In India, smoking is a common problem in both urban and rural areas, regardless of the type of tobacco used, such as cigarettes, bidis, cigars, etc., [1]. According to NFHS-III, 55.8% male, 10.8% female between the ages of 12 and 60 years have been found to be consuming tobacco. There are 32.7% smokers and 36.5% chewers of tobacco among men, compared to 1.4 and 8.4%, respectively, among women [2]. More than eight million people die from tobacco-related diseases worldwide each year. Around seven million of those deaths are caused by smoking heavily, while 1.2 million are brought on by non-smokers being exposed to passive smoking or SHS [3]. Passive smoking or Environmental Tobacco Smoke (ETS) exposure has sometimes been referred to as “involuntary smoking” or SHS. ETS is made up of Sidestream (SS) smoke from burning cigarettes, bidis, and hookahs as well as the remaining Mainstream (MS) smoke that smokers exhale. SHS inhale nicotine and toxic substances in equal amounts to those of the active smokers. More than 7,000 chemicals have been identified in secondhand tobacco smoke that can cause cancer [4]. According to a recent Global Youth Tobacco Survey (GYTS) study conducted in India, children are more likely to be exposed to SHS [5]. Prolonged SHS exposure has the same detrimental effects as prolonged active smoking. Research findings indicated a correlation between smokers’ susceptibility to fatal arrhythmias and indications of elevated sympathetic or decreased vagal activity [6].
SLT product consumption is a serious health issue both abroad and in India. The prevalence ratio of SLT is more in rural areas, and is common among men and women. SLT products such as “chewing tobacco, moist, dry snuff, dissolvable tobacco, or gutka” [7]. One study had demonstrated that exposure to passive smoking or ETS causes autonomic imbalance in young and middle-aged subjects [8]. The chronic exposure of SLT on cardiac autonomic sympathetic assessment has not been clarified. In India only limited numbers of studies have been conducted among SLT user’s to highlight the cardiac autonomic nerve activity especially in western part of India [9]. To our knowledge, no analysis has been done to determine the impact of longer-term exposures to passive smoking and SLT on sympathetic activity. Hence, the aim of the study was to:
Materials and Methods
The present cross sectional study was conducted in the Department of Physiology, Nootan Medical College and Research Centre, Visnagar, Gujarat, India from August 2023 to February 2024. Study was approved by the institutional ethics committee (Approval No: IEC/NMCRC/APPROVAL/26/2023) and an informed consent was taken from all the subjects after explaining the test procedures and the goal of the study in local language (Gujarati/Hindi).
Inclusion criteria: Non-smokers who chew tobacco for at least five gram per day and for more than five years duration who had never been a passive smoker and are between the ages of 20 and 40 were included. Non-smoking male subjects those who stayed with at least one smoker or interacted regularly with smokers for at least three years were included.
Exclusion criteria: Subjects with acute or chronic diseases like diabetes, cardiac diseases, smoking, alcoholism, bronchial asthma and hypertension were excluded.
Study group:
Group-A-SLT (Smokeless tobacco): 50 Non-smokers who chew tobacco more than five years for at least five gram per day and who has never been a passive smoker and are between the ages of 20 to 40.
Group-B (Passive smokers): 50 matched in age non-smokers who lived with at least one smoker (cigarette/bidi smokers) or frequently interacted with smokers for at least three years.
Parameters chosen for the present study:
(i) Anthropometric measurements: Height, Weight, Body Mass Index (BMI), Body Surface Area (BSA).
(ii) Test Parameters: Resting heart rate, heart rate response to immediate standing, resting supine blood pressure, blood pressure response to immediate standing, blood pressure response to sustained handgrip.
