CNBs, which include spinal (subarachnoid) and epidural blocks, are commonly performed for a wide variety of surgeries. Both types of blocks can be administered as a single injection or with an indwelling catheter to allow for intermittent boluses or continuous infusions. For a central neuraxial block, the needle is inserted through the interspinous space between two spinous processes. It passes through the skin, subcutaneous tissues, supraspinous ligament, interspinous ligament, ligamentum flavum, and dura, ultimately entering the subarachnoid space, as indicated by the free-flowing clear cerebrospinal fluid [1]. An epidural block can be performed at lumbar, thoracic, or cervical levels. Epidural techniques are widely used for operative anaesthesia, obstetric analgesia, postoperative pain control, and pain management in patients with chronic pain [2]. Combined Spinal Epidural (CSE) anaesthesia offers complete sensory and motor blockade, a longer duration of surgical anaesthesia, excellent postoperative pain control, and a reduction in the incidence of postoperative pulmonary morbidity [3]. Sequential CSE anaesthesia is a safe, effective, and reliable technique. It provides stable haemodynamics along with prolonged postoperative analgesia compared to spinal anaesthesia alone for high-risk geriatric patients undergoing major orthopaedic lower limb surgery [4].
Performing neuraxial anaesthesia is not always easy, especially in geriatric orthopaedic patients. Anatomical abnormalities such as spinal canal stenosis, scoliosis, and narrowing of interspinous spaces contribute to the difficulties faced by anaesthesiologists while performing these procedures [5]. Scoliosis is a complex deformity of the vertebral spine, resulting in lateral curvature and rotation of the vertebral body. In such cases, a needle puncture perpendicular to the skin plane can direct the needle toward the lateral part of the dural sac, which can cause paraesthesia and difficulty in performing the block. Recently, ultrasonography has proven to be quite useful in challenging neuraxial blocks; however, it requires advanced imaging facilities and the expertise of anaesthesiologists, which are not available everywhere [6]. Therefore, in such cases, lumbosacral spine X-rays can be helpful in identifying the angle and plane of entry for the spinal and epidural needle [7]. Multiple punctures are associated with increased pain, discomfort, and dissatisfaction for the patient [8]. They also lead to wasted time, embarrassment, and a decrease in the morale of the anaesthesiologist. Traumatic placement of the needle during the neuraxial block procedure can cause complications, such as vasovagal attacks and postdural puncture headaches. In severe cases, trauma to neural structures or a spinal haematoma can result in permanent neurological damage and long-term disability for patients [9]. Preoperative X-rays of the lumbar spine, both anteroposterior and lateral views, facilitate neuraxial block procedures in patients scheduled for knee or hip replacement surgeries who have had previous lumbar spine surgeries [10]. Lumbar spine X-rays help in identifying a clearer access route for the passage of the needle, providing some degree of guidance in an otherwise blind procedure. Preoperative prediction of difficulty enhances the quality of care by making block procedures easier and more comfortable for patients [11].
In the current study, authors developed a difficulty predictor score (MUSG Score, which stands for Minnu, Usha, Shilpa, and Gurleen) based on the findings from preoperative X-rays of the lumbosacral spine in patients who were undergoing lower limb arthroplasty surgeries.
The study aimed to assess the role of the difficulty predictor score (MUSG Score) in anticipating the difficulty while performing neuraxial block procedures and also to compare the lumbosacral radiological imaging findings with clinical findings.
Materials and Methods
A cross-sectional study was conducted in the Department of Anaesthesiology and Intensive Care at Adesh Institute of Medical Sciences and Research in Bathinda, Punjab, India from March 2023 to March 2024. After obtaining approval from the Hospital Ethics Committee (Ref. No. AU/EC_BHR/2K23/381) and securing patient consent, the study focused on patients admitted for lower limb surgeries, such as hip and knee arthroplasties.
Inclusion criteria: Patients aged 40 to 80 years, classified as American Society of Anaesthesiologists (ASA) I-III, and admitted for lower limb arthroplasty surgeries were included in the study.
Exclusion criteria: Patients who refused to participate, those with infections at the site of injection, coagulopathy, thrombocytopenia, a history of allergy to local anaesthetics, severe valvular stenosis, left ventricular outflow obstructions, or pre-existing neurological conditions such as radiculopathy, multiple sclerosis, intracranial hypertension, and spinal tumours were excluded from the study.
