4-5 days, along with frequent episodes of nausea, vomiting, and occasional diarrhoea that lasted for 1-2 days. During the clinical examination, signs of pain were noted in the right iliac fossa, and a 4×3 cm mass was palpated in that area. The surgeon suspected that acute appendicitis might be the cause. Following a clinical assessment, he ordered an ultrasound and blood tests. The patient’s total leukocyte count was determined to be 18.44×103/cumm during the evaluation, and the ultrasound suggested that the patient may have an appendicular abscess (complicated appendicitis) [Table/Fig-1].
Ultrasound of the patient showing appendicular abscess.
The Ochsner-Sherren regimen was initiated for the patient. She was kept NPO. Intravenous (IV) antibiotics were started: PCM 750 mg TDS, Paracetamol 20 mg BD, Amikacin 750 mg OD, Ceftriaxone 1 gm BD, and Metronidazole 400 mg TDS. IV fluids (Dextrose Normal Saline at 80-100 mL/hour) were also started for the patient. She continued to have a high-grade fever for the next three days, and her total leukocyte count increased to 22,000/cumm.
Subsequently, periappendicular pus was aspirated under ultrasound guidance and sent for culture sensitivity. The patient was found to be sensitive to piperacillin and tazobactam. Piperacillin + Tazobactam 4.5 gm TDS was administered as an empirically improved version of ceftriaxone. The patient responded favourably to the prescribed treatment. Her temperature decreased, and the mass in her appendix resolved. She was transitioned to an oral diet, which she accepted successfully, and she had regular bowel movements. For the next two days, she exhibited no symptoms.
On day eight of her hospital stay, she was discharged with a prescription for antibiotics (Tab Oflox OZ BD), an antacid (Tab Pantop 20 mg), a pain reliever (Tab Meftal Spas SOS), and Paracetamol (Tab PCM SOS). Her follow-up appointments were scheduled regularly, and she continued to respond well to the treatment.
Discussion
An infection of the vermiform appendix complicated by a confined or limited perforation, resulting in an appendiceal abscess or mass growth, is known as complicated appendicitis [1]. It usually appears suddenly within 24 hours of onset, though it can also manifest as a more persistent illness. Initially, it presents as periumbilical or generalised abdominal pain and subsequently migrates to the lower right quadrant [2]. Severe appendicitis may necessitate immediate surgery or conservative therapy, depending on the patient’s condition and the healthcare provider’s assessment [1].
Research highlights the effectiveness of broad-spectrum antibiotics in treating complicated appendicitis, which reduces the likelihood of abscess development and postoperative sequelae [3-5]. In the present case, the patient recovered favourably after switching to antibiotics, with the fever and appendiceal abscess resolving. Oral diet tolerability, regular bowel movements, and overall improvement in symptoms were noted; these findings are consistent with studies supporting the use of broad-spectrum antibiotics in cases of complicated appendicitis [5,6].
A recent meta-analysis by Vaos G et al., showed that the rates of complications and wound infections are significantly reduced in patients treated conservatively [7]. The treatment plan in the present study aligns with research supporting conservative approaches in managing severe appendicitis, demonstrating that appendiceal abscesses can be successfully managed without requiring emergency surgery [1]. Gavriilidis P et al., concluded that conservative approaches are favoured over acute appendicitis resection for managing complicated appendicitis [8].
Although appendectomy has long been considered the most effective treatment for acute appendicitis, new research indicates that there may be other viable options. The discovery that conservative management is effective, challenges the conventional wisdom [9]. While there are differences in quality, research on the conservative management of appendicitis generally agrees on the proportion of patients who respond well to treatment [10].
The risk of perforation in paediatric appendicitis underscores the need for appropriate management strategies to avert complications, highlighting the importance of the intervention [11].
