Introduction
Neck Pain (NP), a major global disability, disproportionately affects women, especially homemakers performing repetitive domestic tasks with poor ergonomics. Regular exercise helps, but access might be limited. Telerehabilitation, using technology for remote care, emerges as a potential solution. Homemakers with NP often lack access to exercise programmes. This study tests if telerehabilitation with exercises and ergonomics improves their function.
Aim
The aim of this study was to assess the effectiveness of a combined tele-rehabilitation programme incorporating structured neck exercises and ergonomic advice for the sustainable management of NP among homemakers experiencing non-specific NP.
Materials and Methods
This experimental study was carried out at BV (DU), School of Physiotherapy on 63 female homemakers residing at Sangli city, Maharashtra. The duration of study was one year from March 2023 to April 2024. Participants aged 25-55, with moderate NP (VAS 2-5) and performing tasks like chopping, mopping, and lifting for more than 4 hours a day, were included. A 30-day telerehabilitation programme with daily supervised exercises and ergonomic advice was carried out. Wilcoxon Matched Pairs test was used to compare pretest and post-test VAS, Neck Disability Index (NDI), performance, and Manual Muscle Testing (MMT) scores. The p-value: 0.001 (at 5% level of significance).
Results
The combined intervention significantly improved pain, strength, quality of life, and all components of the ICF Core Set, a standardised outcome measure for disability. 68.46% reduction was seen in VAS scores; 83.68% reduction was seen in NDI scores with effect size 0.9570. Maximum improvement of 100% was seen in code d4103 (sitting) and a minimum improvement of 40.86% was seen in code d4105 (bending).
Conclusion
Telerehabilitation with structured neck exercises and ergonomic advice can effectively reduce pain, improve strength and quality of life, and enhance function in homemakers with NP. This study also highlights the ICF Core Set’s usefulness in evaluating NP interventions. Telerehabilitation offers a promising, accessible treatment option for individuals facing barriers to in-person care.
Introduction
Globally, Musculoskeletal (MS) conditions impact more than 1.7 billion people, standing as the fourth most prominent health concern worldwide imposing considerable functional limitations on adults compared to other health issues. Homemakers, playing a pivotal role in nurturing society, engage in tasks that induce ergonomic stress and muscle exhaustion, consequently leading to Musculoskeletal Pain (MSP) [1]. Approximately, 150 million individuals grapple with work-related MS disorders, and in India, housewives exhibit a significant 49% prevalence of such disorders [2]. Non-specific NP, marked by discomfort in the posterior and lateral regions of the neck [3], affects a substantial global population, with prevalence ranging from 16.7% to 75.1% [4]. Notably, NP stands as the fourth leading cause of years lost to disability. These conditions, characterised by inflammatory and degenerative factors, originate from forceful, repetitive, and prolonged job tasks, impacting soft-tissues, tendons, tendon sheaths, muscles, and nerves across various body regions [5].
The World Health Organisation (WHO) defines MS disorders as multifactorial, with work playing a significant but not exclusive role in their development [6]. Common occurrences include musculoskeletal disorders that affect the neck and upper extremities, impacting soft-tissues such as tendons, muscles, joints, ligaments, and nerves. The latest estimate reveals that a substantial 269 million people worldwide will grapple with NP by 2050 [7].
In the context of household income and workforce participation women constitute 42% of workforce (International Labour Organization (ILO), Asian decent work decade 2006-2015) [8] and in India, where over 60% of women are homemakers due to traditional gender norms, household tasks contribute significantly to MSP [9]. Work-related fatigue and strain injuries are more prevalent in women than men [10]. The domestic kitchen, a hotspot for hazards, contributes to physical and mechanical risks due to poor ergonomics, low-quality equipment, and inadequate maintenance. Despite the associated pains, homemakers, constrained by prevailing gender norms and economic dependence, often lack awareness and resources for corrective measures. A systematic review underscores that education alone may not improve non-specific NP but shows positive outcomes when combined with exercise therapy [10].
Work activities in house such as heavy lifting, twisting, bending, and awkward postures, prolonged sitting, and standing with repetitive movements can contribute to develop low back pain and NP [11]. Conservative treatments and complementary approaches, including exercise, demonstrate efficacy in managing NP [12]. In a world facing healthcare access barriers and rising costs, telerehabilitation shines as a game-changer. It empowers geographically distant patients, tackles transportation hurdles, and promotes self-management through virtual therapy (e.g., VR). Studies show its effectiveness in diverse conditions, from stroke to chronic pain (NCBI, 2023). This technology’s potential to improve patient outcomes, accessibility, and affordability makes it a vital tool for the present and future [13].
