Anxiety disorders significantly impact well-being and productivity at a personal level, as well as contribute to economic losses at a national level. The National Mental Health Survey (NMHS) of India (2016) reported a prevalence rate of 2.57% for anxiety disorders [1]. In Punjab, the prevalence rate of neurotic and stress-related diseases is estimated to be 3.25% [2]. The NMHS highlighted that around 60% of individuals experienced varying levels of disability, and there is a considerable treatment gap for anxiety disorders, estimated at 82.9%, which is quite substantial [1].
The course of anxiety disorders is characterised by fluctuating symptom severity, a high relapse rate, and chronicity. Given the diminished quality of life, functional impairment, and absenteeism linked to residual symptoms, it is advisable to approach treatment with caution [3]. Patients diagnosed with anxiety disorders are typically prescribed antidepressants or anti-anxiety medications [4]. Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) are recommended as first-line treatments due to their favourable benefit-to-risk ratio [5]. Research studies have indicated that pharmacological therapies alone have restricted long-term efficacy [6]. Combining pharmacotherapy with non-pharmacological techniques, such as Progressive Muscular Relaxation (PMR), may prove more effective in managing anxiety disorders compared to either treatment alone [4].
PMR was originally developed by American physician Edmund Jacobson, who first introduced the technique at Harvard University in 1908 and later outlined a comprehensive process for muscle tension reduction in his book “Progressive Relaxation,” published in 1929 [7]. The theory underlying PMR is that relaxation and anxiety are linked to opposing autonomic nervous systems (parasympathetic and sympathetic). Thus, tension and anxiety are incompatible with relaxation. Therefore, applying relaxation techniques should help diminish worry and tension, particularly [8]. Joseph Wolpe further enhanced Jacobson’s method into a 20-minute regimen [9]. Jacobson’s method of PMR has been modified by various scientists and medical professionals over time, resulting in multiple contemporary variations of the technique [10].
The utilisation of PMR is particularly effective in alleviating stress, anxiety, and depression due to its straightforward nature and lack of adverse effects. This makes it accessible, cost-effective, and self-induced. By distinguishing between sensations of tension (intentional muscle tensing) and relaxation (conscious muscle tension release), PMR facilitates the identification of persistently tense muscle groups. The significance of Escitalopram or PMR as standalone treatments in the management of neurotic, stress-related, and somatoform disorders is well established [11,12]. However, it is noteworthy that approximately 20% of patients may require a duration of 10 to 12 weeks, or even longer, before exhibiting any therapeutic response [11]. Furthermore, the management of residual symptoms presents a considerable challenge [13]. Additionally, the corpus of studies available on PubMed that assess the efficacy of antidepressants in conjunction with PMR for the treatment of neurotic, stress-related, and somatoform disorders remains markedly limited. Existing research [12] indicates that combining PMR with other non-pharmacological interventions enhances the efficacy of PMR compared to its standalone application. Consequently, it may be advantageous for researchers to consider integrating PMR with pharmacological therapy to amplify its potential in diminishing anxiety and stress [12]. Therefore, we posit the null hypothesis that there will be no difference in the level of anxiety after treatment with either Escitalopram alone or in combination with PMR therapy. This study was conducted to assess and compare the Hamilton Anxiety Rating Scale (HAM-A) scores at six-months between Group-E (who received Escitalopram exclusively) and Group-E+PMR (who received Escitalopram in addition to PMR). The objective was also to compare the baseline HAM-A scores with those obtained after six months within each group.
Materials and Methods
A hospital-based randomised clinical study was conducted from March 2020 to March 2021. The study commenced after receiving approval from the IEC at Sri Guru Ram Das Institute of Medical Sciences and Research in Amritsar, Punjab, through a formal letter with reference number SGRD/IEC/Pat 56/20 dated February 7, 2020. The study population comprised individuals who visited the Psychiatry OPD at Sri Guru Ram Das Institute of Medical Sciences and Research in Amritsar and qualified for a provisional diagnosis of neurotic, stress-related, and somatoform disorders.
Sample size calculation: The sample size was determined based on the prevalence of neurotic, stress-related, and somatoform disorders, which was reported as 3.25% according to a prior investigation [2]. The chance of error was assumed to be 5%, with a confidence level of 95%. By utilising the formula n=z2×pq/d2, the sample size was calculated to be 50 in each group. Considering an expected attrition rate of 20%, the final total sample size for each group was approximately 60.
