Postural stress to the upper body for prolonged durations can lead to upper cross syndrome [1]. The increasing cases of upper cross syndrome has raised concerns among healthcare professionals regarding the need for early identification and prevention of secondary complications arising from it. Therefore, there is a need to develop a valid and reliable tool that can provide a better understanding of this syndrome. Upper cross syndrome occurs due to muscular imbalances between tonic and phasic muscles [2,3]. The tonic muscles, which maintain posture, tend to become shortened and tight, while the phasic muscles, responsible for movement, become weak [1]. Upper cross syndrome is characterised by a forward head posture, slouched or rounded shoulders, an increased upper thoracic kyphotic angle, protracted shoulders, anterior tilting, and winging of the scapula [4,5]. This condition can lead to headaches, pain, and limitations in the neck, shoulder, and upper back [6,7].
The early identification of upper cross syndrome at an early stage is difficult, as the diagnosis depends on the clinician’s individual judgment [8]. Many a times, it remains asymptomatic, but when prolonged, individuals may experience neck and upper back pain [9]. It can go undiagnosed for a long duration of time. Early identification and treatment can prevent further secondary complications. While various valid and reliable tools are available for postural assessment, like REEDCO Posture Score (REEDCO) and the New York Posture Rating Chart [10,11], there are no proper diagnostic criteria specifically for identifying upper cross syndrome [6]. There is a paucity of reliable and valid tools to identify this syndrome. In order to fill the gap, a valid and reliable tool was developed to identify upper cross syndrome. For a tool to be valid, it is crucial to establish content validity [12]. Content validity represents the relevance and true representation of the items concerning the construct being measured [13,14]. Content validity can be evaluated using the CVI, which is one method for quantifying it [13-15]. The construct validity and reliability of the tool were also established [16].
The objective of this study was to develop a tool that will help identify upper cross syndrome, ultimately improving postural dysfunction and the quality of life for individuals affected by upper cross syndrome.
Materials and Methods
This cross-sectional study was carried out in Amity Institute of Health Allied Sciences, Department of Physiotherapy, Amity University, Noida, Uttar Pradesh, India, between November 2023 and March 2024. Ethical consent for the study was obtained from Amity University Noida (AUUP/IEC/JUN/2022/6). The study was conducted in accordance with the Helsinki Declaration. Informed consent was obtained from each participant prior to data collection. The CTRI registration number for the trial is (CTRI/2022/10/046611).
The study was divided into phases: the first part was the instrument design phase, and the second phase was the judgment phase [14]. This was followed by statistical analysis.
Phase I- Instrument Design Phase
The process involves determining the content domain, item generation, and construction of the instrument. The content domain is the content that the instrument is designed to measure [14]. In this study, the content domain and item pool were generated through an extensive review of the literature and focus group discussions. Various data-based search engines, like PubMed, ScienceDirect, and Google Scholar, was used. Focus group discussions was carried with six experts (2 physiotherapists, 1 physician, 1 orthopaedic surgeon, 2 occupational therapists) who had at least 10 years of experience and a special interest in spine and posture. Based on the literature review, the moderator posed questions related to the research problem. The experts shared their ideas and perspectives, while the moderator took notes. Two sessions, each lasting one hour, were conducted, and no further ideas were generated. Consequently, the item pool was created.
The item pool consists of the following domains: Postural Alignment Domain (four items), Movement Pattern Domain (four items), Muscle Imbalance Domain (five items), Joint Dysfunction Domain (five items), Pain Domain (five items), Functional Limitation Domain (nine items), and Psychosocial Domain (five items). Based on this information, a conceptual framework for upper cross syndrome was prepared. All standard guidelines for tool development were followed [17].
