Cataracts are a major cause of treatable visual impairment in developing countries [1]. Vision impairment and blindness are both causes and consequences of poverty [2]. Blindness often contributes to decreased economic productivity, which further exacerbates the cycle of poverty in affected communities [3]. This association underscores the far-reaching impact of visual impairments, not only on individual health but also on broader socio-economic dynamics. The study by Finger RP et al., showed that patients who underwent cataract extraction experienced significant improvement in their economic status and concluded that, in addition to restoring sight, there is an additional benefit of mitigating poverty in the long run [4].
The primary objective of cataract surgery is to enhance an individual’s visual function. The rationale behind this intervention lies in the assumption that an improvement in vision will consequently lead to an amelioration in the quality of life associated with vision-related aspects. It is widely acknowledged that cataracts stand out as the predominant cause of visual impairment, particularly affecting a considerable proportion of individuals residing in developing countries [5]. Blindness and visual impairment have been shown to reduce VRQoL, general health and social status, while increasing mortality [1].
Moreover, it is noteworthy that strabismus, a condition characterised by misalignment of the eyes, although not as prevalent as cataracts, affects approximately 4% of the adult population. This necessitates attention and suitable interventions within the broader scope of visual health initiatives [6]. Diplopia (double vision) and amblyopia (commonly known as lazy eye) are the prevailing presentations within the spectrum of strabismus, a frequently encountered ocular misalignment [7]. A study by Chang MY et al., showed that 81% of strabismus patients experienced diplopia, and these patients reported significantly worse eye pain during any surgery [6]. Notably, diplopia can emerge postcataract surgery due to extended sensory deprivation, which disrupts the harmonious fusion of visual inputs, weakness in one or more eye muscles, adverse effects of local anaesthesia on muscles, visual distortions and pre-existing medical conditions [8].
Furthermore, investigations have suggested a correlation between poor visual outcomes and the presence of concurrent ocular co-morbidities, demonstrating an odds ratio of 2.7 [9]. However, it is noteworthy that the specific odds ratio solely attributable to strabismus, devoid of additional ocular complications, remains undefined within the existing literature. While certain studies have extensively detailed the beneficial outcomes of surgical interventions in cases where cataracts coincide with conditions such as age-related macular degeneration, it is crucial to exercise caution when extrapolating these findings to other co-morbidities, such as strabismus [10-14]. The unique complexities and interactions involved in strabismus necessitate a more nuanced understanding and a tailored approach, distinct from those applied to different ocular conditions.
Materials and Methods
The present quasi-experimental study was conducted in the Department of Ophthalmology, RL Jalappa Hospital and Research Centre, Kolar, Karnataka, India, from August 2023 to September 2023. It received approval from the Institutional Ethics Committee (IEC) (SDUMC/KLR/IEC/352/2023-24), and written informed consent was obtained from all participants.
Sample size calculation: The sample size was estimated based on the proportion of the adult population (4%) with strabismus [6].
Z1-α/2 is the standard normal variate. At a 5% type I error rate (p-value <0.05), it is equal to 1.96, while at a 1% type I error rate (p-value <0.01), it is equal to 2.58. In the majority of studies, p-values are considered significant, if they are below 0.05; therefore, 1.96 is commonly used in the formula.
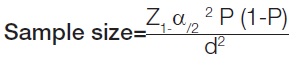
where,
d=P=4% or 0.04 (the expected proportion in the population based on a previous study)
q=96% or 0.96
d=5% or 0.05 (the absolute error or precision)
Using the values provided at a 95% confidence level, a sample size of 59 subjects was included in the study.
Inclusion criteria: Patients aged 42-79 years who were attending the Outpatient Department (OPD) and had both cataracts and varying degrees of strabismus, with visual acuity in the worse eye being worse than or equal to 6/60 on the Snellen vision chart were included in the study.
Exclusion criteria: Patients with visual acuity better than 6/60 in the worse eye, those with opacities in the ocular media (cornea and vitreous), or those with significant retinal pathologies were excluded from the study.
After applying these criteria, 15 patients were excluded: 11 had vision better than 6/60, two had diabetic retinopathy changes, one had a corneal opacity, and one was not operated on due to systemic co-morbidities. Consequently, 44 patients were included in the study.
Study Procedure
During the comprehensive assessment, demographic information was collected alongside a detailed patient history. Initial visual acuity for both distant and near vision was evaluated using the Snellen chart. Ocular alignment was examined using the Hirschberg test and the cover-uncover test, followed by slit lamp biomicroscopy.