Eligibility criteria: Inclusion criteria consisted of individuals aged 18 to 45 years who were diagnosed with neurotic, stress-related, and somatoform disorders according to the ICD-10 criteria (F40-F48) [14] and who provided informed consent. Conversely, exclusion criteria included patients with physical conditions such as cardiac and respiratory diseases, psychiatric comorbidities, substance abuse or dependence, as well as uncooperative individuals or those with communication limitations, including muteness, deafness, speech impairments, or intellectual disabilities.
Methodology: Patients who visited the Psychiatry department at Sri Guru Ram Das Institute of Medical Sciences and Research in Amritsar, Punjab, between March 2020 and October 2020 were approached and requested to participate in the study. Patients underwent a screening process to determine their eligibility for the research study. Following the receipt of informed consent, each participant was independently assessed by two psychiatrists to confirm the diagnosis of neurotic, stress-related, and somatoform disorders according to ICD-10 criteria. A semi-structured proforma was utilised to collect socio-demographic information.
Participants were randomly allocated to the two groups using a simple randomisation method (utilising a computerised random numbers table). The first group, referred to as Group-E for brevity, received Escitalopram as a standalone treatment for six months. The second group, designated as Group-E+PMR, practiced Jacobson’s PMR exercise in conjunction with receiving Escitalopram. Both groups received Escitalopram at a dosage of 10 mg once daily [15]. Participants in the PMR group were instructed on the PMR technique by the principal investigators and advised to practice it at home for 20 minutes twice a day over the course of six months. A video illustrating the PMR process was created and distributed to all participants in the PMR group to serve as a guide whenever they encountered difficulties in practicing PMR.
In this study, participants engaged in PMR in a comfortable setting, starting the exercise in a supine position while emphasising continuous breathing. The recommended approach involved beginning with the feet and progressing upwards towards the forehead, targeting specific muscle groups, including the toes, feet, calves, thighs, buttocks, hips, waist, abdominal muscles, fists, hands, upper arms, chest, shoulders, back, neck, jaw, mouth, cheeks, eyes, and forehead. The exercise entailed a systematic process of inhaling and tensing each muscle group for 3-5 seconds, followed by a brief hold, exhalation, and then relaxation for 10-15 seconds, sequentially moving through all the muscle groups [10]. All participants were provided with a sheet to record whether they had completed the PMR exercise twice a day. Only participants who regularly performed the PMR sessions were included in the study.
Participants in both groups were evaluated using the HAM-A at the beginning of the study and again after six months. The HAM-A is a commonly used rating scale for assessing the severity of anxiety symptoms. It comprises 14 items, each item delineating a set of symptoms and evaluating both psychic and somatic anxiety. Scoring for each item ranges from 0 (indicating absence) to 4 (indicating severity), yielding a total score range of 0-56. A score below 17 suggests mild severity, while scores between 18-24 indicate mild to moderate severity, and scores falling within 25-30 suggest moderate to severe symptoms [16]. The HAM-A scores at baseline and after six months were the primary outcome measures.
Statistical Analysis
After collecting and coding the data, it was entered into the Statistical Package for the Social Sciences (SPSS) version 24.0. Continuous variables were described using the mean and standard deviation, while categorical variables were presented using frequencies and percentages. The Chi-square test (χ2) was applied to compare categorical variables, whereas the t-test was utilised to compare continuous variables. The effectiveness of the treatment was assessed by examining variations in the mean HAM-A scores. A paired t-test was conducted to compare the HAM-A scores prior to and following treatment within a specific group, while an independent t-test was employed to compare HAM-A scores across the two groups. Statistical analysis was carried out using SPSS version 24.0 and a significance level of p<0.05 was adopted for the statistical assessments.
Results
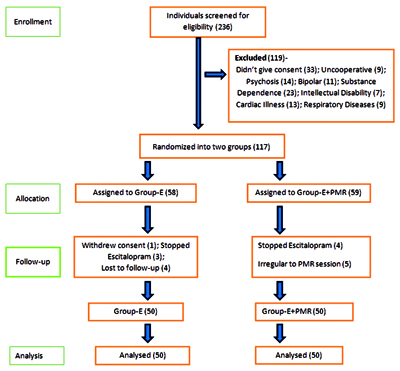
At the beginning of the study, 236 individuals were screened for potential participation, as depicted in [Table/Fig-1]. A total of 119 individuals were deemed ineligible and, therefore, had to be excluded from the study. The remaining 117 participants who satisfied the established inclusion criteria were randomly assigned to either Group-E (n=58) or Group-E+PMR (n=59). Within Group-E, one participant chose to withdraw the consent, three participants independently discontinued Escitalopram, and four participants were lost to follow-up. In Group-E+PMR, four participants stopped taking Escitalopram, and five participants displayed irregular attendance at the PMR sessions. Consequently, the analysis was conducted on 50 participants in each group. The mean (SD) age was 30.6±7.9 years [Table/Fig-2]. Most individuals in both groups were female (70%), indicating a greater incidence of anxiety among females (70%) compared to males (30%). Most participants were married (67%), unemployed (65%), had limited educational attainment (59%), lived in extended family setups (60%), and came from lower-middle (45%) to upper-lower class (29%) backgrounds [Table/Fig-2]. Upon comparison, no significant differences were found between Group-E and Group-E+PMR in terms of mean age and other socio-demographic variables. No significant difference (p>0.05) was observed between the two groups regarding the incidence of neurotic, stress-related, and somatoform disorders [Table/Fig-3].
