Oral competence and mastication are strongly dependent on the integrity of the jaw, the condition of the teeth, the periodontium, the masticatory muscles, the tongue and appropriate salivary flow. All of these factors can be affected by surgery and radiation therapy, which are often required for the treatment of head and neck cancer. The affected structures and the degree of resection frequently influence the extent of the resulting impairment. Majority of the structure necessary for mastication can be compromised if a segment of manbible is surgically removed or if its continuity is lost [1].
In general, a resection that preserves mandibular continuity and removes only a portion of the mandible is less debilitating than one that compromises it. Loss of mandibular continuity causes deviation of mandible towards the defect, and mandibular occlusal plane rotated inferiorly. Re-training the muscles to re-establish a favourable occlusal relationship is the fundamental aim of rehabilitation. A PGFP is a conventional mandibular/maxillary prosthesis created for individuals who can achieve a proper mediolateral maximum intercuspal position but are unable to maintain this position over time in order to masticate properly and prevent further deviation [2].
In the present research, the MP of patients who had undergone hemi-mandibulectomy surgery was evaluated before and after receiving an interim guide flange prosthesis. To date, no study has been carried out on the effect of an interim maxillary guidance ramp prosthesis on the MP in patients who have undergone hemi-mandibulectomy. The null hypothesis for the current study is that there will be no difference in MP between pre- and post-mandibular guidance therapy in hemi-mandibulectomy patients, whereas the alternative hypothesis states that there will be a difference in MP pre- and post-mandibular guidance therapy in these patients.
Materials and Methods
A quasi-experimental study was conducted on patients meeting the inclusion criteria selected from the Outpatient Department of the Department of Prosthodontics at Bharati Vidyapeeth Dental College and Hospital in Sangli, Maharashtra, India, from January 2021 to July 2022. This was a time bound study therefore, the sample size was not calculated. A total of 10 subjects were selected based on the inclusion criteria. Institutional Ethical Clearance was obtained, with reference number BV(DU)MC&H/Sangli/IEC/Dissertation2020-21/D43.
Inclusion criteria: Individuals with Cantor and Curtis Class 2 and Class 3 defects with a mouth opening of 2 fingers or more were included in the study.
Exclusion criteria: Individuals with Cantor and Curtis Class 1, 4, 5, or 6 defects, completely edentulous patients, maxillectomy patients, and those who were periodontally compromised were excluded from the study.
The primary outcome measure was to assess the MP based on the following parameters: age, sex, type of defect, and mandibular deviation of patients who had undergone hemi-mandibulectomy surgery. These parameters were evaluated both pre- and post-receiving an interim guide flange prosthesis.
Mandibular deviation: This was measured using a vernier calliper device in the following manner:
- Class 2 defect: The deviation was measured from the maxillary midline to the mandibular midline.
- Class 3 defect: In cases where the mandibular lateral incisors were present, a line was marked 5 mm distal to the maxillary midline toward the unoperated central incisor side. The distance between the mesio-incisal line angle of the mandibular lateral incisor and the marked line on the maxillary central incisor was then measured.
Study Procedure
Steps in the fabrication of the palatal guidance ramp prosthesis: Maxillary and mandibular alginate impressions (Zhermack) were made using stock trays (Jabbar) and were poured with type III dental stone (Kalabhai) to obtain casts [Table/Fig-1a,b]. On the casts, undesirable undercuts were blocked, and clasps were made onto the selected abutment teeth using 19-gauge wire for added retention of the prosthesis. A record base was fabricated on the maxillary cast using Dental Product of India (DPI) cold cure clear acrylic resin [Table/Fig-1a]. Dental modelling wax (Maarc) was then adapted to the record base to create an indentation of the lower teeth in a deviated position [Table/Fig-1c-e].
(a-k) Steps in the fabrication of palatal guidance ramp prosthesis.
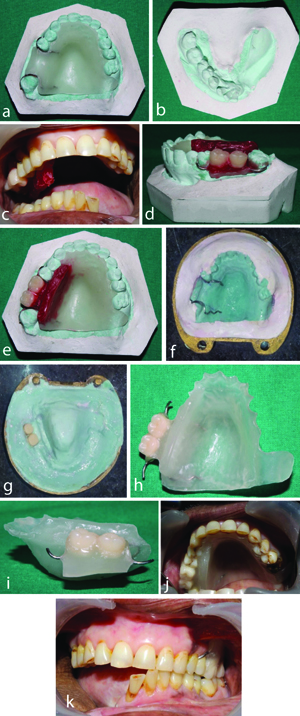
While recording the jaw relationship, the mandible was guided towards the non operated side within the comfortable limits of the subject. This recording was transferred onto a mean value articulator for mounting. The palatal guidance ramp prosthesis was fabricated with (DPI) heat cure acrylic resin using the compression moulding technique [Table/Fig-1f-i].