Study Procedure
The subject’s clinical history was taken, including pertinent historical events, family history, drug history, and personal history like smoking, drinking, etc. Standardised questionnaire was given to subjects to obtain information about their history of passive smoking, SLT consumption, past or present health issues etc. Anthropometric measurements were recorded for each subject [10,11]. The weight was recorded on a weighing scale with standard minimum clothing to the nearest 0.5 kg. To measure height, a vertical scale was used, with the head in the Frankfurt plane and the heel, buttocks, and occiput against the wall, all to the nearest 0.5 cm. All individuals’ BSA and BMI were calculated using the formula below:
BSA (m2) = (Body height in cm) 0.725×(Body weight in kg) 0.425×0.007184 [12];
BMI=Weight (kg)/height (m2) [13];
Cardiac autonomic function tests were done by using a noninvasive Polyrite recording machine (Model number: DSMP0410, RMS, Chandigarh, India) with mode “ECG” in Lead-II position. The time marker was adjusted to 10 seconds. For determination of heart rate with change of posture the time marker with adjustment of 10 seconds was used. All the tests were performed in a comfortable atmosphere with room temperature between 27-30°C. The experiments were conducted in a room with a relative humidity of 60-70% using a temperature and humidity meter (Model number HT-12 Metravi, Kolkata, India). Five minutes rest was given between each test parameter. Experiments were done in accordance with Helsinki Declaration of 1975 that was revised in 2004 [14].
Study description: Resting (Basal) heart rate and blood pressure: The subjects were instructed to lie down in the supine posture, after which lead II of the ECG was recorded while electrodes in the ECG mode are placed to the subject’s appropriate limbs to record the subject’s heart rate (or resting heart rate). Resting heart rate is predominantly controlled by parasympathetic nervous system; hence, measurement of resting heart rate is an index of parasympathetic function test. An oscillometric digital BP monitor (HEM-7134E, Omron, Japan) was used to test the blood pressure in supine position.
Heart rate response to immediate standing (30:15 Ratio): The subjects were instructed to lie down in a supine position and were completely at ease. After that, ECG electrodes were placed, and lead II of the ECG was used to record heart rate while the subjects were in supine posture. To measure the change in heart rate, the participant was asked to stand straight up from a supine position as quickly as possible (within 3 sec) with continuous ECG recording for 30 seconds.
30:15 ratio=Longest R-R interval around 30 beat after immediate standing/Shortest R-R interval around 15th beat after standing.
In the present study, 1.04 and above was taken as normal and less than 1.00 was taken as abnormal response [15].
Blood pressure response to immediate standing after lying (orthostatic test): The participants were asked to rise upright from a supine position after resting measurements (resting heart rate and blood pressure) and the blood pressure was recorded immediately with digital blood pressure apparatus [Table/Fig-1]. In the present study, a mean fall in SBP of 30 mm Hg or more was taken to indicate postural hypotension (abnormal response). Postural fall of SBP of 10 mm Hg or less was taken as normal. And the value 11 to 29 mm Hg was taken as borderline [15,16].
Measurement of blood pressure response to immediate standing.

Blood pressure response to sustained Hand Grip Test (Isometric exercise test): The subjects were instructed to press the handgrip dynamometer (YMRR Hand Grip Dynamometer model no: ARGHC2242, Delhi, India) or 15 seconds at 30% of their maximum voluntary contraction. Blood pressure was recorded just before the release of hand grip and after one minute and five minutes of grip release. Maximum rise in Diastolic Blood Pressure (DBP) above baseline was noted [Table/Fig-2]. The rise in DBP was considered normal if it is 16 or greater, borderline if it is 11 to 15, and abnormal if it is 10 or less as per Ewing’s classification [Table/Fig-3] [17].
Measurement of blood pressure response to sustained handgrip.

Ewing’s cardiac autonomic (sympathetic) function tests.
| Tests reflecting sympathetic function | Normal | Borderline | Abnormal |
|---|
| Blood pressure response to immediate standing {Fall in Systolic Blood Pressure (SBP)} | <10 mmHg | 11-29 mmHg | >30 mmHg |
| Blood pressure response to sustained handgrip {Increase in Diastolic Blood Pressure (DBP)} | >16 mmHg | 11-15 mmHg | <10 mmHg |
| Heart rate response to immediate standing (30:15) ratio | >1.04 | 1.01-1.03 | <1.00 mmHg |
Statistical Analysis
Statistical analysis was carried out using Statistical Package for the Social Sciences (SPSS) software version 17.0 (Chicago, Inc., USA). Results were expressed as mean±SD, and analysed by using unpaired student t-test. The p-value of <0.05 was considered as statistically significant.