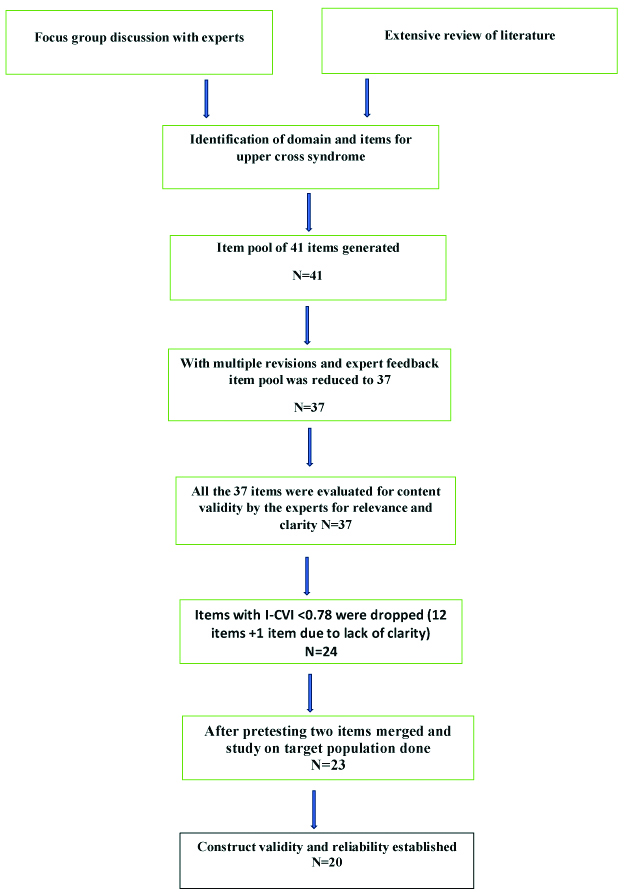
An initial pool of 41 items was identified and was again reviewed by experts, it was further reduced to 37 items. Closed-ended questions were then prepared for further judgement by the experts [Table/Fig-1].
| Postural alignment |
| 1. Is the craniovertebral angle decreased? |
| 2. Is the kyphotic angle increased? |
| 3. Are the shoulders rounded? |
| 4. Is there any asymmetry in scapula? |
| Movement pattern |
| 5. Is there any scapular dyskinesis? |
| 6. Is there any difficulty doing pecking movement? |
| 7. Is there any observed pattern of winging, excessive scapular upward rotation, shrugging or protraction while doing Wall Push up? |
| 8. Is the Scapulohumeral rhythm altered? |
| Muscle imbalance |
| 9. Is there any tightness in the following muscles? Pectoralis major, pectoralis minor, levator scapulae, sternocleidomastoid. |
| 10. Is there a decrease in the endurance of deep neck muscles? |
| 11. Is there a decrease in the strength of neck muscles? |
| 12. Is there a decrease in the strength of shoulder muscles? |
| 13. Is there a decrease in the strength of scapular muscles? |
| Joint dysfunction |
| 14. Is there any restriction in cervical range of motion? |
| 15. Is there any restriction in shoulder range of motion? |
| 16. Is there any decreased mobility of thoracic spine? |
| 17. Is there any decreased opening of mouth? |
| 18. Is the cervical joint position sense altered? |
| Pain |
| 19. Do you have any neck/neck shoulder pain/upper limb pain? |
| 20. Do you have any thoracic pain? |
| 21. Do you have any jaw pain? |
| 22. Do you have any headache? |
| 23. Are the trigger points present? |
| Functional limitation |
| 24. Do you feel difficulty in doing tasks at house? |
| 25. Do you feel difficulty in doing tasks at jobs? |
| 26. Do you feel fatigue in the neck and arm? |
| 27. Do you feel any pins or needle sensation in the arm? |
| 28. Is the chest expansion reduced? |
| 29. Is the peak expiratory flow rate or the maximum flow rate generated during forceful exhalation, reduced? |
| 30. Do you feel any tightness in the chest? |
| 31. Do you feel any dizziness during neck movement? |
| 32. Is your static/dynamic balance altered? |
| Psychosocial factors |
| 33. Do you have low self-esteem due to poor body posture? |
| 34. Do you have dissatisfaction towards your poor body posture? |
| 35. Do you have poor sleeping pattern? |
| 36. Do you avoid social gathering? |
| 37. Do you have any anxiety or stress? |
(if present Yes-1, if absent No-0)
Instrument construction is the third step, in which the items are refined and organised in a suitable format and sequence. Each item was distributed under the appropriate domain based on clinical relevance. A scoring system was developed (Present-Yes, Absent-No) to identify the presence or absence of each item within the domain. Each item was rated on a dichotomous scale: Yes-(1), No-(0).
Phase II- Judgement Phase
In this phase, expert opinions were collected through Delphi rounds. The Delphi method is a procedure for gathering opinions on a research problem. In this approach, a question is formulated, followed by the collection of expert opinions and analysis of responses. Through an iterative process, the individual responses are transformed into a consensus by the group, without revealing the participants’ identities or confidentiality [18,19]. Experts were selected based on their knowledge and expertise, with a focus on multidisciplinary professionals who had more than 10 years of clinical experience.
