The Diabetes Mellitus (DM) is a serious chronic illness that develops when the pancreas is unable to produce enough insulin or when the body is unable to utilise the insulin that is produced. Type 2 diabetes, the most common form, occurs when the body is unable to use insulin effectively [1]. The most recent edition of the International Diabetes Federation’s (IDF) Diabetes Atlas noted that 9.3% of people worldwide currently have diabetes. Due to its high prevalence of diabetes, India is referred to as the global diabetes capital. As of 2020, it was predicted that over 77 million people in India between the ages of 20 and 79 years had diabetes. According to predictions, by 2030, there will be 101 million diabetics in India [2].
The DM is an intense cause of blindness, kidney failure, heart attacks, stroke, and lower limb amputation [3]. Type 2 DM, a major public health concern in India, is characterised by its high prevalence and its impact on individuals’ quality of life. Diabetes is a chronic disease with many complications, including macrovascular issues (such as peripheral artery disease, stroke, and coronary artery disease) and microvascular complications like diabetic retinopathy, neuropathy, and nephropathy. The primary goal of diabetes management is to prevent or reduce the risk of chronic complications associated with the disease [4].
Effective management of DM relies heavily on self-care practices. These practices are crucial for controlling the condition and achieving optimal health outcomes. Self-care practices are characterised as a collection of behavioural strategies used by individuals with diabetes to effectively manage their condition independently. Engaging in self-care improves one’s quality of life and is especially important for preventing diabetes-related complications [5]. Beyond just monitoring blood glucose levels, diabetes care is more complex and necessitates a deeper understanding of the illness. Therefore, a healthy lifestyle-which includes eating a balanced diet, getting regular exercise, quitting smoking, and maintaining a healthy weight- is essential for managing type 2 DM.
Diabetes self-care is hampered by several factors, such as time constraints, perplexing medical information, unethical family values and participation, the cost of care, distance from medical facilities, and cultural differences between the patient and the healthcare professional [6]. Glycaemic control and the avoidance of complications depend heavily on effective self-care behaviours, such as medication adherence, food management, physical activity, glucose monitoring, and foot care [7]. Even with advancements in treatment, a lot of individuals still struggle to adhere to these practices consistently because of a variety of complex issues, including psychological factors, healthcare access, and socioeconomic status [8].
Numerous studies have explored the relationship between self-care practices and outcomes in Type 2 DM patients. These studies have often focused on urban populations or broader geographical regions, examining factors such as age, gender, socioeconomic status, and education about self-care behaviours [9-12]. However, there is a significant gap in the literature regarding the specific challenges and practices of Type 2 diabetes patients in rural areas, particularly in regions like Thiruvallur District, Chennai, Tamil Nadu, India. The need for present study arises from the distinct lifestyle, healthcare access, and cultural factors that may influence self-care practices in rural populations. Understanding these unique factors is crucial for designing effective interventions and support systems tailored to the needs of rural diabetic patients.
The novelty of present study lies in its focus on a rural setting, where the socioeconomic and healthcare dynamics differ significantly from those in urban areas. By addressing the gap in the existing literature, the present research aimed to provide insights that could lead to more effective, context-specific diabetes management strategies in rural regions.
Hence, the aim of the study was to evaluate self-care practices among type 2 DM patients in the rural population of Thiruvallur District and to identify the association between self-care practices and socio-demographic variables, as well as the clinical profile of the patients.
Materials and Methods
A community-based cross-sectional study was carried out from June 2022 to November 2022 (a duration of 6 months) in and around the rural field practice area of ACS Medical College and Hospital in Thiruvallur District, Chennai, Tamil Nadu, India with Institutional Ethical Commitee (IEC) approval number No. 542/2022/IEC/ACSMCH. Informed consent was obtained from the diabetic population before the start of the study.
Inclusion and Exclusion criteria: The study included adults aged 18 years and older with a confirmed diagnosis of Type 2 DM and who have been residing in the rural areas of Thiruvallur District, Tamil Nadu. Individuals who were unable to provide informed consent, those with mental illness, or those unwilling to participate in the study were excluded.
Sample size calculation: A systematic random sampling method was used. The sample size was determined based on a prior study by Karthik RC et al., which indicated a 52.4% prevalence of poor self-care practices [13]. Using an alpha error of 0.05 and a power of 80%, the formula N=(1.96)2PQ/L*L yielded an estimated sample size of 206.
