Optimal Anaesthetic Management in Tracheal Reconstruction Surgery: The Role of High-frequency Jet Ventilation
Tanmay Chaudhari1, Shweta Khatri2
1 Assistant Professor, Department of Ear, Nose and Throat, Dr. D. Y. Patil Medical College, Hospital and Research Centre. Dr. D.Y. Patil Vidyapeeth (Deemed to be University), Pune, Maharashtra, India.
2 Assistant Professor, Department of Anaesthesia, Dr. D. Y. Patil Medical College, Hospital and Research Centre. Dr. D.Y. Patil Vidyapeeth (Deemed to be University), Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Shweta Khatri, House No: D1-702, Gangaskies Housing Society, Pimpri, Pune-411018, Maharashtra, India.
E-mail: dr.shwetakhatri@gmail.com
Cardiopulmonary bypass, Mechanical ventilation, Tracheal resection
Dear Editor,
Anaesthesia for tracheal resection and reconstruction presents a significant challenge due to the compromised airway and the necessity of sharing the airway with the surgeon while ensuring that respiratory function is maintained [1,2]. Tracheal resection and reconstruction are the primary palliative or curative treatments for severe airway obstruction [3]. These surgical interventions have the potential to increase the 5-year survival rates from 5-47% [4]. Successful management of such cases requires innovative approaches to ensure adequate ventilation and oxygenation while allowing the surgeon to perform intricate procedures. Although there are several airway techniques to manage this critical phase, each with its own limitations, no controlled randomised trials have demonstrated the superiority of one method over another [4].
Various anaesthetic techniques have been employed in these surgeries, with some notable methods highlighted. The conventional approach involves general anaesthesia with endotracheal intubation and cross-field ventilation. However, mechanical ventilation in this method can limit surgical exposure due to the presence of the endotracheal tube. Another option is Cardiopulmonary Bypass (CPB) and extracorporeal oxygenation, which provide optimal exposure of the surgical site and haemodynamic support. Despite its advantages, this method is limited by its high cost and limited availability [4]. Jet ventilation is a specialised form of mechanical ventilation that uses a high-frequency, low-volume technique to deliver oxygen and remove carbon dioxide. Using a fine-bore catheter for jet ventilation allows the procedure to be less invasive and minimises interference with surgical procedures [5]. Jet ventilation, which can be either high-frequency or low-frequency, offers excellent exposure of the surgical field but comes with the risks of barotrauma and difficulties in monitoring ventilation [4].
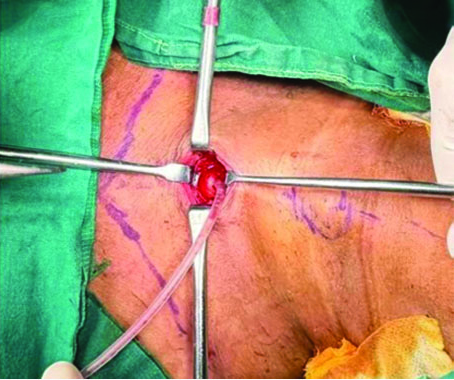
This letter discusses the use of High-frequency Jet Ventilation (HFJV) with a 10 Fr catheter, along with intravenous anaesthesia combined with muscle relaxation, in a patient with a history of tracheal stenosis [Table/Fig-1] due to endotracheal intubation performed for organophosphate poisoning. The patient presented with dyspnoea and hoarseness of voice, necessitating an emergency tracheostomy [Table/Fig-2]. Following the relief of these symptoms, she was scheduled for tracheal resection and reconstruction. The anaesthetic management for this surgery was unique, particularly in the preoperative assessment and induction planning, with a specific focus on coordinating airway sharing with the surgeon.
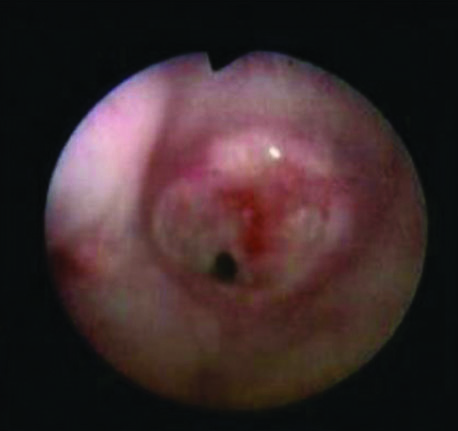

A 19-year-old female patient with a tracheostomy, diagnosed with severe subglottic stenosis and a granuloma in the lumen, was scheduled for tracheal reconstruction surgery. A thorough pre-anaesthetic evaluation was conducted, confirming the patient’s fitness for surgery. Routine laboratory investigations, arterial blood gas analysis and a 2 Dimensional (2D) echocardiogram were all within normal limits. All standard American Society of Anaesthesiologists (ASA) monitors, including the End-tidal Carbon Dioxide (ETCO2) monitor, were attached.