The Hirschberg test is performed to estimate the angle of manifest strabismus, which can be determined by observing the position of the corneal light reflex when a torchlight is shined on the cornea. Each millimeter of deviation corresponds to approximately 7° of deviation or 14 Prism Diopters (PD), assuming a pupil diameter of 4 mm [17].
The alternate cover test is a dissociation test performed to identify the total deviation by interrupting fusion. A plastic prism is placed in front of one eye while alternately covering and uncovering the eyes to observe the re-fixation movement on an accommodative target. The prism’s power is gradually increased until the direction of the refixation movement reverses, and then the prism power is reduced until no further re-fixation movement is observed in the other eye, indicating neutralisation. The prism power that either fully neutralised the deviation or was closest to achieving neutralisation was recorded [18].
Additionally, a thorough fundus examination was conducted using a +90D lens-assisted slit lamp biomicroscopy and indirect ophthalmoscopy. The preoperative quality of life was assessed using the IND-VFQ-33 [19]. The patients were further categorised into three groups: group 1 with 15° deviation, group 2 with 30° deviation and group 3 with 45° deviation. All 44 patients underwent unilateral manual small incision cataract surgery with posterior chamber Intraocular Lens (IOL) implantation in the worse eye. After surgery, visual acuity and IND-VFQ-33 were reassessed at six weeks to monitor changes in the patients’ VRQoL.
Postoperatively, visual acuity was further graded into: no to mild vision impairment {Best-corrected Visual Acuity (BCVA) <6/18), moderate vision impairment (BCVA 6/24 to 6/60), severe vision impairment (BCVA 6/60 to 3/60) and blindness (BCVA worse than 3/60) [19].
The IND-VFQ-33 scoring was conducted by the trainee surgeon. Each question had four active response options targeting difficulty or frequency using Likert scaling, ranging from “no problems at all” to “a lot.” The three subscales, as proposed by the developers, were separately assessed. The overall general functioning scale was split into mobility and activity limitation scales. The scores were averaged to generate three subscale scores: general functioning, psychosocial impact, and visual symptoms [20].
Statistical Analysis
Data were analysed using Statistical Package of Social Sciences (SPSS) version 22.0 software. The paired t-test was used to assess the significance of pre and postoperative quantitative data. A p-value of <0.05 was considered statistically significant, assuming that all the rules of statistical tests were followed.
Results
Various characteristics of the patients are shown in [Table/Fig-1]. This study comprised 44 strabismus patients with cataracts, with a mean age of 64.34±8.09 years (range: 42-79 years). Among the cohort, 29 (65.9%) patients were aged between 50 years and 70 years. The cohort included 15 (34%) males and 29 (66%) females. All patients underwent unilateral manual small incision cataract surgery on the worse eye. The degree of strabismus among the patients varied: 61.36% exhibited a 15° deviation, 27.27% a 30° deviation, and 11.36% a 45° deviation. A total of 93.1% of patients presented with exotropia, while 6.9% exhibited esotropia.
Distribution of subjects according to age group, gender and, the amount and type of deviation.
| Characteristics | Frequency (n) | Percentage (%) |
|---|
| Age (years) | 41-50 | 4 | 9.1 |
| 51-60 | 7 | 15.9 |
| 61-70 | 22 | 50.0 |
| 70-80 | 11 | 25.0 |
| Gender | Male | 15 | 34 |
| Female | 29 | 66 |
| Strabismus | 15° | 27 | 61.4 |
| 30° | 12 | 27.3 |
| 45° | 5 | 11.3 |
| Type of deviation | Exotropia | 41 | 93.1 |
| Esotropia | 03 | 6.9 |
The preoperative and postoperative IND-VFQ-33 scores and CDVA for the entire study population are presented in [Table/Fig-2]. The results indicate significant improvements in CDVA from the preoperative to the postoperative period. The IND-VFQ-33 questionnaire reveals significant reductions in scores for general functioning, mobility, activity limitation, psychosocial impact and visual symptoms. Postoperatively, no patient complained of diplopia. Overall, 84.09% of patients experienced mild to no visual impairment postoperatively.