Study Procedure
Data collection tools: Participants were interviewed regarding their diabetic status and various components of self-care practices, as adopted from the SDSCA questionnaire [14]. Random blood glucose levels were measured using a standardised glucometer. Socioeconomic status was determined using the Modified BG Prasad Scale 2023 [15].
Summary of SDSCA score: The SDSCA scale, developed by Toobert, Hampson, and Glasgow in 2000, is a widely used tool that assesses key aspects of diabetes self-management, such as diet, exercise, blood glucose monitoring, foot care, and medication adherence [16]. This scale was selected for the study due to its strong reliability, ease of use, and comprehensive coverage of essential self-care activities. Its validation across diverse populations and frequent use in research make it an ideal choice for assessing self-care practices among Type 2 diabetes patients in rural settings. Although the SDSCA measure is a self-report tool, participants recorded the number of days in the prior week for six domains in this study.
Self-care practices within each domain were graded on a scale of 0 to 7. Better self-care practices were represented by a higher number of days, and to enable comparison in percentage terms, a self-care activity was deemed good if it was performed on the majority of days (more than 5 days) within a week [17].
For diet, exercise, medication compliance, foot care, blood glucose monitoring, and non smoking behaviour, the total number of days recorded as a response for each item in a domain/sub-scale constituted the score. The total score was then calculated by adding all the scores and dividing by the total number of items. Ultimately, each patient’s overall score varied from 0 to 7, with a score of less than 5 being regarded as poor self-care [10]. All participants received a brief explanation of the study’s purpose and were assured of complete confidentiality. The study was conducted using the collected data, which were kept private.
Statistical Analysis
Microsoft Excel was used for data entry, and International Bussines Machine (IBM) Statistical Package for Social Sciences (SPSS) version 25.0 was used for analysis. The study employed a range of statistical analyses to evaluate the SDSCA scale, including Chi-square tests to examine associations between categorical variables, One-way Analysis of Variance (ANOVA) to compare mean scores across different groups, and binomial linear regression analyses to investigate the relationships between self-care activities and various influencing factors.
Results
A total of 206 type 2 DM patients participated in the study. The mean age of the participants was 47±10 years. The study comprised 48.1% of the male population and 51.9% of the female population. The majority of the subjects were married (96.6%). Most of the participants belonged to the age group of 31-50 years (63.6%). A significant portion of the participants had graduated from high school (25.2%), and 60.2% were employed. Most of their housing was classified as semipucca (76.7%) [Table/Fig-1].
Socio-demographic variables of the study group (N=206).
| S. No. | Variables | n (%) |
|---|
| 1. | Age (in years) |
| 18-30 | 10 (04.9) |
| 31-50 | 131 (63.6) |
| 51-65 | 53 (25.7) |
| >65 | 12 (05.8) |
| 2. | Gender |
| Male | 99 (48.1) |
| Female | 107 (51.9) |
| 3. | Religion |
| Hindu | 142 (68.9) |
| Muslim | 29 (14.1) |
| Christian | 35 (17.0) |
| 4. | Qualification |
| Illiterate | 47 (22.8) |
| Primary school | 29 (14.1) |
| Middle school | 18 (08.7) |
| High school | 52 (25.2) |
| Higher secondary | 25 (12.1) |
| Undergraduate | 35 (17.1) |
| 5. | Marital status |
| Married | 169 (82.0) |
| Unmarried | 10 (04.9) |
| Divorced | 12 (5.8) |
| Widowed | 15 (6.8) |
| 6. | Occupation |
| Employed | 124 (60.2) |
| Unemployed | 82 (39.8) |
| 7. | House-type |
| Kutcha | 19 (09.2) |
| Semi pucca | 158 (76.7) |
| Pucca | 29 (14.1) |
| 8. | Socioeconoimc status (BG Prasad Scale) |
| Upper class | 21 (10.2) |
| Upper middle class | 35 (17) |
| Middle class | 68 (33) |
| Lower middle class | 81 (39.3) |
| Lower class | 01 (0.5) |
Among the 206 type 2 DM patients, 56.3% were diagnosed in the age group of 31-40 years, with a positive family history of diabetes noted in 56.8% of cases has been depicted in [Table/Fig-2]. The majority of diabetic patients reported taking medication in the form of tablets only, which accounted for 72.3% of the participants. The study found that 35.4% of participants did not have any history of co-morbidities, followed by those with hypertension (27.2%). Approximately 59.2% of the subjects did not experience any complications, while diabetic retinopathy was the next most common complication, affecting 20.9% of the participants.
