Stroke is the third most common cause of disability and the second most common cause of death worldwide [1,2]. Following a stroke, a large number of individuals frequently require rehabilitation because to lingering deficits linked to hemiparesis, upper-limb dysfunction, pain, decreased balance, swallowing, and vision, neglect, and problems with mobility, activities of daily living, and communication [3]. Hemineglect, also referred to as unilateral neglect, neglect, hemispatial neglect, spatial neglect, or contralateral neglect, is a condition whereby patients are unable to report, respond to, or orient themselves to significant stimuli in the opposite side of space following a brain lesion that cannot be attributed to sensory or motor dysfunction [4]. Hemispatial neglect is a frequent outcome of stroke, especially after right-hemisphere brain damage, with a reported prevalence of over 80% after injuries to the right middle cerebral artery [5]. A brain damage to the right hemisphere, more specifically the posterior parietal cortex, is known to cause hemineglect syndrome, which is characterised by spatial disorientation on the non-dominant side (usually the left-side). Biased line bisection and extinction are caused by defects in the posterior-inferior region and involvement of the temporoparietal junction [6]. The occurrence of hemineglect is prevalent in stroke patients, accounting for around 30% of cases, and has a significant impact on the recovery from stroke from the condition, diverse senses (such as vision, hearing, touch, and proprioception) and diverse mechanisms may be affected by neglect [7].
According to studies, 30% of stroke patients with left brain damage and 50% of those with right brain damage exhibit unilateral spatial neglect [8]. Common signs of unilateral neglect include eye and head deviation to the ipsilesional side, neglecting or failing to pay attention to individuals and items on the contralesional side, and stumbling into objects positioned on the contralesional side [4]. From the patient’s perspective, behavioural difficulties with everyday tasks like forgetting to eat or tending to the contralesional space are indicative of spatial neglect [7]. In poststroke patients, hemineglect condition can occur in up to 82% of cases [6].
There are routine or conventional therapies available for treating hemineglect in stroke such as transcutaneous electrical nerve stimulation, prism adaptation, limb activation, mirror therapy which showed a significant improvement in hemineglects. Pandian JD et al., from his study concluded that in patients with stroke, mirror therapy is a simple treatment that improves unilateral neglect [9]. The result from study by Kang TW and Kim BR suggested that the chopping pattern of PNF is effective in improving the hemi-spatial neglect, balance, and activities of daily living in stroke patients with neglect [10].
An essential component of stroke care is education, which should be provided to stroke victims, their families, and caregivers at all stages of care and during transitions. Individualised educational needs must occasionally be updated and re-evaluated as they evolve [11]. For continuity of care, education of the patient, family, and caregivers is crucial [12]. Strokes frequently cause people to abandon their previous lifestyle. The prospect of working, doing previously assigned home chores, or engaging in previously favoured leisure activities is precluded during the acute phase. Patients often abandon the habits that they developed before stroke, inclusive of hygienic habits. The patient ought to change as a result of the educational and pedagogical activities. It is possible that this will contribute to the patient’s ability to resume their prior activities [13]. The study done by Spaccavento S et al., concluded that Prismatic Adaptation (PA) and Visual-Scanning Training (VST) on patients with neglect following a right-hemisphere lesion both are useful rehabilitation techniques that appear to improve neglect [14].
Numerous tests have been developed specifically for the purpose of evaluating hemispatial neglect in stroke patients, the most widely utilised paper-and-pencil test is the line bisection test, which is the gold standard test for classifying the difficulty of hemineglect [15,16]. The Catherine Bergego scale analyses the functioning of unispatial neglect patients for 10 everyday situations after stroke, with the objective of assessing the impact of unispatial neglect on ADLs [16]. To measure functional independence in personal care and mobility, the Barthel Index was developed [17]. There is strong need for the patient, as well as, the caregiver to understand about hemineglect and awareness on how patient responds to neglected side. The purpose of this study is to prove the effectiveness of education along with conventional therapy on hemineglect helping improve the symptoms and functional outcomes so that the patient will get discharged early from the hospital. The null hypothesis of this study is that there will be no significant effect of education on hemineglect in patients with acute stroke. The alternative hypothesis of this study is that there will be significant effect of education on hemineglect in patients with acute stroke. Thus, the objective of the study is to determine the effects of education on hemineglect in patients with acute stroke.