Sample size: The sample size was calculated based on a previous study by Coetzer AP and De Villiers RVP [10], using the incidence of difficult blocks. A sample size calculator (OpenEpi) was employed with a confidence level of 95% and a margin of error of 5%. The calculated sample size was found to be 151 cases. With an attrition rate of 10%, an additional 15 cases were added, resulting in a final sample size of 166.
Study Procedure
Patients enrolled in the study underwent a detailed preoperative anaesthesia check-up at the preanaesthesia clinic. They were asked about co-morbid illnesses, including hypertension, diabetes, cardiac diseases, seizure disorders, and bronchial asthma. The history of any previous surgeries under anaesthesia and any complications related to anaesthesia were noted. A detailed clinical assessment of the lumbar spine was conducted to check for localised swelling, surgical scars, and deformities such as scoliosis, kyphosis, or loss of lordosis. Palpation of the spinous processes and interspinous spaces, as well as tenderness of the spine at any point, were recorded. The interspinous space with easily palpable spinous processes was considered the best interspinous space according to clinical examination, which is a traditional method for selecting the interspinous space for the block [9]. The best space identified radiologically was compared whether it was the same as that determined through clinical examination.
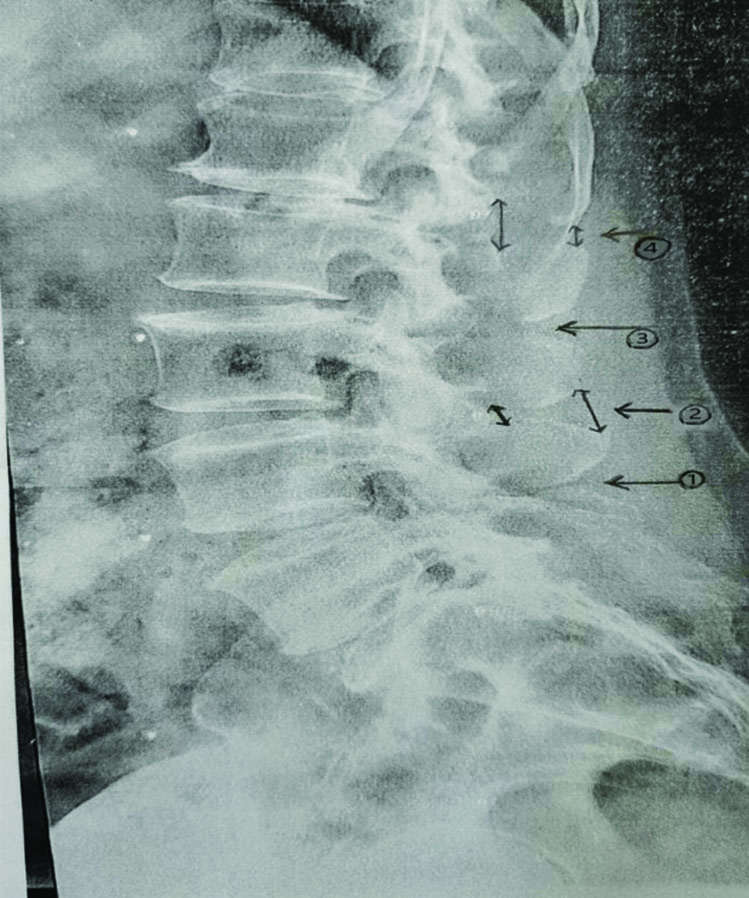
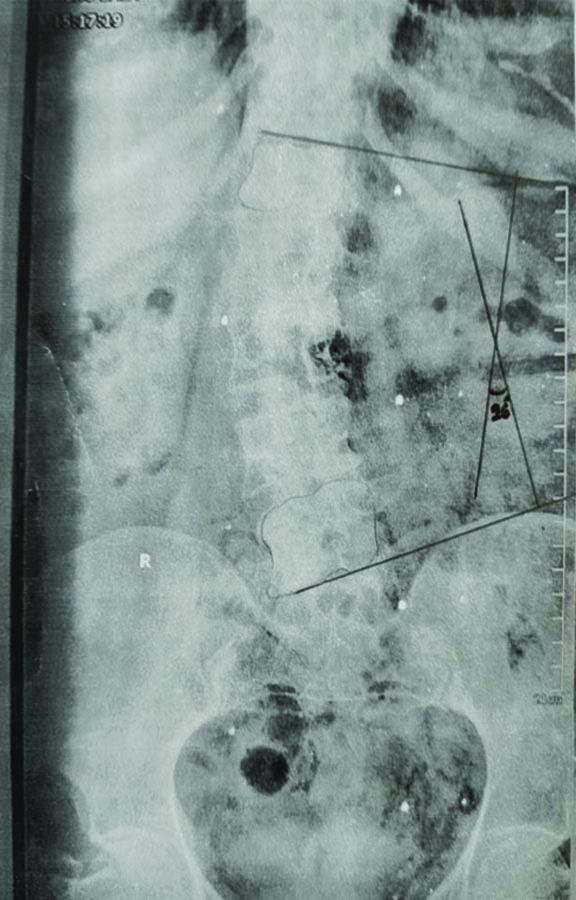
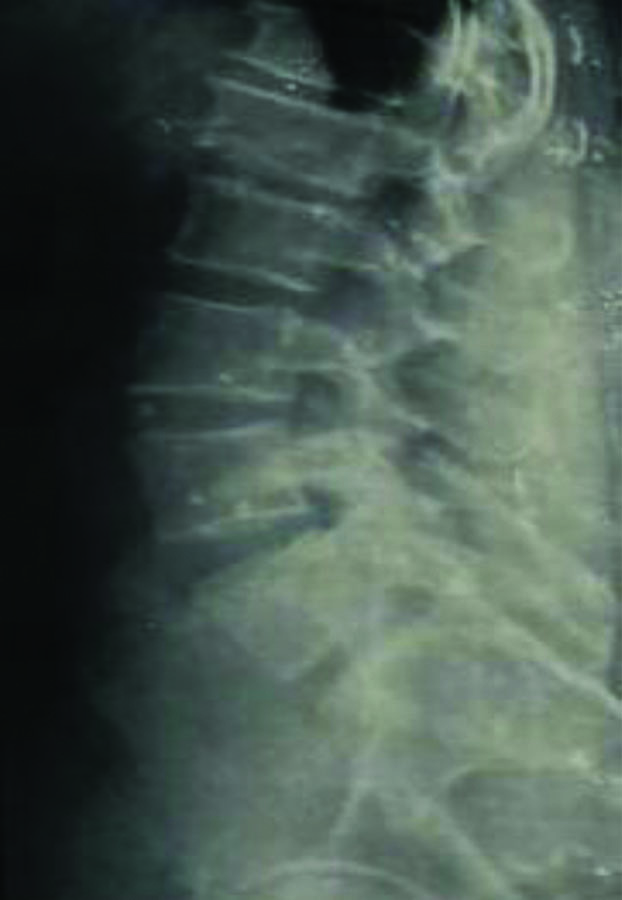
Upon arrival in the preoperative room, written informed consent was obtained from patients for participation in the study. The preanaesthesia check-up sheet was reviewed again. Anteroposterior and lateral views of lumbosacral X-rays of the spine were examined to identify structural