Clinical profile of the study participants.
| S. No. | Variables | n (%) |
|---|
| 1. | Age at diagnosis of diabetes (in years) |
| 18-30 | 52 (25.2) |
| 31-50 | 116 (56.3) |
| 51-65 | 21 (10.2) |
| >65 | 17 (8.3) |
| 2. | Duration of diabetes (in years) |
| <1 years | 38 (18.4) |
| 1-5 years | 38 (18.4) |
| 5-10 years | 35 (7.0) |
| >10 years | 95 (46.2) |
| 3. | Family history of diabetes |
| Yes | 117 (56.8) |
| No | 89 (43.2) |
| 4. | Mode of drug intake |
| Tablets only | 149 (72.3) |
| Insulin only | 37 (18) |
| Tablets and insulin | 18 (8.7) |
| None | 2 (1.0) |
| 5. | Comorbidity history |
| Hypertension | 56 (27.2) |
| Asthma | 26 (12.6) |
| OAE knee | 46 (22.3) |
| Others | 5 (2.5) |
| None | 73 (35.4) |
| 6. | Complication history |
| Diabetic retinopathy | 43 (20.9) |
| Diabetic neuropathy | 18 (8.7) |
| Diabetic nephropathy | 9 (4.4) |
| Others | 14 (6.8) |
| None | 122 (59.2) |
| 7. | Glucose control |
| High | 120 (58.3) |
| Normal | 86 (41.7) |
OAE: Osteoarthritis of knee
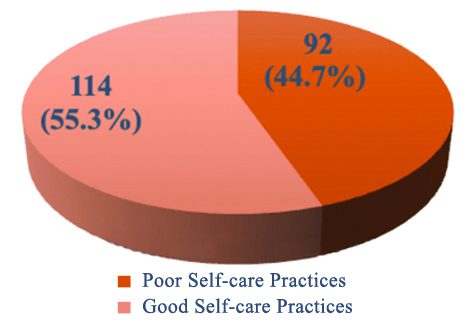
The overall scoring of self-care practices is presented in [Table/Fig-3]. Good self-care practices were observed in 55.3% of the participants, while poor self-care practices were observed in 44.7%.
Overall self-care practices scoring among the study participants (N=206).
The association between self-care practices and various factors is detailed in [Table/Fig-4]. It was found that higher educational qualifications and a shorter duration of diabetes significantly impacted the self-care practice scores (p<0.05).
Factors influencing self-care practices.
| S. No. | Factors | Scores n (%) | p-value |
|---|
| Poor (n=92) | Good (n=114) |
|---|
| 1. | Qualification |
| Illiterate | 32 (68.1) | 15 (31.9) | <0.001* |
| Primary school | 17 (58.6) | 12 (41.4) |
| Middle school | 05 (27.8) | 13 (72.2) |
| High school | 26 (50.0) | 26 (50.0) |
| Higher secondary | 10 (40.0) | 15 (60.0) |
| Undergraduate | 02 (5.7) | 33 (94.3) |
| 2. | Age (in years) |
| 18-30 | 03 (30.0) | 07 (70.0) | 0.004* |
| 31-50 | 50 (38.2) | 81 (61.8) |
| 51-65 | 29 (54.7) | 24 (45.3) |
| >65 | 10 (83.3) | 02 (16.7) |
| 3. | Duration of diabetes |
| <1 year | 14 (36.8) | 24 (63.2) | 0.026* |
| 1-5 years | 10 (26.3) | 28 (73.7) |
| 6-10 years | 19 (54.3) | 16 (45.7) |
| >10 years | 49 (51.6) | 46 (48.4) |
| 4. | Complication history |
| Diabetic retinopathy | 25 (58.2) | 18 (41.8) | 0.018* |
| Diabetic neuropathy | 08 (44.4) | 10 (55.6) |
| Diabetic nephropathy | 05 (55.6) | 04 (44.4) |
| Others | 06 (42.9) | 8 (57.1) |
| None | 48 (39.3) | 74 (60.7) |
| 5. | Socioeconomic status |
| Lower class | 0 | 1 (100) | 0.004* |
| Lower middle class | 41 (50.6) | 40 (49.4) |
| Middle class | 35 (51.5) | 33 (48.5) |
| Upper middle class | 14 (40) | 21 (60) |
| Upper class | 2 (9.5) | 19 (90.5) |
| 6. | Gender |
| Male | 49 (49.5) | 50 (50.5) | 0.218 |