An invitation letter was sent to 20 experts; of those, 15 accepted the invitation and agreed to participate in the study. The group included two orthopaedic surgeons, one physician, six physiotherapists, and six occupational therapists. Experts received a cover letter along with a questionnaire and were asked to rate each item on a Likert scale based on two criteria: clarity and relevance. The first Delphi round was then conducted [14].
The ratings for relevance were as follows: Not relevant (1); Somewhat relevant (some revision needed-2); Quite relevant (minor revision needed-3); Very relevant (no revision needed-4) [14]. The ratings for clarity were: Not clear (1); Some revision needed (2); Minor revision needed (3); Very clear (4) [14].
A separate column was provided for expert feedback, including a comments and suggestions section. The feedback was subsequently used to modify the tool. In the first step, items were rated according to the aforementioned criteria. Later, the items were categorised into a dichotomous variable: 0 for non relevant and 1 for relevant. Items rated 3 and 4 were assigned a value of 1, while items rated less than 3 were marked as 0.
During the instrument development process, the most widely used method is the calculation of the CVI [19]. The process of developing a new tool’s content validity is crucial because it transforms an abstract concept into a measurable and observable value [20].
Process of content analysis and validity: The Item Content Validity Index (ICVI) was calculated by dividing the number of agreements (rated 3 and 4) by the experts by the total number of participants. Analysis was done for all items. We applied the criteria of I-CVI ≥0.78 and an average CVI of ≥0.9, using a 95% confidence threshold recommended by Polit DF and Beck CT [13]. A cut-off of <0.78 was established for the deletion of items [13,14]. There was a separate comment section for each item, allowing experts to provide feedback and inputs for further modifications. We repeated this iterative process until no further modifications were necessary. A total of three Delphi rounds were done. I-CVI index and S-CVI for items were calculated [Table/Fig-2].
Flow chart of tool development on upper cross syndrome (N=Number of items).
Inclusion criteria: A cross-sectional study was conducted with 240 participants suffering from upper cross syndrome, including both males and females aged 18 to 50 years were included in the study.
Exclusion criteria: Individuals with malignancy, congenital deformities, scoliosis, fractures, a history of surgeries, pregnancy, or vertebral basilar insufficiency were excluded from the study.
Sample size: The sample size was calculated based on the number of items; it is recommended to have 10 participants per item [17]. With 24 items, the sample size becomes 240. The parameters evaluated included postural alignment, movement patterns, muscle imbalance, joint dysfunction, pain, functional limitations, and psychosocial factors. The materials required for the study included a camera, Kinovea software (for postural alignment), an inch tape (for muscular tightness/chest expansion), an inclinometer (for kyphotic angle), a goniometer (for joint range of motion), and a peak flow meter (for peak expiratory flow rate). Additionally, manual muscle testing was used to assess muscle strength, while movement patterns was tested by observation.
The construct validity was computed using factor analysis with Varimax rotation [16]. The goal was to sort similar items into factors. Items with similar characteristics were grouped into factors, and inter-related items formed clusters known as factors. Eigenvalues represent the amount of variance each factor accounts for. We retrieved factors with eigenvalues greater than 1 [21] and items with factor loading greater than 0.4. The Kaiser-Meyer-Olkin (KMO) measure and Bartlett’s test were conducted to assess sample adequacy and the correlation matrix [16].
A Cronbach’s Alpha of 0.7 was considered while estimating the tool’s reliability using the internal consistency metric [22]. At a 14-day interval, test-retest reliability was computed using the identical sample. The measurement of test-retest reliability was done using the Intraclass Correlation Coefficient (ICC). ICCs are measured in intervals of 0.00 to 1.00, where values above 0.80 denote exceptional reliability, and values between 0.60 and 0.80 indicate good reliability [23]. In total, 24 items were retained for further analysis.
Pretesting was done to ascertain if there were any difficulties in delivering the instrument to the target group [17]. Based on the respondents’ responses, the tool was modified to improve its simplicity, accuracy, and the time required to complete it.
Statistical Analysis
Statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS) software (Version 21.0, IBM Corporation, Armonk, NY, USA) and Microsoft Excel 2010. The Item-Level Content Validity Index (I-CVI) was calculated, and the overall Scale-Level Content Validity Index (S-CVI) was calculated. Factor identification was done using exploratory factor analysis. Additionally, Cronbach’s alpha and test-retest reliability were computed.