Flow diagram of the study.
Comparison of socio-demographic variables.
| Variables | Group-E (n1=50) | Group E+PMr (n2=50) | Total (N=100) | p-value |
|---|
| Age (in years), Mean±SD | 30.5±7.7 | 30.7±8.3 | 30.6±7.9 | 0.92§ |
| Sex, n (%) | Males | 14 (28%) | 16 (32%) | 30 (30%) | 0.82† |
| Females | 36 (72%) | 34 (68%) | 70 (70%) |
| Marital status, n (%) | Married | 35 (70%) | 32 (64%) | 67 (67%) | 0.67† |
| Unmarried | 15 (30%) | 18 (36%) | 33 (33%) |
| Domicile, n (%) | Rural | 35 (70%) | 34 (68%) | 69 (69%) | 0.86† |
| Urban | 5 (10%) | 4 (8%) | 9 (9%) |
| Semi urban | 10 (20%) | 12 (24%) | 22 (22%) |
| Family type, n (%) | Nuclear | 5 (10%) | 6 (12%) | 11 (11%) | 0.94† |
| Joint | 15 (30%) | 14 (28%) | 29 (29%) |
| Extended | 30 (60%) | 30 (60%) | 60 (60%) |
| Educational status, n (%) | Illiterate | 28 (56%) | 31 (62%) | 59 (59%) | 0.14† |
| High school | 3 (6%) | 0 (0%) | 3 (3%) |
| Intermediate/diploma | 3 (6%) | 0 (0%) | 3 (3%) |
| Graduate | 6 (12%) | 5 (10%) | 11 (11%) |
| Professional degree | 10 (20%) | 14 (28%) | 24 (24%) |
| Occupational status, n (%) | Unemployed | 30 (60%) | 35 (70%) | 65 (65%) | 0.6† |
| Clerical/shop/farm | 14 (28%) | 10 (20%) | 24 (48%) |
| Professional | 6 (12%) | 5 (10%) | 11 (11%) |
| Socio-economic status, n (%) | Lower middle | 23 (46%) | 22 (44%) | 45 (45%) | 0.97† |
| Upper lower | 14 (28%) | 15 (30%) | 29 (29%) |
| Lower | 13 (26%) | 13 (26%) | 26 (26%) |
Group-E: Escitalopram only; Group-E+PMR: Escitalopram+Progressive muscular relaxation group; §Independent t-test; †Chi-square test
Comparison of incidence of neurotic, stress related and somatoform disorders (N=100).