| Female | 43 (40.2) | 64 (59.8) |
| 7. | Family history of diabetes |
| Yes | 53 (45.3) | 64 (54.7) | 0.452 |
| No | 39 (43.8) | 50 (56.2) |
| 8. | Marital status |
| Married | 72 (42.7) | 97 (57.3) | 0.326 |
| Unmarried | 8 (80) | 2 (20) |
| Divorced | 7 (58.3) | 5 (41.7) |
| Widowed | 5 (33.3) | 10 (66.7) |
| 9. | Occupation |
| Employed | 61 (49.2) | 63 (50.8) | 0.261 |
| Unemployed | 31 (37.8) | 51 (62.2) |
| 10. | Age (years) at diagnosis of diabetes |
| 18-30 | 19 (36.5) | 33 (63.5) | 0.153 |
| 31-50 | 53 (45.6) | 63 (54.3) |
| 51-65 | 20 (95.2) | 1 (4.8) |
| >65 | 0 (0) | 17 (100) |
| 11. | Mode of drug intake |
| Tablets only | 43 (28.9) | 106 (71.1) | 0.112 |
| Insulin only | 31 (83.7) | 6 (16.3) |
| Tablets and insulin | 17 (94.4) | 1 (5.6) |
| None | 1 (50) | 1 (50) |
| 12. | Co-morbidity history |
| Hypertension | 11 (19.6) | 45 (80.4) | 0.324 |
| Asthma | 14 (53.8) | 12 (46.2) |
| OAE knee | 21 (45.6) | 25 (54.4) |
| Others | 5 (100) | 0 |
| None | 41 (56.1) | 32 (43.9) |
| 13. | Glucose control |
| High | 90 (75) | 30 (25) | 0.281 |
| Normal | 2 (2.3) | 84 (97.7) |
| 14. | Religion |
| Hindu | 53 (37.3) | 89 (62.7) | 0.486 |
| Muslim | 18 (62) | 11 (38) |
| Christian | 21 (60) | 14 (40) |
| 15. | Type of house |
| Kutcha | 4 (21) | 15 (79) | 0.371 |
| Semipucca | 60 (37.9) | 98 (62.1) |
| Pucca | 28 (96.5) | 1 (3.5) |
The overall adherence to the various self-care practice domains is shown in [Table/Fig-5]. Among diabetics, foot care practices were the least followed of all the domains, with only 95 participants (46.1%) adhering to them. Just 157 patients (76.2%) and 99 patients (48.1%) adequately completed the blood glucose monitoring and physical activity practice domains, respectively. In comparison to other domains, adherence to medication (91.3%) and dietary practices (82.5%) was notably higher.
Domain-wise distribution of self-care practices.
| Self-care practices domain | Adequate n (%) | Inadequate n (%) | Total n (%) |
|---|
| Diet | 170 (82.5%) | 36 (17.5%) | 206 (100%) |
| Physical activity | 99 (48.1%) | 107 (51.9%) | 206 (100%) |
| Foot care | 95 (46.1%) | 111 (53.9%) | 206 (100%) |
| Blood glucose monitoring | 157 (76.2%) | 49 (23.8%) | 206 (100%) |
| Medication adherence | 188 (91.3%) | 18 (8.7%) | 206 (100%) |
| Non smoking behaviour | 86 (41.7%) | 120 (58.3%) | 206 (100%) |
Adequate self-care practices in diet, physical activity, and medication adherence were significantly associated with better glycaemic control, as evidenced by the lower proportion of individuals with high glycaemic control among those with inadequate adherence in these domains (p-values <0.05) has been depicted in [Table/Fig-6]. However, no significant association was found between glycaemic control and foot care, blood glucose monitoring, or non smoking behaviour, suggesting that these practices may not directly influence glycaemic control in this sample.