abnormalities, such as the degree of scoliosis, vertebral osteophytes, angulation of the spinous processes, calcification of the ligamentum flavum, and the ratio of inner and outer interspinous space height [Table/Fig-1,2 and 3]. A total difficulty score was calculated [Table/Fig-4] [8].
Lateral view lumbar spine radiograph showing: (1) Osteophytes causing narrowing of interspinous space; (2) Inner and outer interspinous distance ratio <1.1; (3) Osteophyte causing beak shaped downward extension of upper spinous process; (4) Ratio of outer and inner interspinous space >1.1.
Anteroposterior view of lumbar spine radiograph showing scoliosis and Cobb’s angle of 26°.
Lateral view of lumbar spine radiograph showing downward angulation of spinous processes.
Total difficulty predictor score (MUSG Score).
| Cobb’s angle (Degree of Scoliosis) [14] | Severity | Score |
|---|
| 11°-25° | Mild | 1 |
| 25°-50° | Moderate | 2 |
| >50° | Severe | 3 |
| Osteophytes | Absent | 1 |
| Present | 2 |
| Angulation of spinous process | Straight | 1 |
| Downward | 2 |
| Fused | 3 |
| Calcification of ligamentum flavum | Absent | 1 |
| Present | 2 |
| Ratio of inner and outer interspinous space height | >1:1 | 1 |
| <1:1 | 2 |
5= easy, 6-9= moderate, 10 or >= difficult
In the current study, the total difficulty predictor score was determined based on the presence of the aforementioned abnormalities in any single interspinous space. For example, if osteophytes were present in one interspinous space, such as L2-L3, the score would be 2 for the lumbar spine, and the same approach was applied to other variables. The individual level score was then calculated for each interspinous space, and the one with the minimum score was selected for the CNB [Table/Fig-5]. The scoring system was validated by 10 subject experts, who found it easy to understand and convenient to implement.