The secondary objective of the study was to compare gender, type of strokes, co-morbidities, smoking and alcoholism among both groups and compare the type of strokes, co-morbidities, smoking and alcoholism among males and females
Materials and Methods
This is a parallel active-controlled, single blinded (assessor) randomised controlled trial in which the control group received the conventional therapy treatment and the experimental group were educated along with the conventional therapy. The sampling technique used was simple random sampling method. The study was carried out from January 2023-2024 and the participants were recruited from Justice K S Hegde Charitable Hospital, Mangaluru, Karnataka, India. Informed consent was taken from the participants who agree to participate in this study. The study proposal was ethically approved by Nitte Institute of Physiotherapy’s Institutional Ethical Committee, Mangaluru, Karnataka, India on February 9th 2023, with reference number: NIPT/IEC/Min/09/2022-2023. It was registered in the Clinical Trial Registry – India (CTRI) with the registration number: CTRI/2023/05/052179.
Inclusion criteria: Hemineglect patients and poststroke patients of any age (>45 years) or gender (both male and female) who were willing to participate were included in the study. Also, acute unilateral stroke confirmed on computed tomography scan and with ischaemic and haemorrhagic type of stroke (MCA territory) were also included. Patients and caregivers capable of communicating in English or Malayalam or Kannada and understanding instructions and those who were able to follow and respond to verbal instruction were included in this study.
Exclusion criteria: Those patients who had recurrent stroke, uncontrolled diabetes mellitus and hypertension, who were unconscious and with other neurological conditions were excluded. Also, those patients having aphasia, cognitive impairment, previous stroke related disability, with pre-morbid or co-morbid impairment, with lack of primary caregivers and who were not willing to give consent were also excluded from the study.
Sample size: On the basis of the study conducted by KB Riyas Basheer [17], mean±SD of Barthel Index in intervention group=40±10.66 and control group is 27.08±15.58, the estimated effect size=0.98, α=5%, power=80%, the estimated sample size for each group was 14. Further assuming 10% dropout, the final sample size required for each group was 14+2=16. Sample size was estimated using the software- G*Power 3.1.9.4.
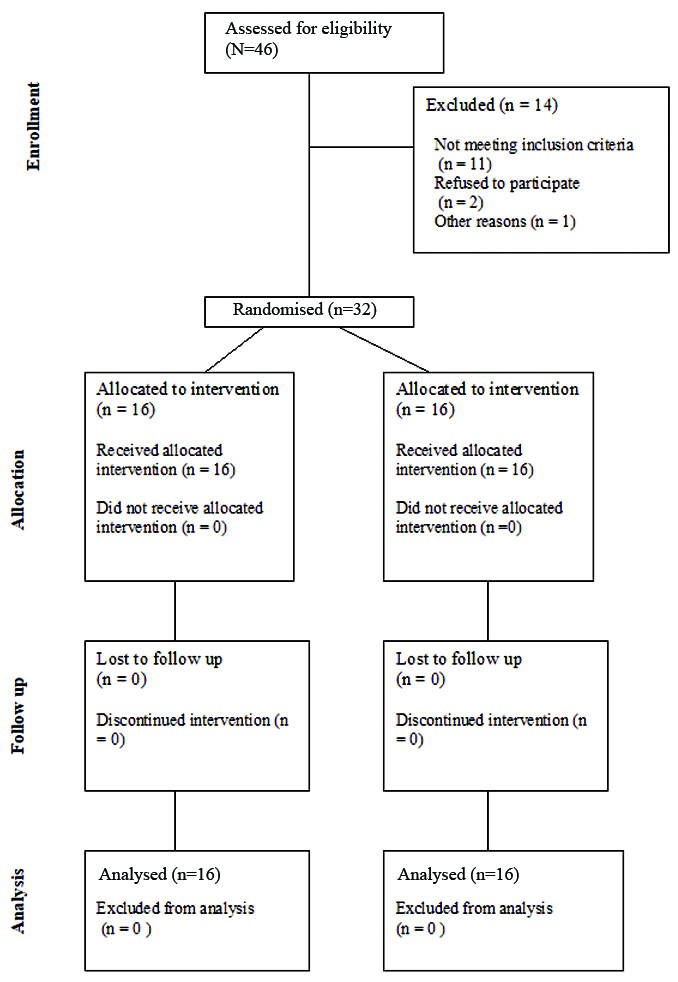
Randomisation and allocation: Randomisation was performed by generating random numbers from 1 to 32 using the www.random.org website [18]. These 32 random numbers were divided into two groups, with 16 numbers in each group. The random number generation was conducted by an independent researcher who was not part of the study. Allocation was done by Sequentially Numbered Opaque Sealed Envelope (SNOSE) and the subjects were equally allocated into two groups with an allocation ratio of 1:1 [Table/Fig-1].