The patient was premedicated with fentanyl (1 μg/kg). Induction was performed with intravenous propofol at 2 mg/kg, followed by intubation with a cuffed 5.5 mm Endotracheal (ET) tube through the tracheostomised opening, ensuring that the tube passed below the stenosed tracheal segment without difficulty. Atracurium (0.5 mg/kg) was administered for muscle relaxation. Maintenance of anaesthesia was achieved with inhalational sevoflurane and nitrous oxide. An intravenous infusion of dexmedetomidine at 1 μg/kg was started for analgesia.
Ventilation was initially performed using a 5.5 mm endotracheal tube. The tidal volume was set to 400 mL at a rate of 16 breaths per minute, and ETCO2 was monitored with a capnograph. This ventilation set-up was maintained until the stenosed segment was dilated. After the endotracheal tube was removed, a cuffed flexometallic tube size 7.0 was passed through the tracheostomy opening, and ventilation was continued until the resection of the stenosed segment of the trachea was completed.
For the reconstruction with anastomosis of the upper and lower tracheal segments, HFJV was initiated. A number 10 catheter was connected to the jet ventilation unit [Table/Fig-3] and passed through a tracheostomy opening, delivering 100% oxygen at a rate of 50-60 breaths per minute. Auscultation was performed on both lungs to ensure equal air entry, and the catheter tip was positioned just above the carina [Table/Fig-4].
Catheter attachment to jet ventilator unit.

Catheter’s passage through the tracheal opening.
The intravenous propofol drip was maintained throughout the procedure to ensure sedation. Continuous monitoring was performed for any trickling blood in the lower segment. Intermittent serial arterial blood gases were checked. This technique facilitates controlled tracheal mobilisation, resection and reconstruction around the tube while maintaining continuous ventilation and oxygenation.
At the end of the anastomosis, the catheter was removed. Simultaneously, a No. 7 flexometallic tube was passed orally, and anaesthesia was continued with oxygen, nitrous oxide and sevoflurane using Intermittent Positive Pressure Ventilation (IPPV). The anterior anastomosis of the trachea and skin closure were then performed. The patient was successfully extubated after reversal and was discharged on postoperative day 8.
The HFJV works by delivering short bursts (jets) of high-pressure gas to the airway at high frequencies. The small, rapid jets are delivered through a specialised catheter, and expiration occurs passively near the wall of the airway cross-section [4]. To maintain proper gas exchange in patients, adjustments can be made to the respiratory rate, driving pressure, oxygen concentration and inspiration time according to the patient’s needs, and all these parameters must be closely monitored [6].
In conclusion, the use of HFJV, when paired with careful monitoring, offers adequate ventilation and effective surgical access during tracheal surgery.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 21, 2024
Manual Googling: Sep 12, 2024
iThenticate Software: Sep 27, 2024
[1]. Hobai IA, Chhangani SV, Alfille PH, Anaesthesia for tracheal resection and reconstructionAnaesthesiol Clin 2012 30(4):709-30.10.1016/j.anclin.2012.08.01223089505 [Google Scholar] [CrossRef] [PubMed]
[2]. Parab SY, Humane S, Pai P, Karimundackal G, Anaesthesia management of ‘tubeless’ tracheal resectionIndian J Anaesth 2022 66(6):471-72. [Google Scholar]
[3]. Liu X, Jiang R, Xiao J, Lu T, Gan J, Cheng J, Anaesthesia airway management for tracheal resection and reconstruction: A single-center case seriesAnn Palliat Med 2021 10(3):3354-63. [Google Scholar]
[4]. Marwaha A, Kumar A, Sharma S, Sood J, Anaesthesia for tracheal resection and anastomosisJ Anaesthesiol Clin Pharmacol 2022 38(1):48-57. [Google Scholar]
[5]. Putz L, Mayné A, Dincq AS, Jet ventilation during rigid bronchoscopy in adults: A focused reviewBiomed Res Int 2016 2016:4234861 [Google Scholar]
[6]. Fritzsche K, Osmers A, Anaesthetic management in laryngotracheal surgery. High-frequency jet ventilation as strategy for ventilation during general anaesthesiaAnaesthesist 2010 59(11):1051-61.quiz 1062-3 [Google Scholar]