The International Classification of Functioning, Disability and Health (ICF) model by WHO provides a comprehensive framework for understanding the interplay between health conditions, personal factors, and environmental factors [14].
There are numerous studies which have been carried out on NP among office workers but there is dearth in literature when it comes to homemakers, furthermore there is paucity of literature about ICF and its documentation with NP for homemakers, so this study was aimed to know the pre and post effect of structured exercises and ergonomics along with telerehabilitation on activity limitation and participation restriction in homemakers due to non-specific NP with the goal of providing valuable insights into an accessible and sustainable approach for NP management in this specific population.
In order to investigate the influence of interventions on NP, this study tested two competing hypotheses. The null hypothesis (H0) proposed that there will not be any difference after the intervention of structured exercise programmes, ergonomic and telerehabilitation improvements in alleviating non specific NP among homemakers.
Materials and Methods
This experimental study was carried out at BV (DU), School of Physiotherapy on 63 female homemakers residing at Sangli city, Maharashtra. The duration of study was one year from March 2023 to April 2024. Ethical clearance was obtained from the institution ethical committee with reference no. BV(DU)/SI No.2023-24/09 prior to the commencement of the study. The guidelines of Indian Council of Medical Research [15] were followed throughout the interview and treatment and all the safety precautions were taken. The study was conducted on 63 homemakers having non-specific NP who were consulted and were assessed in the hospital Physiotherapy OPD.
Inclusion criteria:
Married woman with age of 25-55 years complaining of NP with Visual Analogue Score (VAS) ranging 2-5 [2].
Working for >4 hours a day in the kitchen and performing at least three of the following tasks; chopping, mopping, stirring, washing utensils and lifting.
Not engaged in any other job other than housekeeping.
Exclusion criteria:
Expecting or breastfeeding women.
Those diagnosed with a psychiatric illness.
Those with a congenital illness affecting skeletal tissue.
Having one or more children with age less than two years.
Not having appropriate materials to attend online sessions.
Study Procedure
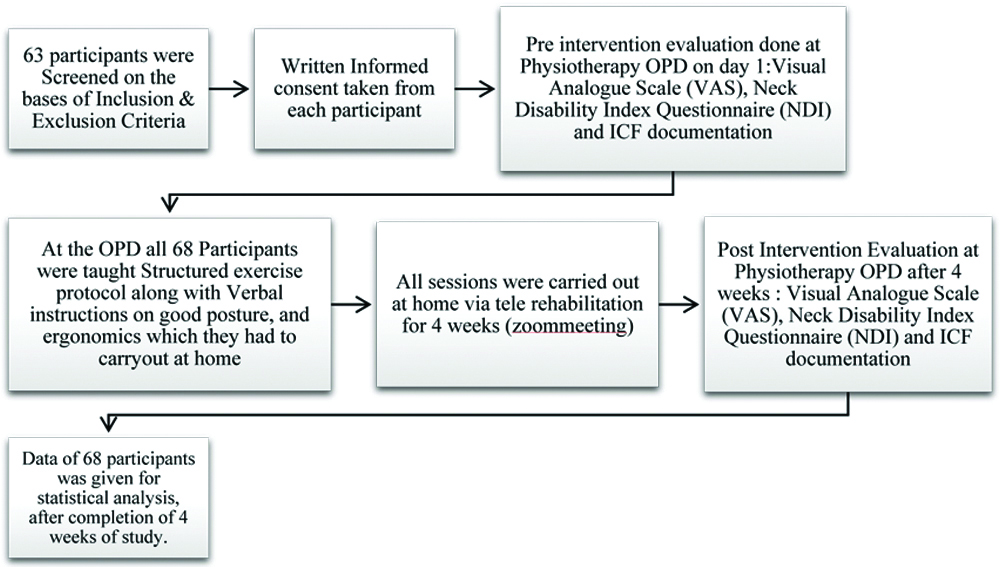
The ICF functional profile checklist was developed for evaluation of functional disability among home makers involving the non-specific NP using ICF codes as a guide [16]. The final core set chosen for evaluation of functional disability in home makers is as follows [Table/Fig-1]. The entire study procedure is explained in [Table/Fig-2].
| S. No. | Code | Description |
|---|
| 1 | b134 | Sleep functions |
| 2 | b28010 | Pain in head and neck |
| 3 | s7104 | Muscles of head and neck region |
| 4 | s7108 | Muscles of head and neck region, other specified |
| 5 | s76000 | Cervical vertebral column |
| 6 | d230 | Carrying out daily routine |
| 7 | d4103 | Sitting |
| 8 | d4104 | standing |
| 9 | d4105 | bending |
| 10 | d430 | Lifting and carrying objects |
| 11 | d450 | Walking |
Flow chart of methodology.