Flowchart of participants (CONSORT flow chart).
Blinding: The primary investigator was blinded in this study to assess pre and post intervention using outcome measures.
Procedure
The participants were screened based on the inclusion and exclusion criteria, and the consent form was obtained. The subjects were then randomly allocated to either group. The selected participants were randomly divided into two groups experimental Group-A (16 participants) and control Group-B (16 participants). Both the groups received standard care treatment which included conventional therapy (positioning, active and passive range of motion exercises, bed mobility exercises) for 40 minutes one session per day for five days. Experimental group received education on Cueing which includes scanning training attempts to encourage patient to direct their gaze to the neglected side and to scan their environment to the left with verbal cueing. Addressing the activities of daily living and may involve direct verbal cues (“look left”/“check your left-side”), visual cues (visual targets, highlighted letters, visual signals, colourful stickers or markers), or tactile cueing (gentle tapping, applying pressure, objects with different textures); and environmental modification The patient’s bedside environment may be oriented leftwards and hence, make the patient perceive his or her left-side. Arrange the environment to minimise distractions (clear pathways, consistent lighting, contrasting colours, using mirror, bedroom modifications, bathroom adaptations, kitchen adjustments); Shifting of representation of space by eye patching, trunk rotation and neck rotations to increase leftward orientation, for adapting their space for improved spatial awareness and regarding sensory and perceptual awareness to incorporate visual scanning activities, visual compensations. Verbal instructions were used to encourage the patient to turn the head to the left to anchor his or her attention to that side of space. The patient is taught to become aware of the existence, the nature of the deficit and given education to increase cognitive awareness; using visual medium with the help of a pamphlet for 15 minutes once a day along with the standard care. The Pre-post intervention evaluation was done for both groups using Line bisection test which is a quick measure to detect the presence of unilateral neglect following stroke. The LBT test paper consist of 20 lines in a random arrangement, with eight lines in the centre, six on the left, and six on the right. The lines are 100, 120, 140, 160, 180, and 200 mm in length. The A4-size test paper was placed on the patient’s centre line with the patient in a sitting position. At first, the centre point of the two top and bottom lines will be showed and patient is instructed to mark the centre points of the remaining 18 lines. The top and bottom demonstration lines were excluded when measuring scores. A displacement of the bisection mark towards the side of the brain lesion is interpreted as a symptom of hemineglect. A deviation of more than 6 mm from midpoint indicates unilateral neglect [15,19,20].
Catherine Bergego scale which is used to track alterations in patient behaviour following specific interventions and to assess the presence and the extent of neglect on a sample of real everyday life activities. This instrument is a 10 items scale, for each subscale, a 4-point scale was used. Each question is scored from zero to three, where 0 corresponds to the absence of Ultrasonic Nebuliser (USN) for the given task (no neglect); 1 corresponds to discrete unilateral space negligence, characterised by slight asymmetry in space exploration (mild neglect where the patient will cross midline after the right side is attended to first.); and 2 represents moderate neglect where the patient has clear and consistent left-side omissions, 3 corresponds to severe neglect. The item scores are summed up to obtain a total. A score of 0 means no neglect, and 30 mean severe neglects. A 1 to 10 means mild behavioural neglect, 10-20 moderate behavioural neglect and 21 to 30 means severe behavioural neglect [21-23]; and the Barthel Index evaluates ten fundamental ADLs. Higher scores reflect higher levels of independence in ADLs, the overall score is 100. A score of 0-20 indicate “total” dependency, 21-60 “severe” dependency, 61-90 “moderate” dependency, 91-99 “slight” dependency [17,20,24]; evaluated on the first and fifth day of treatment sessions.