Results
There were 100 male subjects participated in our study in two groups (SLT and Passive smokers). The mean age of SLT and passive smokers were 35.84±3.58 and 34.71±2.37, respectively. No significant change was noted statistically in mean age of two groups. Anthropological measures did not show any significant difference between SLT and passive smoking groups. BMI was slightly decreased in SLT group but it was not statistically significant [Table/Fig-4].
Physical characteristics of SLT and passive smokers.
| Variables | SLT(Mean±SD) | Passive smokers (Mean±SD) | t-value | p-value |
|---|
| Age (years) | 35.84±3.58 | 34.71±2.37 | 1.86 | 0.0657 (NS) |
| Height (cm) | 172.37±4.71 | 172.24±2.52 | 0.17 | 0.8637 (NS) |
| Weight (kg) | 71.22±7.49 | 70.90±4.39 | 0.26 | 0.7949 (NS) |
| BMI | 23.68±2.24 | 23.89±1.39 | 0.56 | 0.5745 (NS) |
| BSA (m2) | 1.84±0.09 | 1.83±0.06 | 0.71 | 0.4738 (NS) |
SD: Standard deviation; NS: Not significant
Resting (Basal) heart rate was significantly increased in SLT group (p-value≤0.001) and resting (Basal) SBP was significantly reduced in passive smoker group when compared to SLT group (p-value≤0.001). It was noted that 30:15 ratio was decreased and found to be statistically significant in the passive smokers as compared to that in the SLT group (p-value≤0.001) [Table/Fig-5].