Structured exercise programme was set according to the FITT principle [17] [Table/Fig-3]. The FITT principle is a set of guidelines [18] used to create a safe and effective exercise programme. It stands for frequency, intensity, time, and type [Table/Fig-4].
Structured exercise protocol.
| 1 | Progressive neck isometrics |
| Press your palm against your forehead. Resist with your neck muscles. Hold for 10 seconds. Relax. Repeat 5 times. |  |
| 2 | Dynamic exercises |
| a | Dumbbell curls3 sets of 10 curls with 5 sec rest in between each set. | 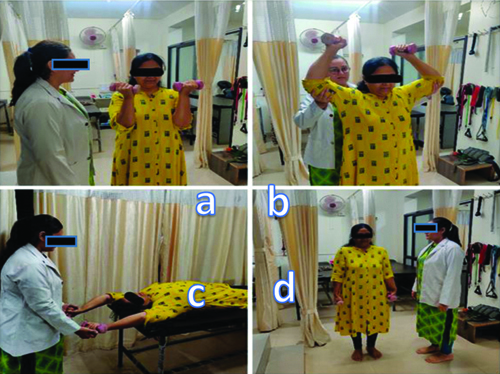 |
| b | Dumbbell press3 sets of 10 repetitions. |
| c | Dumbbell pullover3 sets of 10 repetitions. |
| d | Dumbbell shrugsFor dumbbell shrugs, begin by using a weight of 3 lbs for 3 sets of 10 repetitions. |
| 3 | Stretching exercises |
| Each exercise is done for 30 seconds and repeated three times. | |
| 4 | Telerehabilitation | 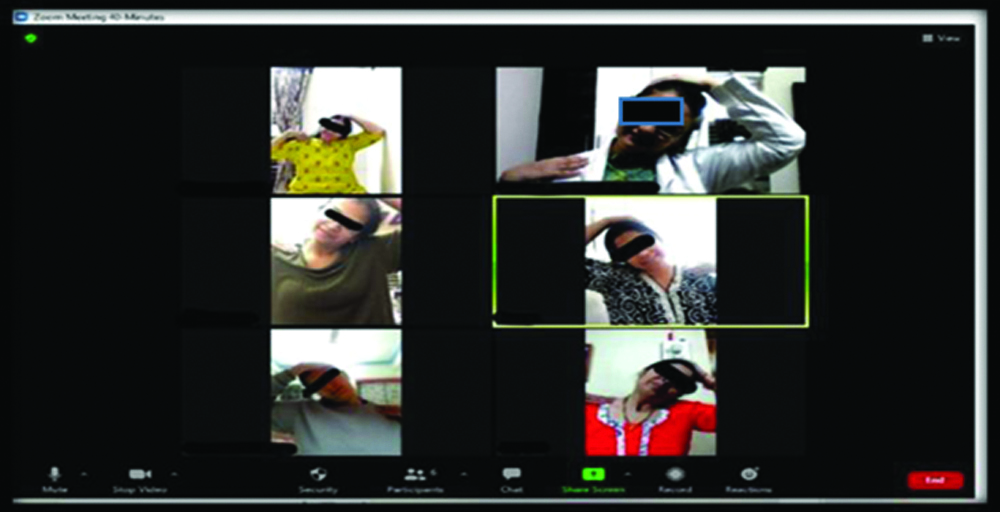 |
Structured exercise programme was set according to the FITT principle.
| Strength training | Frequency | Intensity | Time (Total duration=40 minutes) | Type |
|---|
| Isometric neck exercises | Once a day for 6 days with 1 day recovery period for 4 weeks | Moderate to high | 10 minutes per session.10 seconds hold. Relax. Repeat 5times. | Type: Progressive isometric neck strength exercises in flexion, extension, and rotation, performed in a sitting position. |
| Dynamic exercises for shoulders and upper extremities | Once a day for 6 days with 1 day recovery period for 4 weeks | Moderate to high | Time: 20 minutes per sessionPerformed 3 sets of 10 repetitions for each exercise, allowing for rest between sets. | Type: Dumbbell shrugs, presses, curls, flyes, and pullovers. |
| Stretching of neck and shoulder | Daily incorporating stretching exercises as part of a daily routine to improve flexibility and reduce muscle tightness | Mild to moderate | Time: 10 minutes per session.Holding each stretch for an adequate duration to improve flexibility. 30 seconds and repeated 3 times. | Static stretching for the neck and shoulder muscles. |
Statistical Analysis
Statistical analysis for the present study was done using Statistical Package of Social Sciences (SPSS) version 23 so as to verify the result obtained. For this purpose, data was entered into an excel spread sheet, tabulated and subjected to statistical analysis. Various statistical measures such as mean, frequency, standard deviation were used. Wilcoxon Matched pairs test and dependent t-test were used to compare pretest and post-test VAS, NDI, performance, and MMT scores. The p-value <0.05 (at 5% level of significance).