Statistical Analysis
The collected data were summarised by using the descriptive statistics: frequency, percentage; mean and standard deviation. The independent sample t-test was used to compare age, duration of stroke, Line Bisection, Catherine Bergego Scale, and Barthel Index according to gender, groups as well as type of stroke. The paired t-test was used for the pre to post-test comparison of Line Bisection, Catherine Bergego Scale, and Barthel Index irrespective of groups as well as within the groups. The Chi-square or Likelihood ratio test was used to compare difference in proportion. To find the relation between age, duration of stroke and the pre-test measurements of Line Bisection, Catherine Bergego Scale, and Barthel Index; the Pearson correlation coefficient (“r”) was used. The p-value <0.05 was considered as significant. Data were analysed by using the Statistical Package for the Social Sciences (SPSS) software (SPSS Inc.; Chicago, IL) version 29.0.10.
Results
The study consisted total of 32 participants of an average age of 60.97±11.01 years and duration of 8.34±3.81 days.
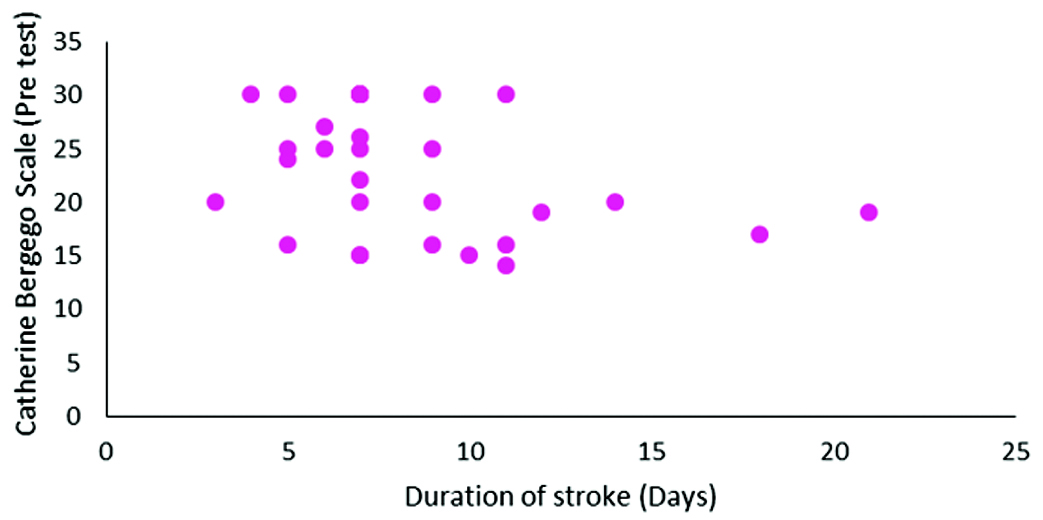
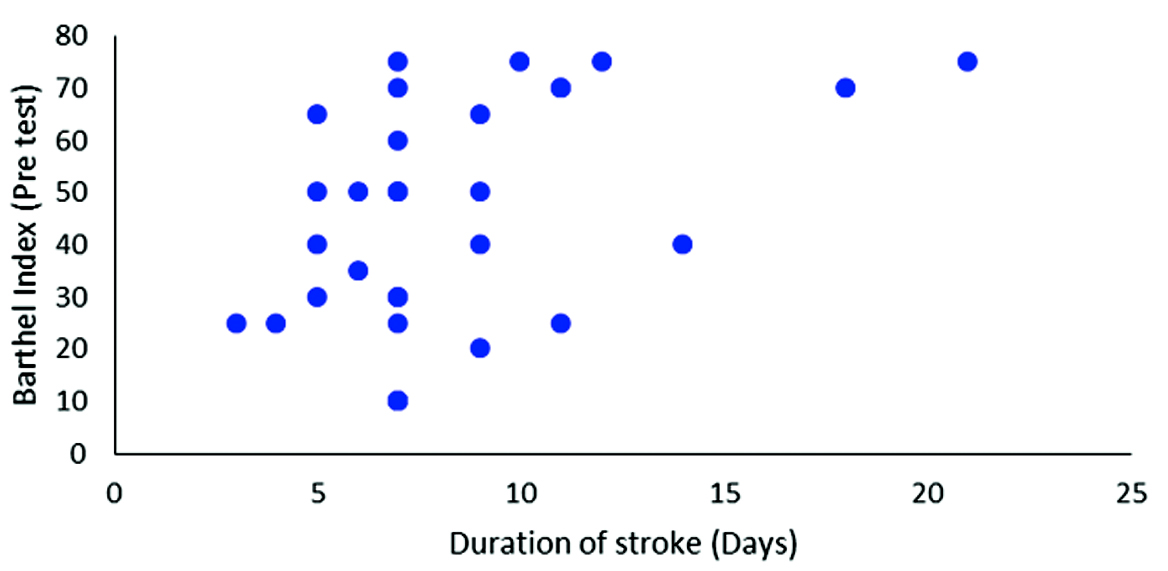
[Table/Fig-2,3 and 4] show Catherine Bergego scale and duration of stroke showed a negative correlation with an r=-0.367 (p=0.039). Whereas, a positive correlation, was observed between Barthel index and duration and stroke with an r-value of 0.446 (p=0.011).