Comparison of study variables among SLT and passive smokers.
| Variables | SLT (Mean±SD) | Passive smokers (Mean±SD) | t value | p-value |
|---|
| Basal Heart rate (beats per minute) | 78.74±1.36 | 75.34±1.22 | 13.15 | ≤0.001 (S) |
| Basal Systolic Blood Pressure (SBP) (mmHg) | 122.44±3.26 | 119.68±7.75 | 4.57 | ≤0.001 (S) |
| Basal Diastolic Blood Pressure (DBP) (mmHg) | 79.24±0.29 | 78.72±2.05 | 1.25 | 0.2121 (NS) |
| Heart rate response to immediate standing (30:15) ratio | 1.20±0.01 | 1.19±0.00 | 7.07 | ≤0.001 (S) |
| Blood pressure response to immediate standing (mmHg) | 7.14±1.49 | 5.68±1.23 | 5.34 | ≤0.001 (S) |
| Blood pressure response to sustained handgrip (mmHg) | 16.52±1.31 | 16.66±1.08 | 0.58 | 0.5612 (NS) |
SD: Standard deviation; NS: Not Significant; S: Significant
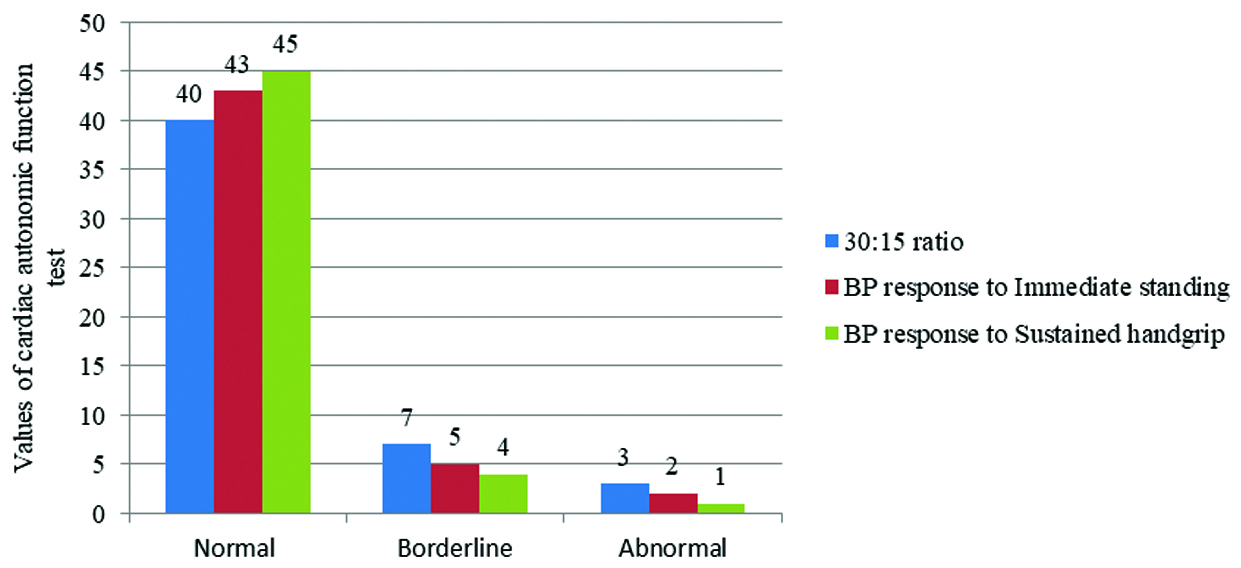
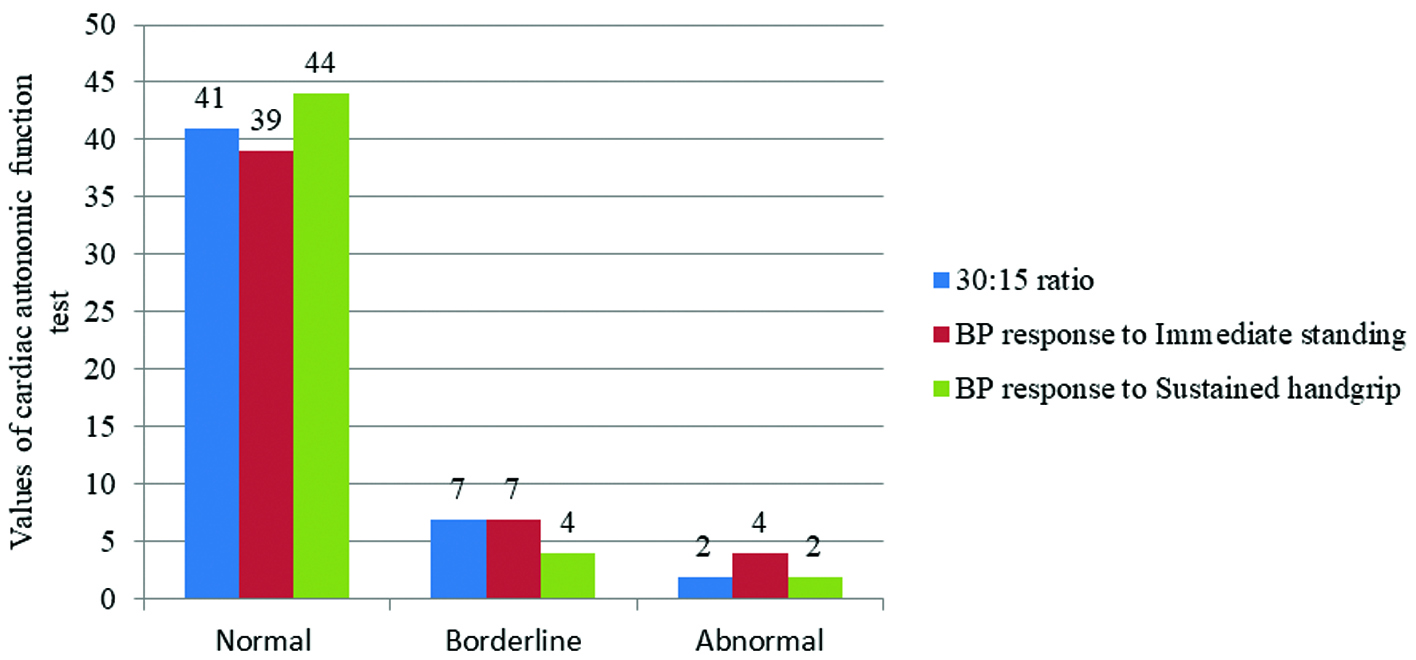
[Table/Fig-6,7] shows normal, borderline and abnormal values in cardiac autonomic function tests based on Ewing’s classification among SLT users and passive smokers, respectively.
Number of SLT participants showing normal, borderline and abnormal values in cardiac autonomic function tests based on Ewing’s classification.
Number of passive smokers showing normal, borderline and abnormal values in cardiac autonomic function tests based on Ewing’s classification.