Association between self-care practices and glycaemic control (N=206).
| Self-care domains | Adherence | Glycaemic control n (%) | p-value |
|---|
| Normal | High |
|---|
| Diet | Inadequate | 18 (50%) | 18 (50%) | 0.017* |
| Adequate | 68 (40%) | 102 (60%) |
| Physical activity | Inadequate | 38 (35.5%) | 69 (64.5%) | 0.040* |
| Adequate | 48 (48.5%) | 51 (51.5%) |
| Foot care | Inadequate | 42 (37.8%) | 69 (62.2%) | 0.257 |
| Adequate | 44 (46.3%) | 51 (53.7%) |
| Blood glucose monitoring | Inadequate | 20 (40.8%) | 29 (59.2%) | 0.508 |
| Adequate | 66 (42%) | 91 (58%) |
| Medication adherence | Inadequate | 9 (50%) | 9 (50%) | 0.049* |
| Adequate | 77 (41%) | 111 (59%) |
| Non smoking behaviour | Inadequate | 23 (19.1%) | 97 (80.9%) | 0.61 |
| Adequate | 63 (73.2%) | 23 (26.8%) |
*p-value less than 0.05 was considered as significant
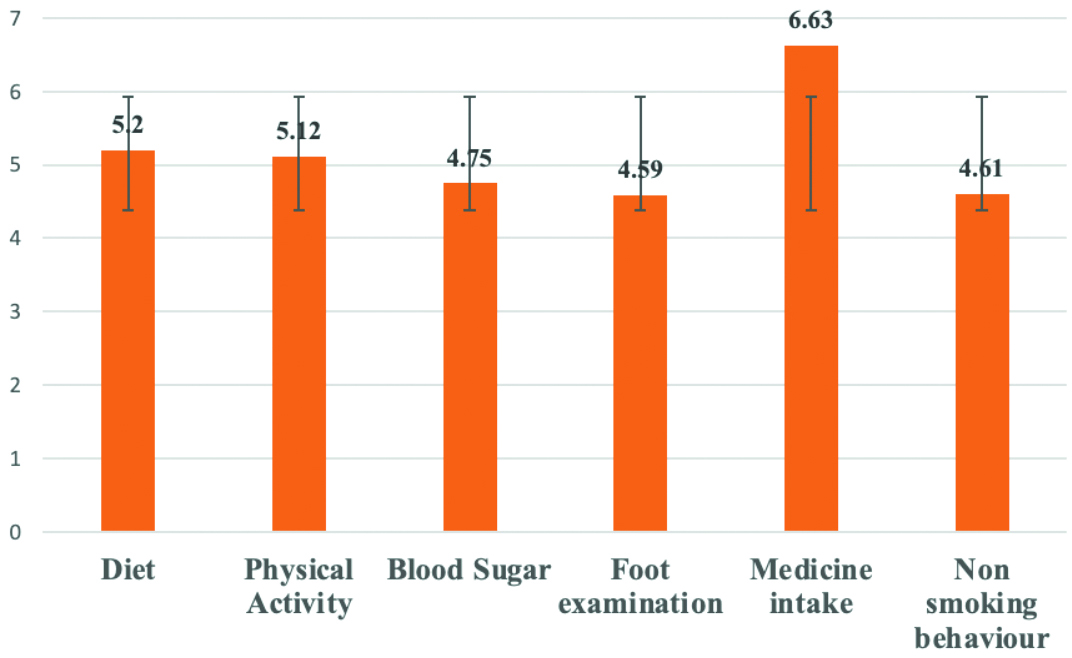
The mean scores for six domains related to the Summary of Diabetes Self-Care Activities (SDSCA), highlighting varying levels of consistency among participants has been depicted in [Table/Fig-7]. The highest mean score was observed in medication intake, with a score of 6.63±1.06, indicating that participants were diligent in taking their prescribed medications. Diet and physical activity followed with scores of 5.2±0.96 and 5.12±1.58, respectively, while monitoring blood sugar levels and non smoking behaviour had lower mean scores of 4.75±1.59 and 4.61±1.27. Foot examination had the lowest mean score of 4.59±2.33, suggesting that this critical health behaviour is often neglected.