| Clinical variables | Group-E (n1=50) | Group-E+PMR (n2=50) | p-value |
|---|
| F40, n (%) | 7 (14%) | 8 (16%) | 0.98† |
| F41.0, n (%) | 7 (14%) | 6 (12%) |
| F41.1, n (%) | 9 (18%) | 10 (20%) |
| F42, n (%) | 5 (%) | 4 (8%) |
| F43, n (%) | 2(4%) | 3 (6%) |
| F43.2, n (%) | 3 (6%) | 1 (2%) |
| F44, n (%) | 14 (28%) | 14 (28%) |
| F45, n (%) | 3 (6%) | 4 (8%) |
Group-E=Escitalopram only; Group-E+PMR=Escitalopram+Progressive muscular relaxation group; †Chi-square test; F40 Phobic anxiety disorders; F41.0 Panic disorder; F41.1 Generalised anxiety disorder; F42 Obsessive-compulsive disorder; F43 Acute stress reaction; F43.2 Adjustment disorder; F44 Dissociative (conversion) disorder; F45 Somatoform disorders
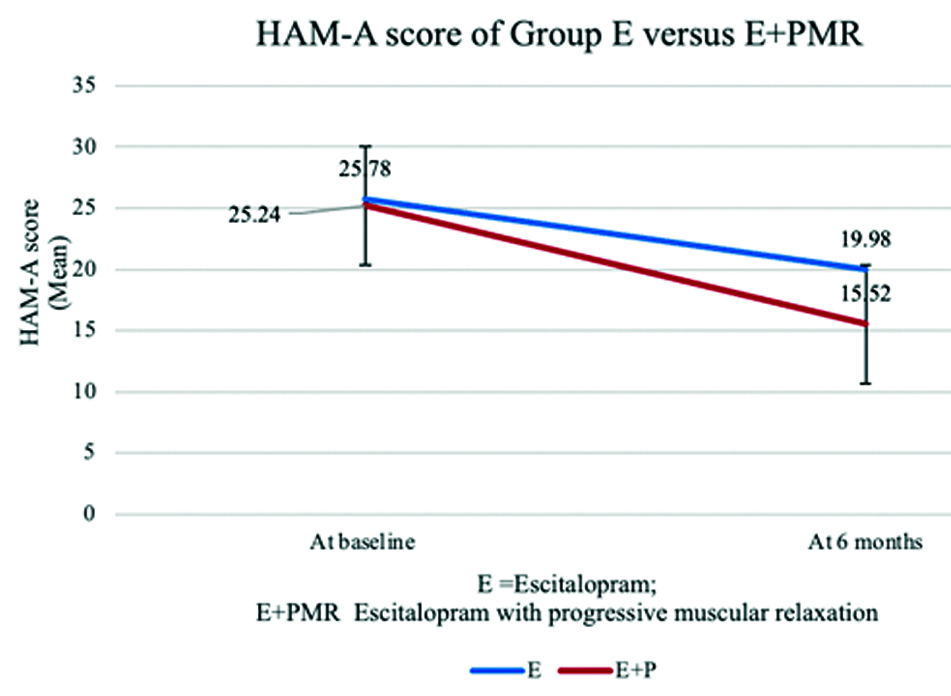
The HAM-A score after six months, in relation to the baseline HAM-A score [Table/Fig-4], was significantly lower (p<0.001) in both Group-E and Group-E+PMR. The baseline anxiety levels were comparable between Group-E and Group-E+PMR, with a p-value of 0.67 [Table/Fig-5,6]. However, the HAM-A score at six months in Group-E+PMR was significantly lower (p<0.001) than in Group-E [Table/Fig-2,4], indicating a more substantial improvement in Group-E+PMR.
Comparison of HAM-A score at base line versus at 6 months within the groups.
| Group | HAM-A (Mean±SD) | t | df | p-value§ |
|---|
| At baseline | At 6 months |
|---|
| E | 25.78±6.54 | 19.98±6.03 | 14.65 | 49 | <0.001 |
| E+PMR | 25.24±6.19 | 15.52±5.02 | 25.79 | 49 | <0.001 |
§Paired t-test
Comparison of HAM-A scores between the groups.
| Variables | E | E+PMR | t | df | p-value† |
|---|
| HAM-A(at baseline)(Mean±SD) | 25.78±6.54 | 25.24±6.19 | 0.42 | 98 | 0.67 |
| HAM-A(at 6 months)(Mean±SD) | 19.98±6.03 | 15.52±5.02 | 4.02 | 98 | <0.001 |
†Independent t-test
Improvement in HAM-A score for Group-E+PMR than Group-E.
Discussion
The vast majority, 70 (70%), of individuals who participated in this research were female, a trend that aligns with prior studies demonstrating that anxiety disorders are nearly twice as prevalent in females compared to males [6]. The severity of anxiety, as indicated by the HAM-A score, was comparable at baseline in both groups, and both groups displayed improvement following treatment.
In the current study, Group-E+PMR engaged in a self-directed application of an adapted version of PMR for a duration of 20 minutes, twice a day, at home. A systematic review conducted by Muhammad Khir S et al., concluded that PMR demonstrated efficacy in mitigating anxiety through both its original and adapted forms. The review further indicated that when individuals engaged in PMR exercises independently in private environments, the lengths of the sessions varied between five minutes to 28 minutes. Moreover, the review elucidated that, irrespective of session duration and frequency, PMR consistently improved anxiety [12].
The improvement in HAM-A scores observed in Group-E+PMR in the current study corresponds with previous research [17-20] illustrating the effectiveness of PMR in reducing anxiety in various contexts such as pregnancy [17], hypertension [18], congestive heart failure [19], and tuberculosis [20]. A separate investigation, characterised by randomisation and single blinding, encompassed 156 nursing students. Findings from this research indicated that the implementation of PMR resulted in a reduction of anxiety levels, despite not achieving statistical significance as observed in the present study [21]. An advantage of PMR is its lower demand on therapists. While it is less demanding, it is equally effective as cognitive therapy in managing Generalised Anxiety Disorder (GAD) [6].