Results
Content validity and pretesting: Items with an I-CVI <0.78 were eliminated following content validity testing conducted with 15 experts. As a result, 12 items were removed from the initial draft, and one item (Item 20) was deleted due to a lack of clarity. As a result, 24 items with a S-CVI of 0.90 were retained for further analysis [Table/Fig-3]. Pretesting of the final draft was done on 10 patients to assess the feasibility and applicability of the instrument. Further changes were made during the pretesting phase, and two questions that were identical to one another were combined into one item (Difficulty in doing household chores, Item 24, and Difficulty in doing tasks at work, Item 25). The final draft was reduced to 23 items.
Content validity and interpretations.
| Items | Total no of experts=15 | Agreement among experts | I-CVI | Interpretations |
|---|
| 1. Is the craniovertebral angle decreased? | 15 | 15 | 1 | Appropriate |
| 2. Is the kyphotic angle increased? | 15 | 15 | 1 | Appropriate |
| 3. Are the shoulders rounded? | 15 | 15 | 1 | Appropriate |
| 5. Is there any scapular dyskinesis? | 15 | 15 | 1 | Appropriate |
| 7. Is there any observed pattern of winging, excessive scapular upward rotation, shrugging or protraction while doing Wall Push up? | 15 | 15 | 1 | Appropriate |
| 9. Is there any tightness in the following muscles? Pectoralis major, pectoralis minor, Levator scapulae Sternocleidomastoid. | 15 | 15 | 1 | Appropriate |
| 10. Is there a decrease in the endurance of deep neck muscles? | 15 | 15 | 1 | Appropriate |
| 11. Is there a decrease in the strength of neck muscles? | 15 | 14 | 0.933 | Appropriate |
| 12. Is there a decrease in the strength of shoulder muscles? | 15 | 15 | 1 | Appropriate |
| 13. Is there a decrease in the strength of scapular muscles? | 15 | 15 | 1 | Appropriate |
| 14. Is there any restriction in Cervical range of motion? | 15 | 15 | 1 | Appropriate |
| 15. Is there any restriction in Shoulder range of motion? | 15 | 15 | 1 | Appropriate |
| 16. Is there any decreased mobility of thoracic spine? | 15 | 14 | 0.933 | Appropriate |
| 17. Is there any decreased opening of mouth? | 15 | 15 | 1 | Appropriate |
| 19. Do you have any neck/neck shoulder pain/upper limb pain? | 15 | 15 | 1 | Appropriate |
| 20. Do you have any thoracic Pain?† | 15 | 15 | 1 | Appropriate |
| 22. Do you have any headache? | 15 | 14 | 0.933 | Appropriate |
| 23. Are the trigger point present? | 15 | 13 | 0.866 | Appropriate |
| 24. Do you feel difficulty in doing tasks at house? | 15 | 14 | 1 | Appropriate |
| 25. Do you feel difficulty in doing tasks at jobs? | 15 | 14 | 1 | Appropriate |
| 26. Do you feel fatigue in the neck and arm? | 15 | 14 | 1 | Appropriate |
| 28. Is the chest expansion reduced? | 15 | 13 | 1 | Appropriate |
| 29. Is the Peak expiratory flow rate or the maximum flow rate generated during forceful exhalation, reduced? | 15 | 15 | 1 | Appropriate |
| 33. Do you have low self-esteem due to poor body posture? | 15 | 15 | 1 | Appropriate |
| 34. Do you have dissatisfaction towards your poor body posture? | 15 | 15 | 1 | Appropriate |
| Items 4, 6, 8, 18, 21, 27, 30, 31, 32, 35, 36, 37* | 15 | 11 | 0.73 | Deleted |
| | SCVI | 0.90 | |
*Items having I-CVI <0.78 were deleted [13]; †Item 20 was also deleted due to lack of clarity, the experts were not clear about the precise area of involvement in the thoracic region; ‡I-CVI (item level content validity index)
Overall, 240 patients (10 patients for pretesting and 230 patients for the final analysis) were enrolled in the study. A psychometric analysis was performed, and [Table/Fig-4] provides demographic information.