Comparison of preoperative and postoperative Indian Vision Related Quality of Life 33 questionnaire (IND-VFQ-33) and visual acuity (CDVA logMAR).
| IND-VFQ-33 | Preoperative(Mean±SD) | Postoperative(Mean±SD) | p-value |
|---|
| General functioning |
| Mobility | 12.29±3.19 | 9.04±3.21 | <0.001* |
| Activity limitation | 19.63±4.89 | 16.81±5.56 |
| Overall | 31.92±8.08 | 25.85±8.77 |
| Psychosocial impact | 11.57±1.75 | 7.09±2.17 | <0.001* |
| Visual symptoms | 22.34±1.53 | 9.30±3.26 | <0.001* |
| CDVA logMAR | 1.66±0.40 | 0.48±0.44 | <0.001* |
Paired t-test; *The p-value <0.05 was considered statistically significant values
The preoperative and postoperative IND-VFQ-33 scores for patients with 15°, 30° and 45° strabismus are presented in [Table/Fig-3], revealing significant improvements across various aspects of VRQoL. For all degrees of strabismus, there were significant postoperative enhancements in mobility and visual symptoms, as well as, in overall quality of life scores. Activity limitation and psychosocial impact also showed significant improvements in patients with 15° and 30° strabismus, although these improvements were not statistically significant for patients with 45° strabismus. Additionally, significant postoperative improvements in CDVA logMAR were observed across all degrees of strabismus. Overall, the results indicated ample gains in multiple aspects of VRQoL, with more pronounced improvements in activity limitation and psychosocial impact for patients with 15° and 30° strabismus.
Comparison of preoperative and postoperative IND-VFQ-33 questionnaire and Visual acuity (CDVA logMAR) according to degree of strabismus.
| Deviation | 15° | 30° | 45° |
|---|
| IND-VFQ-33 | Preoperative(Mean±SD) | Postoperative(Mean±SD) | p-value | Preoperative(Mean±SD) | Postoperative(Mean±SD) | p-value | Preoperative(Mean±SD) | Postoperative(Mean±SD) | p-value |
|---|
| General functioning |
| Mobility | 21.28±1.78 | 11.42±2.02 | 0.001* | 21.36±1.96 | 12.63±3.58 | 0.001* | 21.6±2.07 | 16.4±4.82 | 0.07 |
| Activity limitation | 35.14±0.17 | 18±3.63 | 0.001* | 37.72±3.49 | 21.36±5.85 | 0.001* | 34±5.33 | 25±4.52 | 0.05 |
| Overall | 56.42±1.95 | 29.42±5.65 | 0.001* | 59.08±5.45 | 33.99±9.43 | 0.001* | 55.6±7.4 | 41.4±9.34 | 0.05 |
| Psychosocial impact | 11.55±1.76 | 6.8±1.39 | 0.001* | 11.66±1.96 | 7.75±3.53 | 0.001* | 11.4±1.51 | 9±4.24 | 0.13 |
| Visual symptoms | 22.22±1.62 | 8.9±1.86 | 0.001* | 22.33±1.49 | 10.12±3.79 | 0.001* | 23±1.22 | 13.5±3.53 | 0.01* |
| CDVA logMAR | 1.36±0.60 | 0.47±0.40 | 0.001* | 1.63±0.36 | 0.77±0.43 | 0.001* | 1.43±0.56 | 1.08±0.75 | 0.05 |
Paired t-test; *The p-value <0.05 was considered statistically significant values
In the present study, among the 27 patients in the 15° strabismus group, all 27 patients achieved a postoperative BCVA of ≤6/12, indicating no visual impairment. There was a significant improvement in daily activities such as climbing stairs, walking on the road, finding new places, attending social functions, going out at night, recognising faces at various distances, locking and unlocking doors, and maneuvering in new environments following cataract surgery. This improvement resulted in greater confidence for patients in performing their daily activities.
Conversely, among the 12 patients with a 30° squint, 7 (58.3%) patients had a postoperative BCVA of ≤6/18, indicating no to mild visual impairment. Three (25%) patients had visual acuity between 6/24 and 6/60, indicating moderate visual impairment. Two (16.66%) patients had postoperative visual acuity worse than 6/60, indicating severe visual impairment. Two (16%) patients experienced difficulty discerning holes and bumps in the road while walking, recognising people from a distance and distinguishing between different banknotes. Five (41%) patients had considerable difficulty going out at night, attending social functions and performing their daily chores. Overall, 75% of these patients were able to perform their daily activities with little to no difficulty following cataract surgery.