Relation between age, duration of stroke and the pre-test measurements of Line Bisection, Catherine Bergego Scale, and Barthel Index.
| (Pre-test) | Age (years) | Duration of stroke (Days) |
|---|
| Line Bisection (cm) | “r” | 0.030 | -0.215 |
| p-value | 0.870 | 0.237 |
| Catherine Bergego Scale | “r” | 0.158 | -0.367 |
| p-value | 0.389 | 0.039* |
| Barthel Index | “r” | -0.310 | 0.446 |
| p-value | 0.085 | 0.011* |
Correlation between duration of stroke and Catherine Bergego scale.
Correlation between duration of stroke and Barthel index.
The [Table/Fig-5] shows comparison of gender, type of strokes, co-morbidities, smoking and alcoholism in both the groups using Chi-square or Likelihood ratio test. There was a significant difference (p<0.05) in type II diabetes experimental and control groups.
Comparison of gender, type of strokes, co-morbidities, smoking and alcoholism among both groups.
| Parameters | Groups | Chi-square/Likelihood ratio# | p-value |
|---|
| Experimental | Control |
|---|
| N | % | N | % |
|---|
| Gender | Male | 10 | 62.5 | 10 | 62.5 | 0 | 1 |
| Female | 6 | 37.5 | 6 | 37.5 |
| Type of stroke | Haemorrhagic | 5 | 31.3 | 6 | 37.5 | 0.14 | 0.710 |
| Ischaemic | 11 | 68.8 | 10 | 62.5 |
| Type II DM | Yes | 4 | 25.0 | 11 | 68.8 | 6.15 | 0.013* |
| No | 12 | 75.0 | 5 | 31.3 |
| Cardiac conditions | Yes | 1 | 6.3 | 2 | 12.5 | 0.37# | 0.541 |
| No | 15 | 93.8 | 14 | 87.5 |
| Smoking | Yes | 5 | 31.3 | 6 | 37.5 | 0.14 | 0.710 |
| No | 11 | 68.8 | 10 | 62.5 |
| Alcoholism | Yes | 5 | 31.3 | 6 | 37.5 | 0.14 | 0.710 |
| No | 11 | 68.8 | 10 | 62.5 |
There was a significant difference (p<0.05) in smoking and alcoholism according to gender, which is shown in [Table/Fig-6]. In [Table/Fig-7], the independent sample t-test was used to compare Line Bisection, Catherine Bergego Scale, and Barthel Index between both the groups. There was a significant difference (p<0.05) in Line Bisection, and Catherine Bergego Scale between experimental and control groups; during pre-test, as well as, post-test. The Barthel Index exhibited a significant difference (p<0.05) between the groups.