Demographic details of the population.
| Gender | n (%) | Cumulative percent |
|---|
| Male | 129 (53.8) | 53.8 |
| Female | 111 (46.2) | 100 |
| Age groups (years) |
| 18-20 | 38 (15.8) | 15.8 |
| 21-30 | 81 (33.8) | 49.6 |
| 31-40 | 53 (22.1) | 71.7 |
| 41-50 | 68 (28.3) | 100 |
| Total | 240 (100) | |
Out of 37 items, 12 items were removed as per criteria and one item was removed due to lack of clarity. As a result, only 24 items were left. Moreover, during pretesting two items were merged into one item due to similarity between them and only 23 items were left for final analysis
Acceptability: The instrument was reportedly well-received by clinicians, and there were no issues with comprehension or interpretation. The percentage of a missing responses was calculated by dividing the number of missing responses by the total score and multiplying the result by 100. The instrument was completed in 20-25 minutes.
Validity and reliability: Bartlett’s test was significant with a p-value of <0.0001, and the Kaiser-Meyer-Olkin (KMO) test resulted in a value of 0.83, indicating that the sample size is sufficient for factor analysis. Applying Varimax rotation produced a total variance of 60.111% and identified a seven-factor structure based on eigenvalues greater than 1 [Table/Fig-5,6]. Cronbach’s alpha was found to be 0.81, indicating a significant result. Test-retest reliability yielded excellent findings, measuring 0.83 [Table/Fig-7].
Factor loading matrix of the items with Cronbach’s α.
| Items | Factor loading |
|---|
| D1 | D2 | D3 | D4 | D5 | D6 | D7 | Cronbach’s α |
|---|
| 1. Is the craniovertebral angle decreased? | 0.834 | | | | | | | 0.901 |
| 2. Is the kyphotic angle increased? | 0.643 | | | | | | | |
| 3. Are the shoulders rounded? | 0.536 | | | | | | | |
| 4. Is there any scapular dyskinesis? | | 0.754 | | | | | | 0.976 |
| 5. Is there any observed pattern of winging, excessive scapular upward rotation, shrugging or protraction while doing Wall Push up? | | 0.766 | | | | | | |
| 6. Is there any tightness in the following muscles?Pectoralis major, pectoralis minor, Levator scapulae, Sternocleidomastoid. | | | 0.572 | | | | | 0.781 |
| 7. Is there a decrease in the endurance of deep neck muscles? | | | 0.756 | | | | | |
| 8. Is there a decrease in the strength of neck muscles? | | | Deleted | | | | | |
| 9. Is there a decrease in the strength of shoulder muscles? | | | 0.804 | | | | | |
| 10. Is there a decrease in the strength of scapular muscles? | | | 0.822 | | | | | |
| 11. Is there any restriction in Cervical range of motion? | | | | 0.685 | | | | 0.78 |
| 12. Is there any restriction in shoulder range of motion? | | | | 0.47 | | | | |
| 13. Is there any decreased mobility of thoracic spine? | | | | 0.426 | | | | |
| 14. Is there any decreased opening of mouth? | | | | Deleted | | | | |
| 15. Do you have any neck/neck shoulder pain/upper limb pain? | | | | | 0.448 | | | 0.756 |
| 16. Do you have any headache? | | | | | 0.468 | | | |
| 17. Are the trigger point present? | | | | | 0.429 | | | |
| 18. Do you feel difficulty in doing tasks at house/jobs? | | | | | | 0.462 | | 0.74 |
| 19. Do you feel fatigue in the neck and arm? | | | | | | Deleted | | |
| 20. Is the chest expansion reduced? | | | | | | 0.441 | | |
| 21. Is the Peak expiratory flow rate or the maximum flow rate generated during forceful exhalation, reduced? | | | | | | 0.597 | | |
| 22. Do you have low self-esteem due to poor body posture? | | | | | | | 0.494 | 0.721 |
| 23. Do you have dissatisfaction towards your poor body posture? | | | | | | | 0.441 | |
*Factor loading more than 0.4 were taken [23]
Eigenvalue with total variance.
| Factor | Eigenvalue | Percentage of variance | Total variance (%) |
|---|
| Factor 1 | 6.139 | 17.54 | 60.111 |
| Factor 2 | 2.799 | 7.998 | |
| Factor 3 | 2.181 | 6.23 | |
| Factor 4 | 2.016 | 5.671 | |
| Factor 5 | 1.747 | 4.99 | |
| Factor 6 | 1.383 | 3.953 | |
| Factor 7 | 1.273 | 3.683 | |
*Eigenvalue more than 1 [23]
Intra-class Correlation Coefficient (ICC) of domains.
