Images in Medicine Representing the Management of Mesiodens in Different Dentitions
Simron Baishya1, Aishwarya V Antala2, Anshula Deshpande3, Seema Bargale4
1 Postgraduate Student, Department of Paediatric and Preventive Dentistry, KM Shah Dental College and Hospital, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
2 Postgraduate Student, Department of Paediatric and Preventive Dentistry, KM Shah Dental College and Hospital, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
3 Professor, Department of Paediatric and Preventive Dentistry, KM Shah Dental College and Hospital, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
4 Professor, Department of Paediatric and Preventive Dentistry, KM Shah Dental College and Hospital, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anshula Deshpande, Professor, Department of Paediatric and Preventive Dentistry, KM Shah Dental College and Hospital, Sumandeep Vidyapeeth Deemed to be University, Waghodia Road, Piparia, Taluk Waghodia, Vadodara-391760, Gujarat, India.
E-mail: dranshula@gmail.com
Dentition, Diastema, Malocclusion, Supernumerary, Tooth
Mesiodens are the most common type of supernumerary teeth, typically located between the two maxillary central incisors [1]. Hereby, three cases of mesiodens in primary, mixed and permanent dentition are presented, along with a discussion of how the complexity of treatment varies according to the stage of dentition.
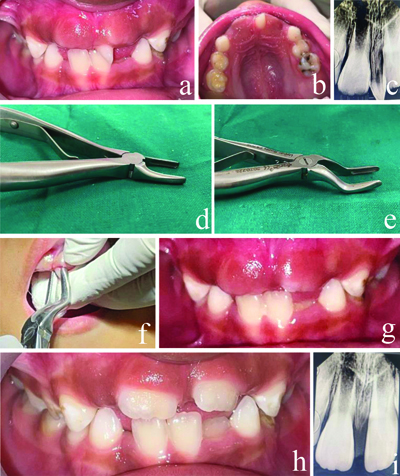
Case 1
A five-year-old female patient reported with the chief complaint of missing teeth in the upper front tooth region. There was no relevant medical or family history. On clinical examination she had a conical-shaped supernumerary tooth, with clinical absentia of both primary maxillary central incisors [Table/Fig-1a,b]. For radiographic examiantion, Intraoral Periapical Radiograph (IOPA) was taken which showed a conical-shaped single-rooted mesiodens [Table/Fig-1c]. On first appointment, diagnostic impressions were taken. On next appointment, the extraction of the mesiodens was done. The shape of the mesiodens posed a challenge to the dental operator, as grip of forceps on the crown during extraction was difficult using normal incisor forceps. Extraction was done using pedo-sized maxillary root forceps, which have a thinner beak that helped in firmer grasp on the tooth crown [Table/Fig-1d,e]. The movement for extraction was 45° rotation and pull, so as to prevent harm to the permanent tooth germs present very close to the tooth to be extracted [Table/Fig-1f]. Succeessful extraction of the supernumerary tooth was carried out without any harm to the permanent tooth germs of the central incisors. The patient was kept on follow-up [Table/Fig-1g] and at the one-month follow-up, the eruption of the permanent maxillary central incisors were seen in the oral cavity [Table/Fig-1h,i]. The extraction was necessary as the mesiodens was hindering the eruption of the permanent central incisors. No further treatment was required, as the central incisors began erupting in their normal position within one month.
a) Preoperative frontal view; b) Preoperative maxillary arch; c) Preoperative IOPA; d) Pedo-sized incisor forceps; e) Pedo-sized root forceps; f) Rotation and pull movement for extraction; g) Post-extraction one week follow-up frontal view; h) Postoperative 1 month follow-up frontal view; i) Postoperative 1 month follow-up IOPA.
Case 2
A nine-year-old female patient reported with the chief complaint of extra teeth in the upper front tooth region. There was no relevant medical or family history. On clinical examination, she had a conical-shaped supernumerary tooth [Table/Fig-2a]. Radiographic examination {IOPA and Orthopantomogram (OPG)} revealed a conical-shaped, single-rooted tooth between 11 and 21 [Table/Fig-2b,c], leading to the diagnosis of mesiodens. Furthermore, due to presence of the mesiodens, labial inclination of the central incisors could be seen. So the extraction, followed by diastema closure and alignment, was planned.
a) Frontal view of mesiodens; b) IOPA of mesiodens; c) Preoperative OPG; d) Immediate postextraction of mesiodens; e) Hawleys’s plate with finger spring delivered; f) Post diastema closure frontal view; g) Post diastema closure OPG.
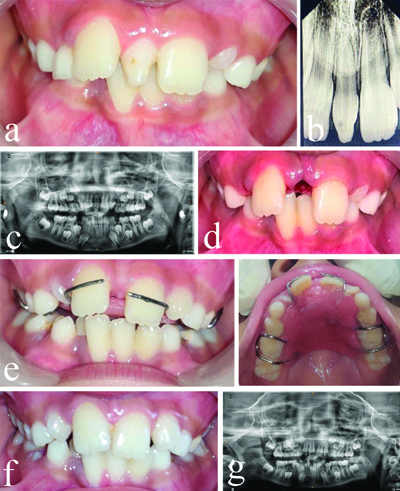
During the first appointment, impressions were taken, followed by the extraction of the mesiodens, which was the patient’s chief complaint. The extraction should be performed atraumatically to avoid any complication and should not hamper the root development, and hence forceps used for extraction was thin-beaked, pedo-sized maxillary root forceps, with only 45° rotation and a pulling motion. The extraction was carried out atraumatically with no harm to the adjacent permanent teeth and healing was achieved within a week [Table/Fig-2d].