Difficulty predictor score (MUSG Score) at individual interspinous space.
| Parameter | L1-L2 | L2-L3 | L3-L4 | L4-L5 | L5-S1 |
|---|
| Cobb’s angle (degree of scoliosis) | | | | | |
| Osteophytes | | | | | |
| Angulation of spinous processes | | | | | |
| Calcification of ligamentum flavum | | | | | |
| Ratio of inner and outer interspinous space height | | | | | |
After the patient was transferred to the operating theatre, standard monitors such as an Electrocardiogram (ECG), Non Invasive Blood Pressure (NIBP) monitor, and pulse oximeter were connected, and baseline heart rate, mean arterial blood pressure, and oxygen saturation were recorded. Intravenous access was secured, and crystalloid infusion was initiated. The patient was preloaded with 5-10 mL/kg of normal saline 10-15 minutes before administering the neuraxial block. X-rays of the lumbosacral spine, both lateral and anteroposterior views, were displayed and reviewed. The best interspinous space with the minimal difficulty score was selected for the block. The patient was positioned sitting on the operating table, and the neuraxial block was administered using a Tuohy’s epidural needle (18 G) and a Quincke Babcock (25 G) needle, following aseptic cleaning and draping of the back. The block was performed by an expert anaesthesiologist with over three years of experience. The number of attempts required to administer the block was noted; more than two attempts for the procedure were considered difficult. During the block, a change in the direction of the needle was not counted as a new attempt, but a new prick in the same or another space was considered an additional attempt.
The procedure time for administering the spinal epidural block was recorded, starting from the cleaning of the skin until the epidural catheter was secured to the patient’s back. Changes in heart rate and blood pressure were monitored until the completion of the procedure.
Outcome Measure
From the findings of the anteroposterior and lateral view X-rays, the total [Table/Fig-4] and individual interspinous space [Table/Fig-5] difficulty predictor scores were calculated. Outcomes were assessed based on the following criteria:
- The number of attempts required to performing the block (more than two attempts were considered difficult).
- A comparison of the lumbosacral radiological imaging findings with the clinical examination findings in the study patients.
Statistical Analysis
The data was recorded in a Microsoft Excel sheet and analysed using the Microsoft Excel ToolPak Data Analysis. Results were expressed as percentages, frequencies, or mean±SD. Discrete and categorical variables were analysed using the Pearson Chi-square test. Continuous variables were compared with the baseline using Analysis of Variance (ANOVA) and Dunnett’s test (2-sided). A p-value of <0.05 was considered significant.
Results
There were 78 male patients (47%) and 88 female patients (53%). A total of 135 patients (81.3%) underwent knee arthroplasty, while 31 patients (18.7%) had hip arthroplasty. [Table/Fig-6] represents the physical characteristics of the study patients. Data for 166 patients were recorded, and since there was no long-term follow-up, no dropouts were reported.
Physical characteristics of study patients (n=166).
| Parameter | Mean±standard deviation | Minimum | Maximum |
|---|
| Age (years) | 59.83±9.96 | 40 | 80 |
| BMI (kg/m2) | 27.843±2.63 | 24 | 40 |
On clinical examination, lumbar spinous processes were palpable in 162 patients (97.6%) and not palpable in 4 patients (2.4%). Scoliosis was observed in 25 patients (15%), and 6 patients (3.6%) exhibited a loss of the normal lordosis of the lumbar spine [Table/Fig-7].
Clinical examination findings of lumbar spine in study patients (n=166).