Among the five patients with a 45° squint, 3 (60%) patients had a postoperative BCVA of ≤6/18, indicating mild to moderate visual impairment, with 1 (20%) patient achieving a postoperative BCVA of 6/60, indicating moderate visual impairment, and 1 (20%) patient having a BCVA of 2/60, indicating poor visual impairment. (40%) patients experienced significant difficulty with daily activities such as climbing stairs, walking on the road, finding new places, attending social functions, going out at night, recognising faces at various distances, locking and unlocking doors and manoeuvring in new environments following cataract surgery. One (20%) patient had considerable difficulty discerning bumps in the road and expressed feeling quite frightened to travel alone at night due to poor vision. Overall, only two (40%) patients were able to perform their daily activities with little to no difficulty following cataract surgery. However, another two (40%) patients reported significant improvements in their quality of life, despite still experiencing considerable difficulty in performing daily chores. Only one patient reported no change following cataract surgery.
Discussion
Cataracts and strabismus are complex ocular conditions that intricately intertwine, often compounding the challenges faced by individuals seeking optimal visual health and a high quality of life. Both conditions profoundly impact visual acuity and the perceptual experience. The interplay of these conditions necessitates surgical interventions to address visual impairments. An in-depth exploration of the repercussions of cataract surgery on the VRQoL in strabismus patients is essential to discern the nuanced, comprehensive benefits derived from such therapeutic interventions.
The current study comprised 44 patients attending the Ophthalmology OPD, with a mean age of 64.34±8.09 years (range: 42-79 years). Notably, 29 (65.9%) of the patient cohort falls within the age range of 50-70 years. The present study findings align with those of earlier researchers who reported similar age distributions. Research conducted by González-Cruces T et al., indicated a mean age of 68.9 years [21]. Another study by Akpolat C et al., found the mean age of patients to be 64.79 years [22]. In a study by Gallenga CE et al., the mean age of patients was found to be 55.5 years [23]. Additionally, Zhu M et al., reported a mean age of 69 years for patients with cataracts [24]. Cataract formation is associated with advancing age, leading to a predominance of older adults among individuals undergoing cataract surgery.
Within the study cohort, 65.9% were females and 34.1% were males. In a study conducted by Sreenivas V et al., 62.5% of patients from rural Angamally were females, which is comparable to the present study [9]. Du YF et al., and Vashist P et al., also found a higher prevalence of senile cataracts among women [25,26]. The elevated proportion of females in this cohort may be attributed to a higher participation of females at camp sites, while a considerable portion of males, constrained by work commitments, exhibit reluctance to seek OPD consultations.
Of the 44 patients, 93.1% had exotropia, while 6.9% had esotropia, which is consistent with findings from another study by Zhang XJ et al., where 90.69% of the cohort had exotropia [27]. Additionally, a study by Spierer A et al., showed that 97.9% of the patients had exodeviation, which aligns with the present study findings [28].
The IND-VFQ-33 questionnaire gathers patients’ personal experiences regarding how vision issues impact their daily activities. It is suitable for individuals with varying literacy levels and is brief enough to reduce respondent fatigue. The present study revealed significant improvements in various domains following cataract surgery. The improvements were statistically significant (p-value <0.001) for all three domains, indicating a positive impact of cataract surgery on patients’ quality of life. Akpolat C et al., also found significant improvements in quality of life following cataract surgery [22]. A study by Chang MY et al., showed significant improvements in all aspects of quality of life at four months after cataract surgery [6]. In a study by Zhu M et al., it was found that cataracts significantly decreased VRQoL in most of the measured parameters [24].
Additionally, the CDVA also showed substantial improvement postoperatively. In the current study, the CDVA logMAR improved from 1.66±0.4 preoperatively to 0.49±0.45 postoperatively. In the study conducted by Akpolat C et al., the preoperative mean logMAR BCVA values improved from 0.62±0.79 to 0.17±0.66 (p-value <0.001) in the postoperative period [22]. Similarly, in another study by Onofre-Déciga PK et al., BCVA improved from a preoperative logMAR of 1.58 to a postoperative logMAR of 0.68, indicating a significant improvement in vision following cataract surgery [29]. In the present study, 70.45% of the patients had postoperative visual acuity of 6/12 or better. Research conducted by Desai P et al., showed that 77% of the patients with co-morbidities had postoperative visual acuity better than 6/12 [30]. These findings underscore the efficacy of cataract surgery in enhancing both visual acuity and patients’ subjective well-being.
The outcomes of the present study highlights the variable impact of cataract surgery on patients with different degrees of strabismus. In patients with 15° strabismus, the surgery led to a notable enhancement in visual function and daily activities. These patients reported significant improvements in their ability to perform routine tasks such as climbing stairs, navigating new environments and recognising faces. The enhanced visual acuity and functional abilities postoperatively contributed to greater confidence and independence in their daily lives.