The current study showed that PMR, in combination with Escitalopram, was more effective than Escitalopram alone in the management of anxiety disorders. This outcome aligns with the results of a prior systematic review that encompassed forty-six studies from sixteen different countries and involved 3,402 adult participants [12]. The systematic review indicated a consistent enhancement in the effectiveness of PMR in reducing stress and anxiety levels when utilised in conjunction with other modalities, as opposed to its standalone application [12].
Similarly, a separate study conducted by Katzman M et al., involving 41 individuals diagnosed with GAD, revealed that augmenting antidepressants with Sudarshan Kriya yoga led to remission, a result that had not been achieved with standard antidepressant treatment alone [22]. In another randomised controlled clinical trial, engagement in 30-minute PMR sessions for five consecutive days by 51 patients diagnosed with Coronavirus Disease 2019 (COVID-19), who exhibited anxiety upon admission to isolation units, resulted in a significant decrease in anxiety scores. This clinical trial endorsed PMR as an auxiliary approach for reducing anxiety [23].
The augmentation of Escitalopram with PMR has also shown to be beneficial in cases of depression. A research study [24], involving 30 patients with mild to moderate depression, demonstrated that combining PMR with Escitalopram significantly enhanced the treatment response compared to PMR or Escitalopram monotherapy [24].
Considering the positive impact of both PMR and Escitalopram, it is imperative to explore the reasons behind the augmented effectiveness of their combination. Escitalopram functions by modulating neurochemical pathways to limit the expression of negative emotions, while PMR assists patients in acquiring relaxation skills to induce a sense of calmness that effectively counteracts these negative emotions. Consequently, this dual approach exerts a substantial and lasting influence on the mental health and overall well-being of patients. Moreover, the focus on breathing during PMR practice aids in reducing unnecessary thoughts and alleviating anxiety symptoms [24].
Another rationale elucidating the advantageous effects of PMR is its utilisation of the principles of neuronal processing, particularly the mechanisms of “top-down” and “bottom-up” processing to produce favourable results. In “top-down” processing, individuals activate higher brain regions, such as the cerebral cortex and cerebellum, to tense muscles and subsequently alleviate stress. In contrast, “bottom-up” processing involves the generation and release of bodily tension, eliciting proprioceptive signals from peripheral muscles that travel to the brain via the spinal cord and brainstem. By engaging both pathways, PMR delivers prompt and immediate relief to participants [25].
Another model elucidating the role of PMR is the neuro-physiological unifying model, which proposes that breathing exercises exert their effects by stabilising the autonomic and stress response systems, reducing chemoreceptor reflex sensitivity, and improving the baroreflex response. Consequently, the transition to parasympathetic dominance inhibits the cortical regions involved in executive functions and activates the limbic system. Additionally, through increased secretion of prolactin and oxytocin, these exercises promote feelings of calmness and bonding [24,26].
Limitation(s)
The research was constrained by specific limitations. For instance, the analysis focused solely on a comparison between Group-E+PMR and Group-E; however, including a third group that received only PMR treatment could have provided a more comprehensive analysis. Another constraint was that adherence to PMR was self-reported by the participants.
Conclusion(s)
Anxiety disorders were approximately twice as prevalent in females as in males. Escitalopram and Escitalopram combined with PMR treatment significantly lowers anxiety levels. However, combining Escitalopram and PMR results in a much larger improvement than Escitalopram monotherapy alone. Future research endeavors could benefit from exploring the efficacy of this combined therapy in patients with anxiety disorders that coexist with other medical conditions. Additionally, tailoring this combination therapy to meet the unique needs of specific demographic groups, including the elderly, children, and pregnant women, could provide invaluable insights and foster more inclusive therapeutic strategies.
Group-E: Escitalopram only; Group-E+PMR: Escitalopram+Progressive muscular relaxation group; §Independent t-test; †Chi-square test
Group-E=Escitalopram only; Group-E+PMR=Escitalopram+Progressive muscular relaxation group; †Chi-square test; F40 Phobic anxiety disorders; F41.0 Panic disorder; F41.1 Generalised anxiety disorder; F42 Obsessive-compulsive disorder; F43 Acute stress reaction; F43.2 Adjustment disorder; F44 Dissociative (conversion) disorder; F45 Somatoform disorders
§Paired t-test
†Independent t-test