| Best palpable interspinous space | Frequency of patients |
|---|
| L1-L2 | 23 |
| L2-L3 | 96 |
| L3-L4 | 43 |
| L4-L5 | 0 |
| L5-S1 | 0 |
| None of the interspinous space were palpable | 4 |
| Scoliosis | 25 |
| Loss of Lordosis of Lumbar spine | 6 |
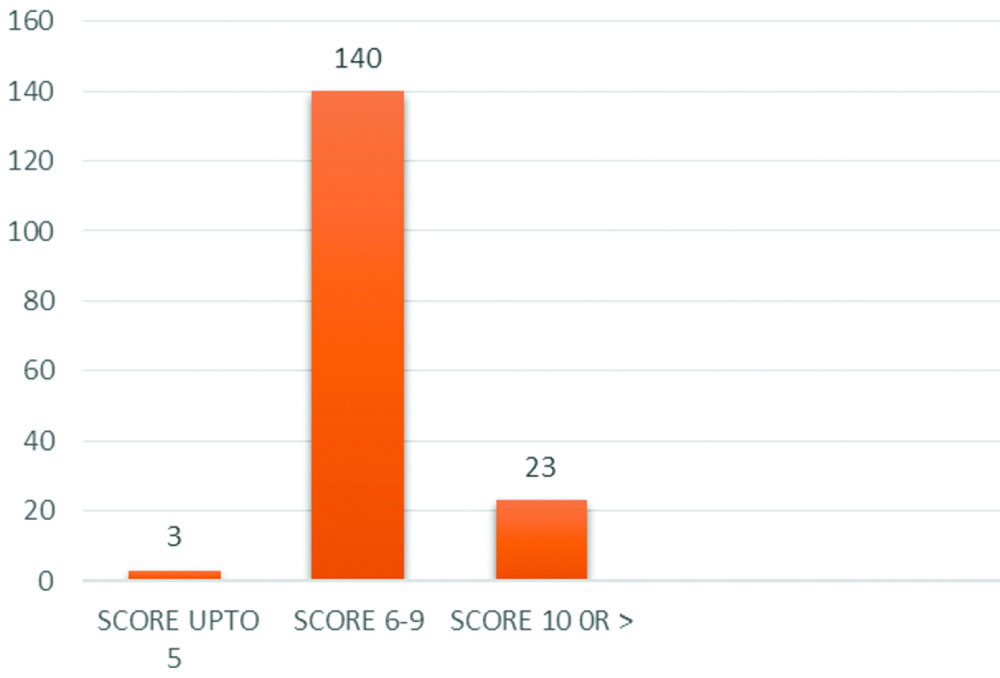
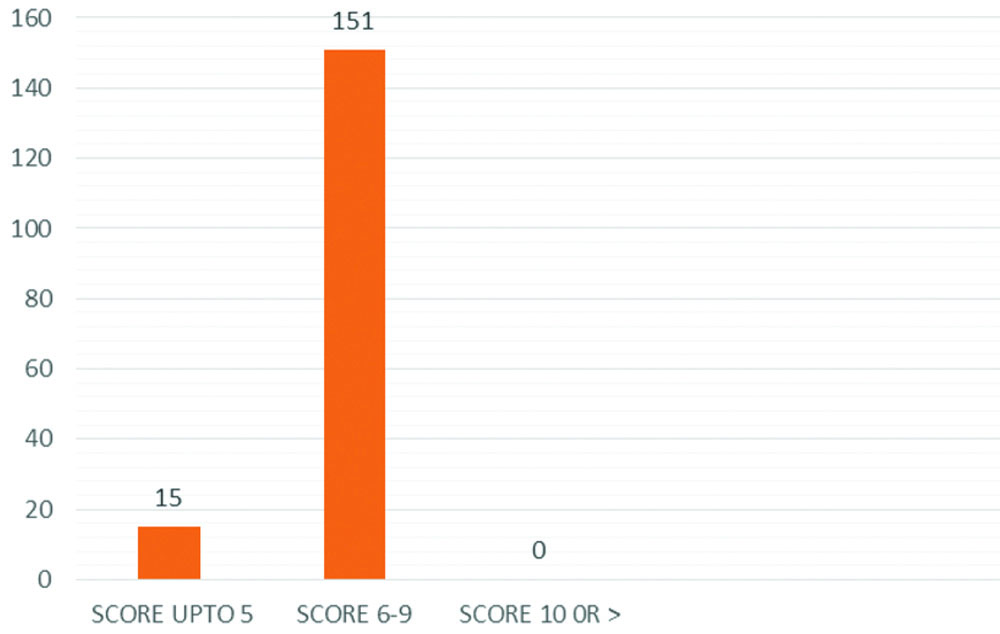
From the radiological findings, the total difficulty score (MUSG Score) was calculated from X-rays of the lumbosacral spine. The total difficulty predictor score was 5 in 3 patients (1.8%), between 6 and 9 in 140 patients (84.3%), and 10 or greater in 23 patients (13.9%) [Table/Fig-8].