Comparison of type of strokes, co-morbidities, smoking and alcoholism among males and females.
| Parameters | Gender | Chi-square/Likelihood ratio# | p-value |
|---|
| Male | Female |
|---|
| N | % | N | % |
|---|
| Type of stroke | Haemorrhagic | 7 | 35 | 4 | 33.3 | 0.01# | 0.923 |
| Ischaemic | 13 | 65 | 8 | 66.7 |
| Type II DM | Yes | 9 | 45 | 6 | 50.0 | 0.075 | 0.784 |
| No | 11 | 55 | 6 | 50.0 |
| Cardiac conditions | Yes | 2 | 10 | 1 | 8.3 | 0.03# | 0.875 |
| No | 18 | 90 | 11 | 91.7 |
| Smoking | Yes | 11 | 55 | 0 | 0 | 13.66# | <0.001* |
| No | 9 | 45 | 12 | 100 |
| Alcoholism | Yes | 11 | 55 | 0 | 0 | 13.66# | <0.001* |
| No | 9 | 45 | 12 | 100 |
Comparison of Line Bisection, Catherine Bergego Scale, and Barthel Index between groups.
| Groups | Pre-test | Post-test |
|---|
| Mean | SD | “t” | p-value | Mean | SD | “t” | p-value |
|---|
| Line Bisection (cm) | Experimental | 2.65 | 0.63 | -2.50 | 0.018* | 1.46 | 0.46 | -7.54 | <0.001* |
| Control | 3.20 | 0.60 | 3.14 | 0.76 |
| Catherine Bergego Scale | Experimental | 20.31 | 4.56 | -3.12 | 0.004* | 12.19 | 5.33 | -5.60 | <0.001* |
| Control | 26.00 | 5.69 | 23.50 | 6.08 |
| Barthel index | Experimental | 51.88 | 21.05 | 1.96 | 0.059 | 74.06 | 15.83 | 4.55 | <0.001* |
| Control | 37.19 | 21.37 | 44.06 | 21.07 |
The [Table/Fig-8] shows the comparision of the effectiveness (pre-post) Line Bisection, Catherine Bergego Scale, and Barthel Index between groups. There was a significant difference (p<0.05) in the effectiveness in Line Bisection, Catherine Bergego Scale, as well as, Barthel Index between both the groups.
Comparison of effectiveness (pre-post) Line Bisection, Catherine Bergego Scale, and Barthel Index between groups.
| Effectiveness (pre-post) | Mean diff. | SD | “t” | p-value |
|---|
| Line bisection | Experimental | 1.19 | 0.57 | 6.41 | <0.001* |
| Control | 0.06 | 0.42 |
| Catherine Bergego Scale | Experimental | 8.13 | 2.16 | 6.20 | <0.001* |
| Control | 2.50 | 2.92 |
| Barthel index | Experimental | -22.19 | 12.38 | -4.41 | <0.001* |
| Control | -6.88 | 6.29 |
Discussion
The objective of the study was to determine the effect of education on hemineglect following acute stroke. In this study the mean age of participants was around 60.97 years, with a SD of approximately 11.01 years (60.97±11.01) and the average duration of stroke was about 8.34 days with a SD of around 3.81 days (8.34±3.81). The study results showed that there is significance difference (p<0.013) in type II diabetes mellitus according to the experimental and the control group. A study done by O’Donnell MJ et al., which demonstrated the impact of diabetes on stroke incidence and outcomes [25]. Mosenzon O et al., diabetes has been shown in epidemiologic studies to be a well-established risk factor for stroke. It is linked to several pathophysiological mechanisms that cause ischemic stroke, such as cardiac embolism, cerebral SVD, and large artery atherosclerosis. In addition to being associated with an increased risk of stroke, diabetes also generally has a negative impact on poststroke outcomes [26]. Kivioja R et al., study establishes the associations between 11 vascular risk factors and early-onset IS, among which atrial fibrillation, cardiovascular disease, and both type 1 and 2 diabetes mellitus in particular showed strong associations [27].
Also, found that there was significant difference (p<0.001) in smoking and alcoholism according to gender, resonates with a study done by Abdu H et al., which emphasised the role of lifestyle factors like age, cigarette smoking, and chewing khat were statistically significant risk factors for stroke in male patients compared to female patients, as indicated by multivariable logistic regression with 95% confidence interval. Approximately three times as many men as women will experience a stroke early in life. For smoking cigarettes and chewing khat, the risk factors for stroke were higher in men than in women by 2.911 and 3.650 times, respectively. Nonetheless, structural heart disease was less likely to be a risk factor for stroke in males than in women, with a p-value of <0.05 [28]. Lee Tk et al., in his study mentioned that diabetes and hypertension continue to be important risk factors for cerebral infarction and all types of stroke. Additionally, smoking was linked to a higher occurrence of all strokes (POR, 1.71), and there was only a marginally significant correlation between smoking and cerebral infarction (POR, 1.72). Once the impacts of other confounders were taken into account, the effects of alcohol use were no longer significant [29].