| Domain | ICC | CI (95% class interval) |
|---|
| Postural alignment | 0.906 | 0.821-0.951 |
| Movement pattern | 0.976 | 0.971-0.980 |
| Muscular Imbalance | 0.781 | 0.781-0.809 |
| Joint dysfunction | 0.78 | 0.781-0.809 |
| Pain | 0.76 | 0.497-0.873 |
| Functional limitation | 0.742 | 0.498-0.868 |
| Psychosocial factors | 0.709 | 0.442-0.849 |
| Overall reliability | 0.83 | |
Discussion
The main objective of present study was to develop a tool for identifying upper cross syndrome and to establish the tool’s validity and reliability. A tool was validated by calculating the I-CVI, S-CVI, and assessing construct validity. Cronbach’s alpha was used to evaluate reliability. To the best of our knowledge, no tool has been developed to identify upper cross syndrome until now. The development of this tool will further aid in the identification and early intervention of upper cross syndrome.
Good posture reflects the physical and emotional wellbeing of an individual [24]. It reduces pain, fatigue, and stress on the muscles, ligaments, and joints, and reduces the chances of injury [25]. The Reedco Posture Analysis Scale is a standard assessment tool used to analyse posture, featuring a scoring system that grades posture from head to toe [26]. However, this tool does not include patient-based outcome measures like pain and functional limitations. This tool adds to the level of evidence by contributing various domains that will help clinicians plan treatment strategies tailored to the patient’s specific problems. This approach will open the door to various corrective measures that can help prevent secondary complications.
In one study, upper body postures were assessed using a three-dimensional back scan with the Video rasterstereography Back Mapper [25]. Reflective markers were placed on the skin surface, and the data was captured by cameras positioned at defined angles. The limitations of this tool include its limited availability in clinical settings and the requirement for trained individuals to perform standardised procedures. One of the major strengths of present study was the development of a novel tool that will be easy to use and does not require any prior training or expertise.
The majority of posture assessment measures [10,11,26] have emphasised body alignment, but none have focused on improper movement patterns or muscle activation. The inclusion of these domains will not only correct faulty movement patterns but also improve the functional performance of individuals affected by this syndrome.
The main cause of upper cross syndrome is persistent stress on the upper body [1]. This causes muscle imbalances at the cervical and shoulder joints, which can result in dysfunction of the glenohumeral, atlanto-occipital, and cervical spine joints [6]. Symptoms in one joint can impact the function of other joints [26]. This can be prevented by recognising and re-educating individuals on correct posture.
An important domains of this tool was the inclusion of psychosocial factors. Good posture is strongly associated with self-confidence [27]. Posture can affect self-esteem to some extent, which could impact personal life and social interactions [28]. It is well acknowledged that posture plays a part in identifying affect and that emotion plays a crucial role in the development of social behaviour [29]. A key strength of this tool was that each domain was related to the International Classification of Functioning, Disability, and Health [30].
The creation of this tool using a biopsychosocial approach will act as a guide and assist clinicians in developing a comprehensive understanding and formulating plans for correction and the avoidance of future complications [31].
Limitation(s)
The fact that the tool’s validation was done only through content validity and construct validity is noteworthy. With a larger sample size, it would be possible to compute the validity using additional methods, including concurrent validity and criterion validity. Present study used a dichotomous screening of categories rather than a weighted contribution, which could have provided clinicians with more insight for planning rehabilitation strategies based on actual evidence. Future studies could focus on translating this tool into other languages and validation can be done respectively.
Conclusion(s)
The aim of the study was to develop a valid and reliable tool for identifying upper cross syndrome. A novel tool was developed to identify upper cross syndrome. The present study adds to existing knowledge by providing healthcare professionals with a better understanding of how to identify upper cross syndrome and design early rehabilitation plans. This will further aid in correction upper cross syndrome and preventing secondary complications. This tool encourages postural awareness both in the community and among individuals. People with good posture are likely to perform better both physically and mentally.
*Items having I-CVI <0.78 were deleted [13]; †Item 20 was also deleted due to lack of clarity, the experts were not clear about the precise area of involvement in the thoracic region; ‡I-CVI (item level content validity index)
Out of 37 items, 12 items were removed as per criteria and one item was removed due to lack of clarity. As a result, only 24 items were left. Moreover, during pretesting two items were merged into one item due to similarity between them and only 23 items were left for final analysis
*Factor loading more than 0.4 were taken [23]
*Eigenvalue more than 1 [23]