The prosthesis was then checked to ensure if it seated correctly, and any hindrance if present were removed. After adjustments and smoothing, the prosthesis was inserted [Table/Fig-1j]. The subject was asked to bite in the guided position, ensuring that they could close into the prepared index [Table/Fig-1k]. It is essential to avoid extending the index beyond the level of the maxillary teeth, as doing so could disrupt speech, swallowing, and other oral activities that involve tongue movements [4].
The patient was recalled after eight weeks for the insertion of the prosthesis, ensuring they could close the jaw within their comfortable limits to achieve maximum intercuspation between the upper and lower teeth. The palatal guidance ramp was relined with cold cure acrylic resin (DPI) if required.
Sample collection: A single group of patients was evaluated for pre- and post-mandibular guidance prostheses. Patients were clinically analysed for MP at three different time intervals, and samples will be collected at:
0 day (T0:preprosthesis): Samples were collected before providing the maxillary guidance ramp prosthesis.
8th week (T1): Samples were collected on the 8th week after the insertion of the maxillary guidance ramp prosthesis, with the prosthesis in place.
16th week (T2:postprosthesis): Samples were collected on the 16th week after the insertion, with the prosthesis in place.
Corn flakes (Kellogg’s) were used as the test food substance for the study. A weight of 0.5 g of corn flakes (Kellogg’s) was measured using a weighing machine (Contech) [Table/Fig-2a]. The weighed corn flakes were then given to the subject to chew for 20 strokes [Table/Fig-2b]. The subject was provided with 4 oz of water to thoroughly rinse their mouth and was then asked to expectorate the chewed sample into a kidney tray until all food particles were expelled [Table/Fig-2c,d]. The oral cavity was checked for any remaining food particles, which were collected if, present.
(a-h) Steps involved in sample collection.
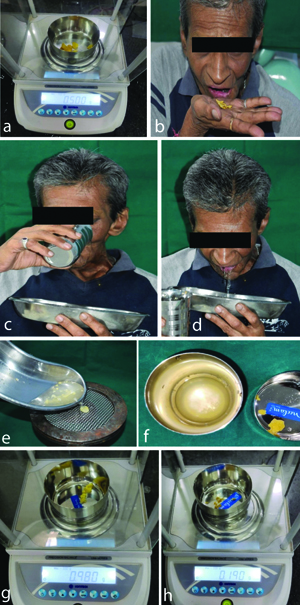
The collected sample was then sieved using a US standard 8-mesh sieve [5], and the sample was gathered [Table/Fig-2e]. The sample collected in the container represented the subject’s masticatory efficiency, while the material collected on the sieve indicated the subject’s masticatory inefficiency [Table/Fig-2f] [1].
The sample collected on the sieve was placed in a bowl, and the wet weight of the sample was then evaluated [Table/Fig-2g]. This sample was incubated in an incubator (Optik) at 37° Celsius for three consecutive days (until the sample became completely dry). The dried sample was then weighed on the weighing machine, and the dry weight was recorded [Table/Fig-2h].
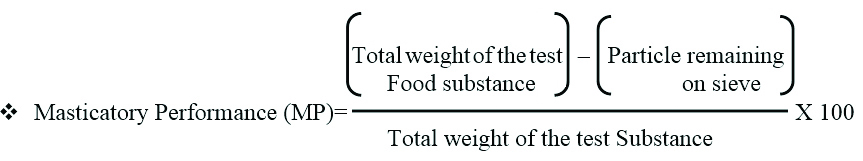
The recorded weight was then used in the following formula to calculate the masticatory efficiency of the subject as a percentage.
Formula [1]:
Statistical Analysis
The data was obtained and entered into Microsoft Excel Version 13. It was subjected to statistical analysis using IBM Statistical Package for Social Science (SPSS) version 21.0. Both descriptive and inferential statistics were applied to the data. The mean and standard deviation were calculated for continuous variables, while frequency analysis was conducted for categorical variables.
To determine the difference in proportions between categorical variables, the Chi-square test of proportions was applied. To compare the MP between T0-T1 and T0-T2 students, a paired t-test was used. All statistical tests were conducted with a confidence interval of 95%, and a p-value of less than 0.05 was considered statistically significant.
Results
In the present study, 10 samples were selected, and the mean age distribution of the study participants was 51.80±11.21 years. It was found that all the study participants were male (n=10). All cancer patient had undergone hemi-mandibulectomy due to squamous cell carcinoma, leading to the loss of mandibular continuity, and showed mandibular deviation toward the affected side. The mean deviation in millimetres observed in the Class 2 and Class 3 study participants was 12.38±10.61 and 16.50±4.94, respectively [Table/Fig-3].