The pre-test to post-test comparison showed a significant difference (p<0.001) in Line Bisection Test, Catherine Bergego scale, and Barthel Index irrespective of groups and within both experimental and control groups. There was a difference (p<0.05) in Line Bisection, and Catherine Bergego Scale between experimental and control group; during pre-test as well as post-test. The Barthel Index exhibited a difference (p<0.05) between the groups: experimental and control during post-test. Also, there was a difference (p<0.05) in the effectiveness in Line Bisection, Catherine Bergego Scale as well as Barthel Index between the groups: experimental and control. Between the group differences in Line Bisection Test, Catherine Bergego Scale and Barthel Index for the experimental group were 1.19±0.57, 8.13±2.16, -22.19±12.38 respectively and for the control group were 0.06±0.42, 2.50±2.92, -6.88±6.29. Between the group comparison of Line Bisection Test, Catherine Bergego Scale and Barthel Index were found to be statistically significant (p<0.001), which proved that education has a major role in the recovery of hemineglect poststroke. Hafsteinsdóttir TB et al., highlighted in his article about the unmet educational needs of stroke patients and caregivers. Patients and carers after strokes reported a wide range of educational demands, many of which were unmet. Knowledge about the clinical aspects of stroke, prevention, treatment, and functional recovery were among the educational needs of stroke patients and carers. The most often mentioned needs of carers were related to patients’ lifting and moving, physical activity, dietary concerns, and psychological shifts. Patient and caregivers wanted information specific to their current situation [30]. Hong SE et al., concluded that there was effectiveness in caregivers education program on their satisfaction as well as patient functional recovery, performed in addition to daily conventional rehabilitation treatment [31]. Ahmad SA et al., concluded from his study that the caregiver education programme positively influenced patients functional independence and thus improves the quality of life [32]. Another study by Jung BC et al., indicates that combining conventional physical therapy with a rehabilitation education program is more effective in reducing depression and burden compared to physical therapy alone [33].
The Line Bisection was positively correlated (p<0.05) with Catherine Bergego Scale and negatively correlated (p<0.05) with Barthel Index. In a study conducted by Riyas Basheer KB et al., there seem to be a positive correlation between Catherine Bergego scale and Barthel Index for measuring functional independence in activity of daily living in acute stroke patient [17]. The result from study by Luukkainen-Markkula R et al., proved that the Line Bisection subtest from BIT had significant correlation with the CBS, and both the test showed good internal consistency. Also, there was a negative correlation (p<0.05) between Catherine Bergego Scale, and Barthel Index during pre-test. Among experimental group, the Line Bisection was positively correlated (p<0.05) with Catherine Bergego Scale. Also, there was a negative correlation (p<0.05) between Catherine Bergego Scale, and Barthel Index during pre-test [34]. A study by Marques CL et al., resulted in CBS negatively correlated with BIT and low correlation with Barthel Index. The duration of stroke was negatively correlated (p<0.05) with Catherine Bergego Scale and positively correlated (p<0.05) with Barthel Index. The duration of stroke was positively correlated (p<0.05) with Barthel Index among experimental group [16].
Through educating patient and caregiver and providing standard care, physiotherapy will be effective once the perceptual problems are addressed. Reduction in the presence of hemineglect in the intervention group suggests improvement in severity of neglect and functional independence in the activity of daily living. As per results obtained, hypothetically, we reject the null hypothesis and accept the experimental hypothesis which suggests that education may have significant effect on hemineglect over the standard care following acute stroke.
Limitation(s)
In the present study, no long term follow-up was conducted and that was a limitation to the study. Further studies with a longer follow-up period can be done in future.
Conclusion(s)
The current single blinded randomised controlled trial results suggests that education coupled with standard care is beneficial in reduction of presence and severity of hemineglect following acute stroke. Reduction in unilateral neglect leads to improvement in the activity of daily living following acute stroke by educating over the conventional neglect management. Thus, will be helpful in improving the perceptual awareness so that the patient will get discharged early from the hospital. Physiotherapy will be effective once the perceptual problems are addressed.