Discussion
Passive smoke and tobacco use harm the cardio-pulmonary system. The development and progression of cardiac dysfunctions, such as coronary artery disease and endothelial dysfunction, have been linked to passive smoking as a substantial risk factor [18,19]. On the other hand, not much is known about how passive smoking affects cardio-respiratory capacity [20-23]. In our study passive smoking was taken to compare with SLT and noted significant difference. Basal heart rate is generally governed by parasympathetic mechanism. In the present study, basal heart rate is significantly increased in SLT group. This can be linked to the reduced vagal tone that occurs in gutkha chewers due to nicotine usage, even over the brief period of three to five years, which manifests as an acute consequence. This finding is in agreement with Pakkala A et al., who reported that resting heart rate was significantly lower among gutkha chewer in his study [24]. Bolinder GM et al., has also reported increased cardiovascular risk among SLT users [25]. According to Ernster VL et al., SLT use has a positive effect on cardiovascular risk factors in young physically fit men [26]. It may be due to quantity of gutkha usage and frequency. Study from the Sweden reported that higher possibility for cardiovascular mortality was observed among smokeless tobacco customers when compared with non-users [27]. Edwards SW et al., reported that SLT usage significantly increases heart rate among athletes [28].
Basal SBP was increased significantly in SLT group when compared to passive smoking group. This indicated increased sympathetic stimulation. The present study results were in agreement with Goyal K et al., who reported the disturbances in autonomic regulation by increasing sympathetic regulation [29]. The increased blood pressure in SLT consumers is mostly likely due to effect of nicotine. One study shows that consumption of tobacco resulting in tachycardia [30]. The 30:15 ratio or the response to standing is a parameter which is useful for assessing the reactivity of the para-sympathetic system. In the present study, a decrease in the 30:15 ratio was found to be statistically significant in the passive smokers as compared to that in the SLT, thereby indicating a reduced para-sympathetic activity. Tayade MC and Kulkarni NB studied effects of active smoking on cardiac autonomic functions (30:15 ratio) on active smokers and found 30:15 ratio was significantly reduced in active smokers but we reported these effects on passive smokers [31]. Tayade MC and Kulkarni NB have reported significant fall of SBP in active smokers particularly in moderate and heavy smokers [31]. BP levels in passive smokers vary according on the kind and length of their exposure to ambient tobacco smoke. One research article had reported that smoking and endothelial dysfunction are closely related in passive smokers [32]. There were no research publications about postural hypotension with passive smokers. It requires in-depth examination.
Isometric test offers a quick and simple method to stimulate the circulatory system and clarify how the sympathetic nervous system contributes to the workout response. In the present study, isometric handgrip test was not statistically significant. Kotamaki M et al., found that the rise in diastolic pressure was significantly less in active smokers as compared to that in the non-smokers, thus suggesting a decrease in the sympathetic reactivity in them [33]. But in present study passive smoking did not show much effect on diastolic pressure when compared with SLT group. It might be due to subjects with less passive smoking exposure and some environmental factors. This parameter must be studied in large sample size with chronic passive smoking exposure in future to get detailed report.
According to Ewing’s criteria, the cardiac autonomic functions of the SLT and passive smoking group have been classfied as normal, borderline, and abnormal. It was revealed that a large number of participants fell in the normal line. Only few participants show abnormal results. It might be due to short-term exposure of tobacco chewing and passive cigarette smoke, and also due to living environment.
Limitation(s)
Less number of subjects was included. Female subjects were not included due to scarcity of getting expected sample within short duration. Since it was a short term study, the present study doesn’t contain other cardiac autonomic parameters such as Heart Rate Variability (HRV). Further studies assessing complete cardiac autonomic parameters in large number of sample size can be conducted in future.
Conclusion(s)
The fall of SBP in response to immediate standing among passive smokers is suggestive of decreased central sympathetic activity and baroreceptor reflex sensitivity. The present study helps to understand the effects of SLT on autonomic functions and cardio respiratory fitness and also helps to create awareness about preventive measures of SLT and passive smoking. It will give an impact to understand about pathological points s such as cardiac autonomic imbalance.
SD: Standard deviation; NS: Not significant
SD: Standard deviation; NS: Not Significant; S: Significant