Results
The study was done on only female homemakers, out of 63 homemakers 50% of them had mild to moderate amount of NP which was found with the help of ICF qualifiers.
Code d230 (carrying out daily routine): 83.84% improvement (n=52)
Code d4103 (sitting): 100.00% improvement (maximum improvement) (n=63)
Code d4104 (standing): 53.12% improvement (n=33)
Code d4105 (bending): 40.86% improvement (minimum improvement) (n=26)
Code d430 (lifting and carrying objects): 50.68% improvement (n=32)
Code d450 (walking): 71.43% improvement (n=45)
[Table/Fig-5] shows Comparison of pretest and post-test VAS scores by Wilcoxon Matched pairs test. A significant difference was observed between pretest and post-test VAS scores (Z=6.7359, p=0.001) at 5% level of significance. It means that, a significant 68.46% reduction was seen in VAS scores after treatment.
Comparison of pre-test and post-test VAS scores (n=63).
| Time points | Mean | SD | Mean Diff. | SD Diff. | % of change | Z-value | p-value |
|---|
| Pretest | 4.97 | 0.94 | 3.40 | 1.25 | 68.46 | 6.7359 | ≤0.001* |
| Post-test | 1.57 | 1.36 |
*p<0.05 Wilcoxon Matched pairs test
[Table/Fig-6] shows Comparison of pretest and post-test NDI scores by dependent t-test. A significant difference was observed between pretest and post-test NDI scores (t=36.0264, p=0.001) at 5% level of significance. It means that, a significant 83.68% reduction was seen in NDI scores after treatment with effect size 0.9570.
Comparison of pretest and post-test NDI scores (n=63).
| Time points | Mean | SD | Mean Diff. | SD Diff. | % of change | t-value | p-value | Effect size |
|---|
| Pretest | 41.45 | 10.53 | 34.68 | 7.46 | 83.68 | 36.0264 | ≤0.001* | 0.9570 |
| Post-test | 6.77 | 5.89 |
*p<0.05 Dependent t-test
[Table/Fig-7] shows the status of b134 (sleep functions), b28010 (pain in head and neck) and nature and extent of different body Structure. In the code b134 majority of the participant scored 0, which means there was no impairment in the sleep function. In code b28010 majority of the participant scored 1, which means there was mild impairment in the structures that caused pain in the neck.
| Codes | Score 0 | % | Score 1 | % | Score 2 | % | Score 3 | % |
|---|
| b134 Sleep functions | n=26 No impairment | 38.3 | n=15 Mild impairment | 25.0 | n=14 Moderate impairement | 23.3 | n=8 Severe impairment | 13.3 |
| b28010 Pain in head and neck | n=7 No impairment | 6.7 | n=36 Mild impairment | 60.0 | n=17 Moderate Impairement | 28.3 | n=3 Severe impairment | 5.0 |
In code s7104 (muscles of head and neck region) majority of the participant had mild impairment in muscles of head and neck region with no change in the structure. In code s7108 (structure of head and neck region, other specified) majority of participant had no impairment with no change in the structure. In code s76000 (cervical vertebral column) majority of the participants had no impairment with no change in the structure.
[Table/Fig-8] shows the Comparison of performance -pretest and performance post test scores (n=63) of different parameters by Wilcoxon Matched pairs test. Significant improvement was seen in carrying out daily routine (p≤0.001), sitting (p=0.0431) standing (p≤0.001), bending (p≤0.001); lifting and carrying objects (p≤0.001) and walking (p=0.0051).