Total difficulty predictor score (MUSG Score) in study patients (n=166).
The difficulty predictor score for individual interspinous spaces was calculated, and the space with the minimum difficulty score was selected for the neuraxial block (spinal and epidural). The values are shown in [Table/Fig-9]. A total of 15 patients (9%) had a score of 5, while 151 patients (91%) had scores between 6 and 9, with none having a score of 10 or greater. This indicates that even if the lumbar spine had a total score of 10 or more, there may still be certain interspinous spaces at which the predictor score is lower and more favourable for administering a neuraxial block.
Minimum difficulty predictor score (MUSG Score) at selected space in study patients (n=166).
More attempts were required to perform spinal and epidural blocks in patients with scores between 6 and 9 compared to those with scores of up to 5. However, the difference was not statistically significant [Table/Fig-10]. Accidental dural puncture was observed in six patients while performing the epidural block procedure, and in those patients, the epidural (18 G) catheter was inserted into the subarachnoid space. Local anaesthetic was administered through the epidural catheter into the subarachnoid space. In two patients, authors were unable to successfully administer the block despite multiple attempts; both patients were obese, with a Body Mass Index (BMI) greater than 35 kg/m2, and therefore, general anaesthesia was administered to them. Since the block procedure was attempted, those patients were included in the study.
Number of attempts for epidural and spinal in selected space in study patients (Chi-square test). In six patients we had accidental dural puncture while giving the epidural block, so did not attempted the spinal block, as we fixed epidural catheter in the subarachnoid space. For spinal block drug was injected through the epidural catheter.
| Attempts epidural block | Score | Total | p-value | Attempts spinal block | Score | Total | p-value |
|---|
| 5 | 6-9 | 5 | 6-9 |
|---|
| ≤2 | 14 | 119 | 133 | 0.308 | ≤2 | 13 | 132 | 145 | 0.371 |
| >2 | 1 | 32 | 33 | >2 | 0 | 15 | 15 |
| Total | 15 | 151 | 166 | Total | 13 | 147 | 160 |
Authors found that during clinical palpation examination, the best palpable space was L2-L3 (96 patients, 57.8%), followed by L3-L4 (43 patients, 25.9%) and L1-L2 (23 patients, 13.9%). The interspinous space was not palpable in 4 patients (2.4%). The best interspinous spaces with minimum difficulty scores from radiological assessments of the lumbar spine were L2-L3 (76 patients, 45.7%), L3-L4 (62 patients, 37.3%), and L1-L2 (28 patients, 16.9%). The detection of scoliosis and loss of normal lordosis of the lumbar spine was equal in both clinical examination and radiological imaging. It has been observed that the best palpable space during clinical examination may not always correspond to the best space identified on radiological imaging [Table/Fig-11].