Mean scores of all the domains of SDSCA.
A binary logistic regression was carried out and showed that individuals with a higher secondary school qualification exhibited significantly greater self-care adherence compared to those with only a high school qualification. Additionally, a history of diabetic neuropathy and nephropathy also significantly increased the odds of self-care adherence, with neuropathy showing an Odds Ratio (OR) of 7.135 (95% CI: 1.544-32.980, p=0.012) and nephropathy showing an OR of 3.970 (95% CI: 1.297-12.158, p=0.016). The regression analysis did not show statistical significance for variables like age (p=0.177), socio-economic status classification (p=1.00), and duration of diabetes (p=0.257) [Table/Fig-8].
Binary logistic regression analysis of variables with self-care adherence.
| Variables | p-value | Odd’s ratio | 95% Confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| Qualification |
| High school | 0.035 | 3.900 | 1.103 | 13.791 |
| Higher secondary school | <0.001 | 52.049 | 9.066 | 298.832 |
| Complication history of diabetes |
| Diabetic neuropathy | 0.012 | 7.135 | 1.544 | 32.980 |
| Diabetic nephropathy | 0.016 | 3.970 | 1.297 | 12.158 |
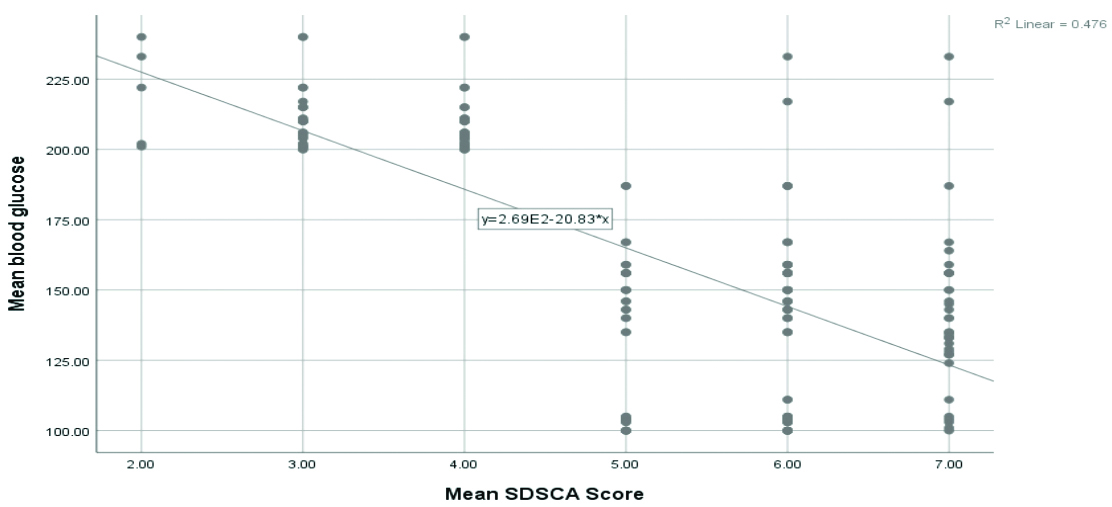
The scatter plot in [Table/Fig-9] illustrates a negative correlation between the mean SDSCA score and mean blood glucose levels, as indicated by the downward trend of the regression line. The R2 value of 0.476 indicates that approximately 47.6% of the variability in blood glucose levels can be explained by the variability in SDSCA scores, suggesting that higher adherence to self-care activities is associated with lower blood glucose levels (R=0.690, p<0.001).
Linear regression between mean blood glucose levels and mean SDSCA scores.
Discussion
The present study, which primarily examined the self-care practices of patients with type 2 DM, was carried out in the rural field practice area of a tertiary medical college in the Thiruvallur district. According to the analysis, 55.3% of participants in present survey reported engaging in good self-care activities, while 44.7% reported poor self-care practices. In comparison, a study by Shivananda R et al., in Karnataka found that 44.6% of individuals engaged in poor self-care habits [18]. Another study by Molalign Takele G et al., in the Tigray region of Ethiopia revealed that approximately 46.7% of participants practiced good self-care [19].