Comparison of performance (pretest) and (post-test) scores (n=63) of different parameters.
| Parameters | Time points | Mean | SD | Median | IQR | % of change | Z-value | p-value |
|---|
| d230 | Pre | 1.7 | 0.8 | 1.0 | 1.0 | 83.84 | 6.6800 | ≤0.001* |
| Post | 0.3 | 0.4 | 0 | 1.0 |
| d4103 | Pre | 0.1 | 0.3 | 0 | 0 | 100.00 | 2.0226 | 0.0431* |
| Post | 0 | 0 | 0 | 0 |
| d4104 | Pre | 0.5 | 0.7 | 0 | 1.0 | 53.12 | 3.4078 | ≤0.001* |
| Post | 0.3 | 0.5 | 0 | 0 |
| d4105 | Pre | 1.6 | 0.9 | 1.0 | 1.0 | 40.86 | 5.0119 | ≤0.001* |
| Post | 0.9 | 0.8 | 1.0 | 1.0 |
| d430 | Pre | 1.2 | 0.8 | 1.0 | 1.0 | 50.68 | 5.1594 | ≤0.001* |
| Post | 0.6 | 0.8 | 0 | 1.0 |
| d450 | Pre | 0.2 | 0.4 | 0 | 0 | 71.43 | 2.8031 | 0.0051* |
| Post | 0.1 | 0.3 | 0 | 0 |
*p<0.05 Wilcoxon Matched pairs test; d230 (carrying out daily routine) d4103 (sitting) d4104 (standing) d4105 (bending) d430 (lifting and carrying objects) d450 (walking)
[Table/Fig-9] shows comparison of pretest and post test scores of different parameters of MMT by Wilcoxon Matched pairs test. It showed a significant improvement in all the muscles of the neck namely, flexors, extensors, right flexors, left flexors, right rotators, and left rotators. Maximum improvement was seen in flexors and extensors and minimum improvement was seen in right and left rotators.
Comparison of pretest and post-test scores (n=63) of different parameters of MMT.
| Parameters | Time points | Mean | SD | Median | IQR | % of change | Z-value | p-value |
|---|
| Flexors | Pretest | 4.3 | 0.5 | 4.0 | 1.0 | -13.33 | 3.6718 | 0.0002* |
| Post-test | 4.8 | 0.4 | 5.0 | 0 |
| Extension | Pretest | 4.3 | 0.5 | 4.0 | 1.0 | -13.33 | 5.0862 | ≤0.001* |
| Post-test | 4.8 | 0.4 | 5.0 | 0 |
| Right flexors | Pretest | 4.3 | 0.5 | 4.0 | 1.0 | -7.42 | 5.0862 | ≤0.001* |
| Post-test | 4.6 | 0.5 | 5.0 | 1.0 |
| Left flexors | Pretest | 4.3 | 0.5 | 4.0 | 1.0 | -7.00 | 3.8230 | ≤0.001* |
| Post-test | 4.6 | 0.5 | 5.0 | 1.0 |
| Right rotators | Pretest | 4.3 | 0.5 | 4.0 | 1.0 | -9.34 | 3.7236 | 0.0002* |
| Post-test | 4.7 | 0.5 | 5.0 | 1.0 |
| Left rotators | Pretest | 4.3 | 0.5 | 4.0 | 1.0 | -9.34 | 4.2857 | ≤0.001* |
| Post-test | 4.7 | 0.5 | 5.0 | 1.0 |
*p<0.05 Wilcoxon Matched pairs test
Discussion
This experimental trial involved 63 subjects, all homemakers with a mean age of 36 years, experiencing non-specific NP. On the first day, individuals with a VAS rating between 2-4 received treatment at the clinical setup in the hospital. They were then instructed to perform prescribed exercises at home daily for the next 29 days, under therapist supervision through telerehabilitation. Additionally, they received ergonomic advice to improve their daily working patterns. The data analysis showed a statistically significant difference in the effectiveness of the interventions for NP reduction, therefore we can reject the null hypothesis, which states no difference. The study found evidence for different intervention effects. Non-specific NP is prevalent among homemakers, leading to activity limitation and participation restriction. Despite extensive literature on non-specific NP, there is a scarcity of documentation on the associated limitations in homemakers in developing countries like India.
The present study found a notable prevalence of sleep impairments (25% mild, 23.3% moderate, 13.3% severe) among homemakers with NP. This aligns with research suggesting that NP can be associated with poorer sleep quality [19]. In a study done on homemakers it was seen that homemakers engage in prolonged housework involving repetitive hand movements, bending, kneeling, and squatting, contributing to MSP [11]. The study emphasised the need for occupational health professionals to consider housework and homemakers in their research and policy agendas, particularly exploring the interaction between specific occupations, housework, and MS symptoms. Most studies indicate a higher incidence of NP among women, and the present study aligns with this trend, as homemakers with an average age of 36 years suffered from non-specific pain [13]. Exercises, specifically neck exercises and isometrics, were employed to alleviate NP in this study. Previous research supports the positive effects of regular exercise in reducing pain and enhancing the body’s endogenous inhibitory systems. Regular exercise is pivotal for boosting overall muscle strength and development. In our recent study, a combination of neck exercises and isometrics proved effective in relieving NP. Lima LV et al., research indicates that regular exercise not only alleviates pain but also reduces NMDA receptor phosphorylation, signifying diminished central facilitation. Furthermore, sustained exercise lowers serotonin transporter expression, raises serotonin levels, and increases opioids within central inhibitory pathways like the PAG and RVM [14]. This underscores exercise’s ability to leverage our innate inhibitory systems for pain relief. In a distinct study, it was observed positive outcomes from a 5-week isometric quadriceps exercise programme, manifesting in increased quadriceps muscle strength, diminished pain, and enhanced functional ability in knee osteoarthritis patients [20].