Comparison of clinical and radiological examination in study patients (n=166) (Chi-square test).
| Parameter | Clinical examination | Radiological | p-value |
|---|
| Best space | L1-L2 (23) | L1-L2 (28) | 0.50233 |
| L2-L3 (96) | L2-L3 (76) | 0.0145 |
| L3-L4 (43) | L3-L4 (62) | 0.0359 |
| Scoliosis | 25 patients | 25 patients | 1 |
| Loss of lordosis | 6 patients | 6 patients | 1 |
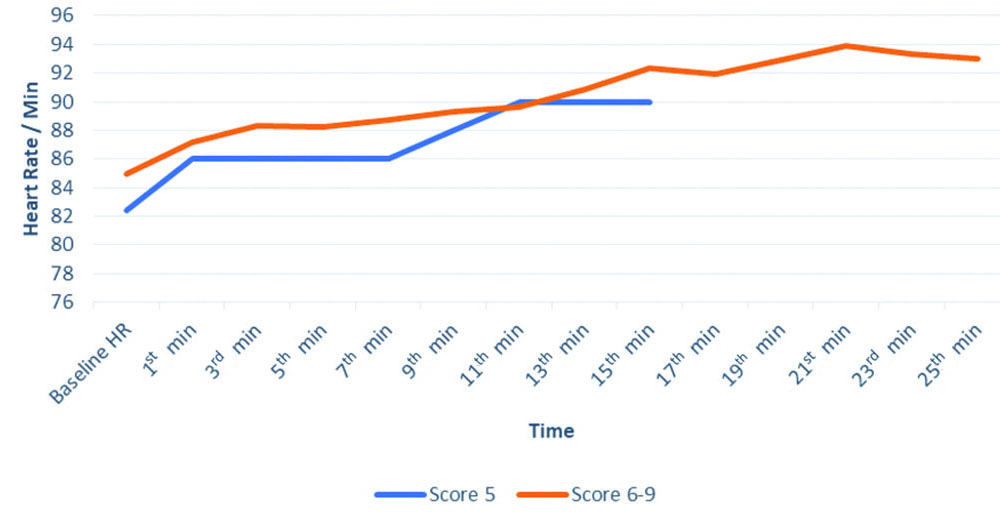
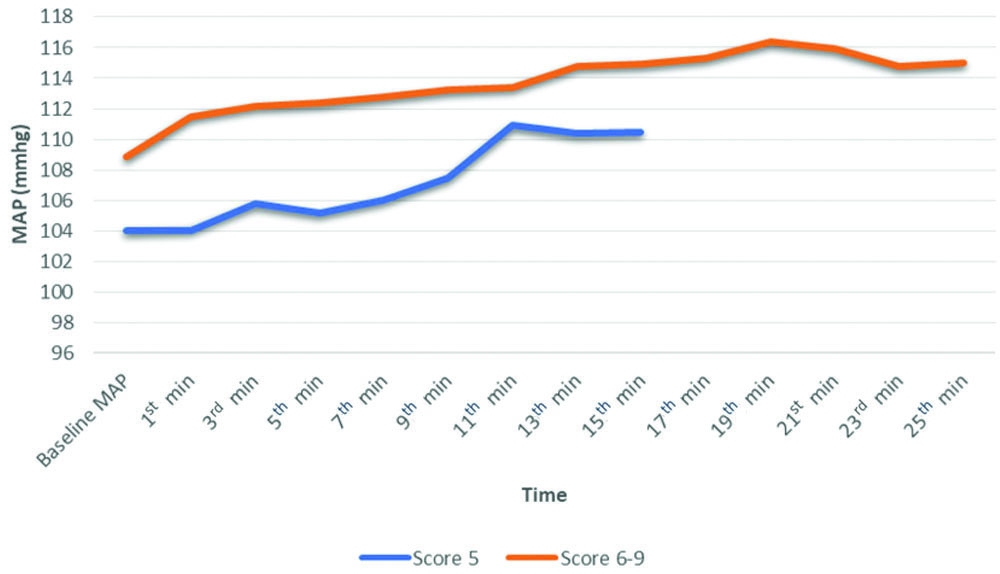
The time taken to perform the block was significantly longer in patients with scores of 6-9 compared to patients with a score of 5 (p=0.030) [Table/Fig-12]. No significant changes were observed in heart rate for patients with scores up to 5; however, significant changes were noted in patients with scores of 6-9 at the 11th minute (p=0.028), 13th minute (p=0.014), 15th minute (p=0.004), 17th minute (p=0.036), 19th minute (p=0.017), and 21st minute (p=0.008) [Table/Fig-13]. Changes in mean arterial blood pressure from baseline were not significant in patients with scores up to 5, but in patients with scores of 6-9, significant changes were observed at the 5th minute (p=0.040), 7th minute (p=0.012), 9th minute (p=0.003), 11th minute (p=0.001), 13th minute (p=0.001), 15th minute (p=0.001), 17th minute (p=0.006), 19th minute (p=0.004), and 21st minute (p=0.008) [Table/Fig-14]. No changes occurred in oxygen saturation during the procedure.
Time taken for performing the block procedures in study patients (n=166)
| Score | Maximum time (min) | Minimum time (min) | Mean time (min)±Standard deviation | p-value |
|---|
| 5 | 15 | 10 | 11.13±1.70 36 | 0.030 |
| 6-9 | 25.30 | 7 | 13.99±5.05 |
(Chi-square test)
Changes in heart rate during the procedure time.
Changes in mean arterial pressure during the procedure.
Discussion
Based on the difficulty predictor score (MUSG Score), which was calculated from lateral and anteroposterior views of lumbosacral spine X-rays, it was demonstrated that the best-selected spaces with minimal difficulty predictor scores for spinal epidurals in study patients, based on radiological findings, were in the following order: L2-L3 (76), L3-L4 (62), and L1-L2 (28). In a similar study, Jang D and Park S found that the interspinous height is maximum at the L1-L2 interspinous space and minimum at L4-L5. They noted that the interspinous distance decreases with the ageing process. Their study also revealed that the skin-to-spinous process depth is minimum at L1-L2, gradually increasing, and maximum at L5-S1 [12]. In present study, the radiologically best interspinous spaces were L2-L3, L3-L4, and L1-L2, which were the most suitable for neuraxial block. The interspinous spaces L4-L5 and L5-S1 were the least suitable for neuraxial block due to their higher difficulty scores. The difficulty score was more than 8 in these interspinous spaces, and their spinous processes were not easily palpable.