Conclusion(s)
Although appendectomy has long been considered the gold standard for treating acute appendicitis, this case adds to the growing body of evidence that challenges this notion. This paediatric patient’s choice to pursue non operative therapy was consistent with research highlighting the efficacy of conservative management in specific situations, especially in the context of appendicular abscesses. Ultimately, this case significantly enhances One’s understanding of complex appendicitis therapy and supports the idea that successful outcomes can be achieved with a well-thought-out, conservative strategy that does not require immediate surgical intervention.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 15, 2024
Manual Googling: Mar 06, 2024
iThenticate Software: Jul 15, 2024 (4%)
[1]. Coccolini F, Fugazzola P, Sartelli M, Cicuttin E, Sibilla MG, Leandro G, Conservative treatment of acute appendicitisActa Biomed 2018 89(9-S):119-34.PMCID: PMC650219610.23750/abm.v89i9-S.790530561405 [Google Scholar] [CrossRef] [PubMed]
[2]. Bouchard ME, Slidell MB, Jones BA, AppendicitisTextbook of Paediatric Gastroenterology, Hepatology and Nutrition: A Comprehensive Guide to Practice 2023 2:673-80.10.1007/978-3-030-80068-0_49 [Google Scholar] [CrossRef]
[3]. Roque FMCB, Melo Filho AA, Roque AJCB, Roque HCB, Moreira TMM, Chaves EMC, Antibiotics for appendicectomy in children and adolescents during the perioperative period: An integrative reviewRev Paul Paediatr 2019 37(4):494-502.PMCID: PMC682148310.1590/1984-0462/;2019;37;4;0001331291445 [Google Scholar] [CrossRef] [PubMed]
[4]. Zavras N, Vaos G, Management of complicated acute appendicitis in children: Still an existing controversyWorld J Gastrointest Surg 2020 12(4):129-37.PMCID: PMC721597010.4240/wjgs.v12.i4.12932426092 [Google Scholar] [CrossRef] [PubMed]
[5]. Ong CP, Chan TK, Chui CH, Jacobsen AS, Antibiotics and postoperative abscesses in complicated appendicitis: Is there any association?Singapore Med J 2008 49(8):615-18.18756343 [Google Scholar] [PubMed]
[6]. Talan DA, Saltzman DJ, DeUgarte DA, Moran GJ, Methods of conservative antibiotic treatment of acute uncomplicated appendicitis: A systematic reviewJ Trauma Acute Care Surg 2019 86(4):722-36.PMCID: PMC643708410.1097/TA.000000000000213730516592 [Google Scholar] [CrossRef] [PubMed]
[7]. Vaos G, Dimopoulou A, Gkioka E, Zavras N, Immediate surgery or conservative treatment for complicated acute appendicitis in children? A meta-analysisJ Paediatr Surg 2019 54(7):1365-71.10.1016/j.jpedsurg.2018.07.017 [Google Scholar] [CrossRef]
[8]. Gavriilidis P, de’Angelis N, Katsanos K, Di Saverio S, Acute appendicectomy or conservative treatment for complicated appendicitis (phlegmon or abscess)? A systematic review by updated traditional and cumulative meta-analysisJ Clin Med Res 2019 11(1):56-64.Epub 2018 Dec 3. PMCID: PMC630613810.14740/jocmr367230627279 [Google Scholar] [CrossRef] [PubMed]
[9]. Suwanwongse K, Shabarek N, Successful conservative management of acute appendicitis in a Coronavirus Disease 2019 (COVID-19) patientCureus 2020 12(4):e7834PMCID: PMC725052110.7759/cureus.783432467809 [Google Scholar] [CrossRef] [PubMed]
[10]. Wojciechowicz KH, Hoffkamp HJ, van Hulst RA, Conservative treatment of acute appendicitis: An overviewInt Marit Health 2010 62(4):265-72.21348022 [Google Scholar] [PubMed]
[11]. Howell EC, Dubina ED, Lee SL, Perforation risk in paediatric appendicitis: Assessment and managementPaediatric Health Med Ther 2018 9:135-45.PMCID: PMC620907610.2147/PHMT.S15530230464677 [Google Scholar] [CrossRef] [PubMed]