In the present study, neck isometrics demonstrated positive results by increasing strength and reducing pain in homemakers with non-specific NP. Research indicates that, in addition to clinical exercises, Home Exercise Programmes (HEPs) play a crucial role in alleviating NP and maintaining muscle endurance [21]. Zronek M et al., study further supports this, concluding that HEPs incorporating self-mobilisations or exercises targeting specific spinal levels effectively reduce NP, enhance function, and diminishes disability, ultimately improving quality of life. The combination of HEPs with other conservative interventions yields varying degrees of benefit, as indicated by a range of effect sizes [22].
Traditional rehabilitation can be challenging for homemakers due to time constraints, transportation difficulties, financial burden and accessibility issues. Considering the challenges homemakers face in visiting hospitals regularly, a telerehabilitation approach was adopted, proving effective over 29 days. Telerehabilitation was deemed cost-effective, particularly beneficial for individuals in remote areas with limited access to traditional rehabilitation services [23]. Telerehabilitation offers a sustainable solution to these challenges, making it a promising shift in healthcare delivery. The study helped in reducing travel and increasing the energy efficiency lowering carbon footprint. It fostered social sustainability of homemakers by improving quality of life, reduced caregiver burden & enhanced access to specialists. There are studies that support the present study. Study on Efficacy and long-term sustainability of a telerehabilitation programme for patients with knee osteoarthritis found that telerehabilitation was as effective as in-person therapy and led to improved patient satisfaction and adherence [24]. A systematic review of effectiveness and cost-effectiveness examined the effectiveness and cost-effectiveness of telehealth interventions for older adults with various chronic conditions. It found that telehealth can be an effective and cost-effective alternative to in-person care for many conditions [25].
The study utilised the ICF framework to analyse its impact on disability and pain. The findings showed a moderate amount of pain in 50% of homemakers, aligning with the ICF qualifiers. The ICF model is considered valuable in understanding and addressing specific functional problems related to NP. Andelic N et al., found that the specific functional problems identified in their study align well with the ICF model [26]. Numerous connections to activities and participation categories, including mobility, domestic life, employment, and social and civic life, imply that a comprehensive approach involving a multidisciplinary team is crucial for the rehabilitation of NP-related disability. The present study similarly aligns with the ICF model, identifying specific functional problems in homemakers, thereby offering valuable insights for the rehabilitation of neck-related disability.
The NDI was employed as a reliable tool to measure self-reported NP -related disability [27]. The study contributes to the body of knowledge linking NDI items to the ICF codes, emphasising the comprehensive approach required for NP related disability rehabilitation. Overall, the research offers insights into the challenges faced by homemakers with non-specific NP and the effectiveness of telerehabilitation and targeted exercises in improving their condition [28]. Combining structured neck exercises and ergonomic improvements can effectively reduce NP, increase strength, and improve quality of life in homemakers. The ICF corset may be a useful tool for evaluating NP before and after treatment. Telerehabilitation is a promising treatment option for people who have difficulty attending in-person appointments.
Limitation(s)
The study involved only 63 subjects, which limits the generalisability of the findings to a larger population of homemakers with NP. The intervention lasted only 30 days, which may not be sufficient to determine the long-term effectiveness of the programme. The study only included homemakers with a VAS rating between 2-4 potentially excluding those with more severe or less severe pain. The study did not account for socio-economic factors that may influence pain perception and access to healthcare. The study did not explore the potential role of mental health factors such as stress or anxiety in NP. Pain tolerance and adherence to the exercise programme can vary significantly between individuals.
Conclusion(s)
A telerehabilitation programme combining exercises and ergonomics improved NP in homemakers, suggesting it’s potential and warranting further study. This study not only demonstrated that a combined approach of structured neck exercises and ergonomic interventions effectively reduces pain, increases strength, and life quality in homemakers with NP, but it also contributed to their overall well-being through sustainable practices. By effectively managing NP and preventing future issues, this approach can potentially reduce the need for expensive medical consultations, medications, and even surgeries, promoting long-term financial sustainability for homemakers and their families. Reduced pain and increased strength lead to improved ability to perform daily tasks effectively and efficiently, allowing homemakers to manage chores and responsibilities with greater ease, contributing to their overall well-being and productivity. The incorporation of telerehabilitation empowers homemakers to manage their NP independently, reducing reliance on healthcare professionals and encouraging self-sufficiency and ownership of their health. Telehealth interventions minimise the need for travel and associated carbon emissions, contributing to a more sustainable healthcare system and environment.