In contrast, patients with 30° strabismus experienced a more mixed outcome. While a substantial proportion managed to carry out daily activities with minimal difficulty, a significant minority faced challenges in specific tasks such as walking on uneven surfaces and recognising people from a distance. The variability in outcomes for this group suggests that while cataract surgery can improve visual function, the degree of strabismus may still influence the extent of functional recovery and ease in performing daily activities.
Patients with 45° strabismus presented the most complex postsurgical scenario. Despite improvements in some aspects of their visual functioning, a significant percentage continued to struggle with essential daily activities. The lower postoperative visual acuity in this group, along with difficulties in navigating environments and recognising objects, underscores the need for additional support and rehabilitation to maximise functional outcomes. Although some patients reported meaningful gains in their quality of life, the challenges faced by a portion of this group highlight the limitations of cataract surgery alone in addressing the broader impacts of severe strabismus.
These findings indicate that while cataract surgery can substantially improve visual outcomes and daily functioning, the degree of preoperative strabismus plays a crucial role in determining the extent of these benefits. Tailored interventions and supportive measures may be necessary to address the specific needs of patients with more severe strabismus to optimise their postoperative functional outcomes and quality of life.
Data from the present study indicates that following cataract surgery, improvements in general functioning, psychosocial impact and visual symptoms scores were more substantial in patients with less severe strabismus. Specifically, patients with 15° strabismus showed the greatest improvements across all measures, while those with 45° strabismus had the least improvement. This suggests that a smaller degree of initial eye deviation is associated with better postoperative outcomes, whereas larger deviations correspond to poorer improvements, likely reflecting the challenges of treating more severe strabismus and the potential for underlying conditions such as amblyopia.
None of the patients had any complaints of diplopia postoperatively. A study by Hatt SR et al., showed that the improvement in VFQ25 scores in patients undergoing strabismus surgery is minimal in those without diplopia; thus, these patients with concurrent cataracts might benefit more from cataract surgery than from strabismus surgery [31].
The intricate procedure of cataract surgery involves the meticulous removal of the opacified lens, followed by the placement of an artificial IOL. The present intervention was aimed not only to restore visual acuity but also to enhance perceptual clarity. For individuals struggling with strabismus, cataract surgery presents an opportunity to mitigate the impediments arising from double vision or visual blurring often associated with their condition. Empirical evidence has shown that the restoration of clear vision through cataract surgery significantly influences daily functioning, fostering heightened self-assurance and independence among strabismic patients.
The findings from the present study provide intriguing insights into the impact of cataract surgery on various aspects of patients’ lives. The significant decrease in mean scores for general functioning, psychosocial impact and visual symptoms postoperatively indicates a positive effect on the overall quality of life following surgery. Strabismic anomalies frequently disrupt the harmonious confluence of binocular vision, compromising both depth perception and ocular alignment. The benefits of cataract surgery extend to the improvement of these visual facets in individuals affected by strabismus. By rectifying cataracts, this surgical intervention contributes substantially to restoring binocular vision and enhancing ocular alignment. Such advancements offer tangible benefits in terms of improved depth perception, thereby alleviating the challenges faced by strabismus patients in tasks that require precise spatial judgment and the synchronised co-ordination of both visual axes.
Limitation(s)
The limitations of the present study include the short follow-up period of six weeks, which may not capture the long-term effects of cataract surgery on quality of life. Furthermore, the study lacks a control group, making it challenging to attribute the observed changes solely to cataract surgery without considering other potential factors. Future research with larger sample sizes, longer follow-up periods, and possibly randomised controlled trials could further validate and expand on these findings.
Conclusion(s)
The study revealed a significant number of patients with strabismus and cataracts belonging to the elderly age group of 61-70 years, with a female predominance. Exotropia was the most common type observed, and a majority of patients had a 15-degree strabismus. Cataract surgery was shown to greatly improve VRQoL in these patients, as evidenced by notable enhancements in clinical outcomes and patient-reported measures. These improvements were most pronounced for patients with 15° of deviation and least for those with 45° of deviation. The scores from the IND-VFQ-33 indicated significant improvements postoperatively across different domains. These enhancements suggest that cataract surgery had a positive effect on the participant’s overall quality of life related to vision, including their functional abilities, psychological well-being, and reduction in visual symptoms. A nuanced understanding and advocacy for timely cataract surgery in the strabismic cohort not only herald visual reclamation but also signify a profound improvement in their overall well-being and quality of life.
Paired t-test; *The p-value <0.05 was considered statistically significant values
Paired t-test; *The p-value <0.05 was considered statistically significant values