Upon clinical examination, the best palpable interspinous spaces were in the order L2-L3 (96), L3-L4 (43), and L1-L2 (23). The spinous processes of L4-L5 and L5-S1 were the least palpable during clinical examination. Kaya Ayvaz D et al., revealed that the posterior height and length of the spinous process increase from L1 to the maximum at L2 and then begin to decrease, reaching a minimum at L5 [13]. Similarly, present study found that the spaces with the minimum difficulty score and best palpability were in the order of L2-L3, L3-L4, and L1-L2. The interspinous spaces L4-L5 and L5-S1 had the maximum scores and were also the least palpable. Present study also demonstrated that the best palpable interspinous space may or may not correspond to the space with the minimum difficulty score calculated from radiological imaging findings. Therefore, X-rays of the lumbar spine help in anticipating difficult neuraxial blocks in what is otherwise a blind procedure and guide the anaesthesiologist in choosing the best interspinous space.
In four patients, none of the interspinous spaces were palpable. In two of these patients with a BMI greater than 35 kg/m2, neuraxial block could not be performed and therefore general anaesthesia was administered. Uyl N et al., found in their study that obesity, indicated by an increased BMI, raises the risk of difficult or failed epidural placement [14].
More attempts were required to perform spinal and epidural blocks in patients with a score of 6-9 compared to those with a score of up to 5. The rise in heart rate and blood pressure from baseline was greater in patients with a score of 6-9 than in those with a score of 5. In patients with a score of 6-9, the presence of bony abnormalities often resulted in multiple attempts and a longer duration for the procedure, which increased patient anxiety and fear, as well as pain from needle pricks, leading to elevated heart rates and blood pressure. Acute pain triggers a neuroendocrine stress response, which causes a transient increase in heart rate and blood pressure [15,16].
A significant difference (p-value <0.05) was observed between the clinically palpable best interspinous space and the radiologically selected best space at the L2-L3 and L3-L4 levels, while no significant difference was noted at the L1-L2 level. X-rays of the lumbosacral spine, performed prior to administering spinal and epidural anaesthesia, along with clinical examination, can predict the difficulty of performing neuraxial blocks. A minimum score of 5 predicts easier spinal and epidural procedures compared to those with a higher predictor score. In present study, the mean age of the patients was over 55 years, and most patients exhibited age-related changes in the lumbosacral spine, such as osteophytes and angulation of spinous processes, which could not be assessed through clinical examination alone. Therefore, X-rays of the lumbosacral spine assisted us in selecting the best space with minimal difficulty, making the procedure more convenient for the anaesthesiologist and more comfortable for the patient. Ghaly RF et al., also recommended the use of imaging of the lumbosacral spine, in conjunction with clinical examination, prior to administering epidural steroid injections and before invasive neuraxial procedures in patients with lower back pain [17].
The current study was conducted on older patients who underwent hip and knee arthroplasty surgeries. These patients typically exhibit degenerative bony changes in the spine, which complicate the performance of neuraxial blocks. The use of anteroposterior and lateral view X-rays helped us to visualise interspinous changes in the lumbar spine, providing insight into an otherwise blind procedure that could not be achieved using traditional palpation techniques. This study advocates for the use of preoperative X-rays of the lumbosacral spine, in conjunction with clinical palpation techniques, to anticipate difficult neuraxial blocks and select the best space for block procedures in elderly patients.
Limitation(s)
Being a single-centric and first-of-its-kind study, it requires further research with a larger sample size to enhance the applicability of this difficulty predictor score (MUSG score) in the future.
Conclusion(s)
Based on the predictor score, the anaesthesiologist can choose the best interspinous space in elderly patients undergoing hip and knee arthroplasties. A minimum score of five predicts an easier block, while a higher score indicates more difficulty. In present study, the interspinous spaces with the lowest scores were most commonly L2-L3, L3-L4, and L1-L2, which were deemed suitable for easier block procedures.
(Chi-square test)