*p<0.05 Wilcoxon Matched pairs test
*p<0.05 Dependent t-test
*p<0.05 Wilcoxon Matched pairs test; d230 (carrying out daily routine) d4103 (sitting) d4104 (standing) d4105 (bending) d430 (lifting and carrying objects) d450 (walking)
*p<0.05 Wilcoxon Matched pairs test
[1]. Mishra M, Srivastava AK, Srivastava VK, Prevalence and risk of musculoskeletal pain in rural homemakers of North IndiaMed J DY Patil Univ 2017 10:138-42.10.4103/0975-2870.202092 [Google Scholar] [CrossRef]
[2]. Norouzi S, Tavafian SS, Cousins R, Mokarami H, Study protocol for a randomized controlled trial to improve the quality of life of housewives with musculoskeletal disorders: A health promotion intervention based on a participatory ergonomic approach-the Housewives Ergonomic Intervention (HEI) trialTrials 2021 22:490Available from: https://doi.org/10.1186/s13063-021-05436-w [Google Scholar]
[3]. Hidalgo B, Hall T, Bossert J, Dugeny A, Cagnie B, Pitance L, The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic reviewJ Back Musculoskelet Rehabil 2017 30(6):1149-69.PMCID: PMC581466510.3233/BMR-16961528826164 [Google Scholar] [CrossRef] [PubMed]
[4]. Cohen SP, Hooten WM, Advances in the diagnosis and management of neck painBMJ 2017 358:j322110.1136/bmj.j3221 [Google Scholar] [CrossRef]
[5]. Das B, Prevalence of work-related musculoskeletal disorders among the brick field workers of West Bengal, IndiaArch Environ Occup Health 2014 69(4):231-40.10.1080/19338244.2013.77124924499251 [Google Scholar] [CrossRef] [PubMed]
[6]. Shah DA, Shah DA, Lakhani NP, Prevalence of musculoskeletal pain in bio- pharmaceutical industry workersInt J Health Sci Res 2021 11(11):48-61.10.52403/ijhsr.20211106 [Google Scholar] [CrossRef]
[7]. GBD 2021 Neck Pain CollaboratorsGlobal, regional, and national burden of neck pain, 1990-2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021Lancet Rheumatol 2024 6(3):e142-e155.PMCID: PMC1089795010.1016/S2665-9913(23)00321-138383088 [Google Scholar] [CrossRef] [PubMed]
[8]. Sudarshan RM, Bhattacharya S, Through the magnifying glass: Women’s work and labour force participation in urban DelhiEconomic and Political Weekly 2009 :59-66. [Google Scholar]
[9]. Krishnan R, Prevalence of musculoskeletal pain and its correlates with ergonomic risk factors among middle aged women home makers in Athiyanoor block Panchayat, Thiruvananthapuram 2016 Available from: https://www.semanticscholar.org/paper/Prevalence-of musculoskeletal-pain-and-its-with-in-Krishnan/e68d059002bbbe2600777cc83b30a1d24040ecea [Google Scholar]
[10]. Verdonk P, Hooftman WE, van Veldhoven MJ, Boelens LR, Koppes LL, Work-related fatigue: the specific case of highly educated women in the NetherlandsInt Arch Occup Environ Health 2010 83(3):309-21.Epub 2009 Nov 4. PMCID: PMC282021410.1007/s00420-009-0481-y19888593 [Google Scholar] [CrossRef] [PubMed]
[11]. Habib RR, El Zein K, Hojeij S, Hard work at home: musculoskeletal pain among female homemakersErgonomics 2012 55(2):201-11.Epub 2011 Aug 1710.1080/00140139.2011.57415721846278 [Google Scholar] [CrossRef] [PubMed]
[12]. Häkkinen A, Kautiainen H, Hannonen P, Ylinen J, Strength training and stretching versus stretching only in the treatment of patients with chronic neck pain: A randomized one-year follow-up studyClin Rehabil 2008 22(7):592-600.10.1177/026921550708748618586810 [Google Scholar] [CrossRef] [PubMed]
[13]. Hill J, Lewis M, Papageorgiou AC, Dziedzic K, Croft P, Predicting persistent neck pain: A 1-year follow-up of a population cohortSpine (Phila Pa 1976) 2004 29(15):1648-54.10.1097/01.brs.0000132307.06321.3c15284511 [Google Scholar] [CrossRef] [PubMed]