On next appointment, another impression was taken and a removable Hawley’s plate with finger springs in positions 11 and 21 was delivered [Table/Fig-2e]. After four days, the finger springs were activated, leading to the closure of a 5 mm diastema within 15 days [Table/Fig-2f,g]. The outcome was quick and satisfactory for both the patient and her parents. The removable Hawley’s appliance was given to the patient for the retention of the diastema closure.
In early mixed dentition, mild orthodontic correction might be required. In the present case, since the root formation of the adjacent permanent incisors were not complete, fixed orthodontic therapy could arrest the root completion due to heavy orthodontic forces while removable appliance provide light, interrupted forces, thus it does not hinder in the root completion [2]. So, removable appliance with finger springs was used for diastema closure.
Case 3
A 14-year-old female patient reported with the chief complaint of malaligned teeth. There was no family history of mesiodens and no relevant medical history was found. On clinical examination there was a conical type of supernumerary tooth present between both maxillary central incisors [Table/Fig-3a]. Slight distal rotation of 21 could also be seen. IOPA was taken and single conical root could be seen and diagnosis of mesiodens was made [Table/Fig-3b]. Diagnostic impressions were taken and model analysis was done. After explaining the procedure and obtaining consent, extraction of the mesiodens was carried out [Table/Fig-3c,d]. The mesiodens was in close proximity to the adjacent central incisors, so pedo-sized maxillary root forceps were used for the extraction, using 45° rotation and pulling movement.
a) Preoperative frontal view; b) Preoperative IOPA; c) Post-extraction maxillary arch; d) Extracted tooth specimen; e) Fixed orthodontic treatment using 2*4; f) Post-treatment frontal view.
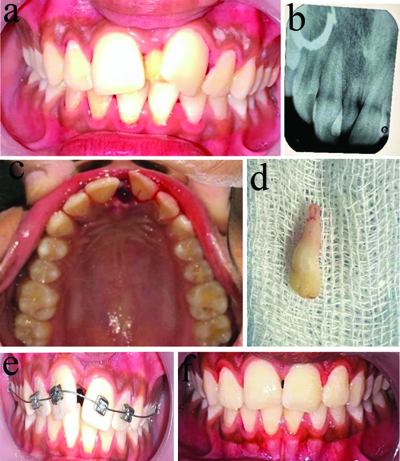
The patient had Angle’s Class I molar relation bilaterally, with no other malocclusion, so only correction of the midline diastema was required. This was achieved using a 2×4 fixed orthodontic appliance [Table/Fig-3e]. Bracket placement was followed by the ligation of 0.014 and 0.016 Nickel-Titanium (NiTi) wires. Closure of the 4 mm diastema of 4 mm was achieved within six months [Table/Fig-3f]. A post-treatment orthodontic retainer was given. In late mixed and complete permanent dentition, fixed orthodontic treatment is the treatment of choice [3]. In permanent dentition, the roots of adjacent permanent maxillary central incisors are completely formed, allowing for complete diastema closure along with alignment to be achieved within six months as in the present case.
The treatment protocol for mesiodens varies based on the type of dentition and eruption status. In the present case series, Case 1 required only extraction, while Cases 2 and 3 involved extraction followed by closure of the diastema. Alsuwaida MM reported a case of a 10-year-old girl with an erupted mesiodens that was extracted immediately, followed by regular monitoring to ensure proper alignment of the permanent incisors as they continued to erupt [4]. This study suggested that erupted mesiodens should be extracted to prevent crowding and displacement of the permanent incisors. Similarly, Bhatara S et al., recommended in a case series that mesiodens present in permanent dentition should be extracted and followed by fixed orthodontic therapy [3].
Conclusion(s)
The treatment of choice for a mesiodens is extraction as early as it is diagnosed. Early treatment would lead to prevent malocclusion, while delayed treatment would require more complex interventions. As a person ages and their occlusion becomes established, the closure of a post-extraction diastema becomes more complicated.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 21, 2024
Manual Googling: Jul 06, 2024
iThenticate Software: Aug 05, 2024 (14%)
[1]. He D, Mei L, Wang Y, Li J, Li H, Association between maxillary anterior supernumerary teeth and impacted incisors in mixed dentitionJ Am Dent Assoc 2017 148(8):595-603.10.1016/j.adaj.2017.05.01728754185 [Google Scholar] [CrossRef] [PubMed]
[2]. Augustine R, Babaji P, Kamalaksharappa SK, Management of mesiodens in mixed dentition-molariform and tuberculate: A case reportInterventions in Pediatric Dentistry: Open Access Journal 2019 2(4)Lupine Publishers, LLC:161-64. [Google Scholar]
[3]. Bhatara S, Goswami M, Shivangani Rahman B, Gogoi A, Double mesiodens in the mixed dentition of non-syndromic north-Indian patients: A case seriesCureus 2024 16(2):e54161PMCID: PMC1094808710.7759/cureus.5416138500940 [Google Scholar] [CrossRef] [PubMed]
[4]. Alsuwaida MM, A supernumerary tooth: A case report of a mesiodensInt J Case Rep Images 2023 14(2):115-17. [Google Scholar]