In the current study, the quality of self-care routines began to deteriorate as individuals aged, which is consistent with findings from studies conducted by Durai V et al., and Ahmad F et al., [20,21]. When comparing the duration of diabetes with self-care practices, this study found that as the duration increased, the quality of practices declined from good to poor. This contradicts a study by Uma Maheshwari R et al., among diabetes patients attending primary health centres in the Thiruvallur district, which showed that as the duration increased, participants maintained good self-care practices [22].
A cross-sectional study done by Sekhar CC et al., among the rural community in Parla found that most participants (43.5%) belonging to the lower middle class had poor self-care practices. In contrast, the present study found that participants classified as middle class according to the BG Prasad Socioeconomic Status Scale exhibited good practices [23]. Approximately 117 participants (56.8%) in our study had a positive family history of diabetes. The present study also found that higher educational status was associated with better self-care practices, which is contrary to the study conducted in Pakistan by Ansari RM et al., which indicated that participants with no formal education were more likely to adhere to self-care practices [24]. Additionally, the present study found that adequate medication adherence is strongly associated with glycaemic control, which is similar to previous studies that have established that adherence to medication has a positive influence on glycaemic control in patients with type 2 DM [25,26].
A domain-wise comparison of self-care practices reveals notable variations across different studies. In the present study, medication intake had the highest mean score (6.63±1.06), while foot examination had the lowest (4.59±2.33), indicating varying adherence levels to self-care practices, with foot examination being the most neglected. In contrast, a study conducted in Puducherry by Arulmozhi S and Thulasingam M highlighted inadequate self-care practices related to dietary management and physical activity among Type 2 diabetes patients, which mirrors findings from Kumar M et al., who reported similar deficiencies in dietary adherence and exercise in a tertiary care hospital in India [4,27]. Conversely, Patel S et al., observed higher adherence to blood glucose monitoring in their study, indicating regional differences in self-care practices and their implementation [28]. Singh S et al., Jannoo Z et al., and Kumar A et al., reported that comprehensive self-care practices, including medication adherence and regular physical activity, were associated with improved glycaemic control in their research, underscoring the positive impact of effective self-care [5,29,30]. These findings suggest that while some regions may struggle with certain aspects of diabetes management, others may show strengths in different areas, highlighting the need for localised and tailored self-care interventions [31].
The key strength of present study lies in its comprehensive approach to diabetic self-care and its practical relevance to the target population. This study emphasises the disparities in eating habits and other self-care behaviours. It demonstrates that it is easier to break a nutritional habit than to pick up new ones; thus, physicians should provide easy-to-follow, accessible, and culturally appropriate dietary recommendations. There are fewer individuals giving up tobacco use compared to those quitting drinking or smoking, possibly because medical practitioners did not inquire sufficiently about tobacco use (including smokeless forms). To sustain motivation among Type 2 DM patients in rural Thiruvallur District, it is essential for doctors and laboratory technicians to regularly communicate target values for key health metrics. This ongoing feedback helps patients better understand their progress and encourages adherence to self-care practices. The present literature reveals that diabetes self-care practices are the foundation of diabetes care. It is widely accepted that self-management is significant in controlling and preventing complications associated with the disease. Despite the benefits associated with diabetes self-management, research has shown that most patients do not adhere to self-management recommendations.
Limitation(s)
The cross-sectional design of present study limits the ability to establish causal relationships, and the focus on a single rural area may restrict the applicability of the findings to other regions.
Conclusion(s)
The present study focused on evaluating self-care practices among patients with Type 2 DM in the rural regions of Thiruvallur District, Tamil Nadu. The results reveal that while some patients are diligent in certain self-care behaviours, such as medication adherence, significant gaps remain in other areas, like dietary management, physical activity, and routine health monitoring. The findings highlight the urgent need for targeted interventions to address these shortcomings, particularly in rural settings where access to healthcare resources and health literacy are often limited. The study emphasises the essential role of healthcare professionals in providing continuous education and support, which are crucial for empowering patients to manage their condition effectively. Strengthening self-care practices through tailored education and ongoing guidance is vital for improving the long-term health outcomes of individuals with Type 2 diabetes in rural communities.
OAE: Osteoarthritis of knee
*p-value less than 0.05 was considered as significant