[14]. Lima LV, Abner TSS, Sluka KA, Does exercise increase or decrease pain? Central mechanisms underlying these two phenomenaJ Physiol 2017 595(13):4141-50.Epub 2017 May 26. PMCID: PMC549189410.1113/JP27335528369946 [Google Scholar] [CrossRef] [PubMed]
[15]. Behera SK, Das S, Xavier AS, Selvarajan S, Anandabaskar N, Indian Council of Medical Research’s National Ethical Guidelines for biomedical and health research involving human participants: The way forward from 2006 to 2017Perspectives in Clinical Research 2019 10(3):108-14. [Google Scholar]
[16]. ICF Core Sets-ICF RESEARCH BRANCH. [website]Available from: https://www.icf-core-sets.org/ [Google Scholar]
[17]. Bertozzi L, Gardenghi I, Turoni F, Villafañe JH, Capra F, Guccione AA, Effect of therapeutic exercise on pain and disability in the management of chronic non-specific neck pain: Systematic review and meta-analysis of randomized trialsPhysical Therapy 2013 93(8):1026-36. [Google Scholar]
[18]. Paraskevopoulos E, Koumantakis GA, Papandreou M, A systematic review of the aerobic exercise program variables for patients with non-specific neck pain: Effectiveness and clinical applicationsInHealthcare 2023 11(3):339 [Google Scholar]
[19]. Lee MK, Oh J, The relationship between sleep quality, neck pain, shoulder pain and disability, physical activity, and health perception among middle-aged women: A cross-sectional studyBMC Womens Health 2022 22(1):186PMCID: PMC912400810.1186/s12905-022-01773-335597981 [Google Scholar] [CrossRef] [PubMed]
[20]. Anwer S, Alghadir A, Effect of isometric quadriceps exercise on muscle strength, pain, and function in patients with knee osteoarthritis: A randomized controlled studyJ Phys Ther Sci 2014 26(5):745-48.Epub 2014 May 29. PMCID: PMC404724310.1589/jpts.26.74524926143 [Google Scholar] [CrossRef] [PubMed]
[21]. Damgaard P, Bartels EM, Ris I, Christensen R, Juul-Kristensen B, The influence of home exercise programs for patients with non-specific neck pain: A systematic review and meta-analysisClin Rehabil 2013 27(3):19-30.10.1177/0269215512448593 [Google Scholar] [CrossRef]
[22]. Zronek M, Sanker H, Newcomb J, Donaldson M, The influence of home exercise programs for patients with non-specific or specific neck pain: A systematic review of the literatureJ Man Manip Ther 2016 24(2):62-73.PMCID: PMC498481310.1179/2042618613Y.000000004727559275 [Google Scholar] [CrossRef] [PubMed]
[23]. Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS, Telerehabilitation: Review of the state-of-the-art and areas of applicationJMIR Rehabil Assist Technol 2017 4(2):e7PMCID: PMC554489210.2196/rehab.751128733271 [Google Scholar] [CrossRef] [PubMed]
[24]. Laufer Y, Laprade MF, Efficacy and sustainability of a telerehabilitation program for knee osteoarthritis patients: A randomized controlled trial with 12-month follow-upArthritis Care and Research 2014 66(11):1647-56. [Google Scholar]
[25]. Khouri H, Aboujaoude R, El-Jardali R, Awada A, Al-Husseini N, Habib AR, Telehealth for older adults: A systematic review of effectiveness and cost-effectivenessJournal of Telemedicine and Telecare 2020 26(12):817-31. [Google Scholar]
[26]. Andelic N, Johansen JB, Bautz-Holter E, Mengshoel AM, Bakke E, Roe C, Linking self-determined functional problems of patients with neck pain to the International Classification of Functioning, Disability, and Health (ICF)Patient Prefer Adherence 2012 6:749-55.Epub 2012 Oct 23. PMCID: PMC348452810.2147/PPA.S3616523118531 [Google Scholar] [CrossRef] [PubMed]
[27]. Vernon H, Mior S, The neck disability index: A study of reliability and validityJ Manipulative Physiol Ther 1991 14(7):409-15.1834753 [Google Scholar] [PubMed]
[28]. Lee HJ, Song JM, Functioning characteristics of patients with neck pain: ICF concept basedJ Kor Phys Ther 2019 31(4):242-47.Available from: https://doi.org/10.18857/jkpt.2019.31.4.242 [Google Scholar]