Characteristics of the study participants.
| Participant | Class of defect with midline details | Preoperative midline deviation (in mm) | Postoperative midline deviation (in mm) | T0 {Masticatory Performance (MP) in %} | T1 8th week {Masticatory Performance (MP) in %} | T2 16th week {Masticatory Performance (MP) in %} |
|---|
| 1 | Class 2 | 10 | 5 | 28.00 | 40 | 50 |
| 2 | Class 2 | 11.2 | 3.4 | 24.00 | 44 | 62 |
| 3 | Class 2 | 9.5 | 0.7 | 58.00 | 62 | 72 |
| 4 | Class 2 | 5 | 0 | 4.00 | 28 | 52 |
| 5 | Class 2 | 1.4 | 0 | 10.00 | 46 | 52 |
| 6 | Class 3 | 20 | 2.6 | 4.00 | 16 | 80 |
| 7 | Class 2 | 15 | 4 | 20.00 | 44 | 60 |
| 8 | Class 3 | 18 | 1 | 54.00 | 72 | 78 |
| 9 | Class 2 | 35 | 8 | 26.00 | 38 | 46 |
| 10 | Class 2 | 22 | 3.7 | 34.00 | 40 | 60 |
Out of the 10 participants, 8 (80%) had a Class 2 defect, and 2 (20%) had a Class 3 defect; this difference in proportion was not statistically significant (p>0.05).
The mean MP at T0, T1, and T2 was 26.20±18.66%, 43.00±15.67%, and 61.20±11.93%, respectively. When a comparison of MP between T0 and T1 was conducted, it was found that the difference in mean was -16.80%, and this difference was statistically significant (p<0.001). Similarly, the difference in mean between T0 and T2 was -35.00%, which was also statistically significant (p<0.001) [Table/Fig-4].
Comparison of Masticatory Performance (MP) between T0, T1, T0 and T2.
| Parameter | Mean | N | Std. Deviation | Std. Error mean | Mean difference | T | p-value |
|---|
| Masticatory Performance (MP) | T0 | 26.2000 | 10 | 18.67738 | 5.90631 | -16.80000 | -5.520 | <0.001 |
| 8th week (T1) | 43.0000 | 10 | 15.67021 | 4.95536 |
| Masticatory Performance (MP) | T0 | 26.2000 | 10 | 18.67738 | 5.90631 | -35.00000 | -6.093 | <0.001 |
| 16th week (T2) | 61.2000 | 10 | 11.93315 | 3.77359 |
Values presented in percentages
In pair-wise comparisons of the MP between various time intervals, the differences in mean between T0-T1 (8 weeks) and T0-T2 (16 weeks) were -16.80% and -35.00%, respectively, both of which were statistically significant. When comparing T1 (8 weeks) and T2 (16 weeks), the difference in mean was -18.20%, and this difference was statistically significant (p<0.05). To compare the MP between T0 and T2, a paired t-test was applied [Table/Fig-5].
Pairwise comparison of Masticatory Performance (MP) at different time intervals.
| Multiple comparisons |
|---|
| Dependent variable: Masticatory Performance (MP) |
|---|
| Tukey HSD |
|---|
| (I) Time interval | (J) Time interval | Mean difference (I-J) | Std. Error | p-value | 95% Confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| T0 | 8th week T1 | -16.80000 | 7.00857 | 0.060 | -34.1772 | 0.5772 |
| 16th week T2 | -35.00000* | 7.00857 | <0.001 | -52.3772 | -17.6228* |
| 8th week T1 | 16th week T2 | -18.20000* | 7.00857 | 0.039 | -35.5772 | -0.8228* |
When the MP was compared between the types of defects at T0, T1, and T2, the differences in mean were -3.50, -1.25, and -22.25, respectively. This difference in mean was statistically significant only between Class 2 and Class 3 MP at the 16th week (T2) (p=0.007). To obtain an overall comparison of the MP between all time intervals, Analysis of Variance (ANOVA) with post-hoc Tukey’s test was applied [Table/Fig-6].
Comparison of Masticatory Performance (MP) and type of defect.
| | Type of defect | N | Mean | Std. Deviation | Std. Error mean | Mean difference | T | p-value |
|---|
| Masticatory Performance (MP) | (T0) | Class 2 | 8 | 25.5000 | 16.34451 | 5.77866 | -3.50000 | -0.224 | 0.828 |
| Class 3 | 2 | 29.0000 | 35.35534 | 25.00000 |
| 8th week (T1) | Class 2 | 8 | 42.7500 | 9.55809 | 3.37930 | -1.25000 | -0.095 | 0.927 |
| Class 3 | 2 | 44.0000 | 39.59798 | 28.00000 |
| 16th week (T2) | Class 2 | 8 | 56.7500 | 8.34523 | 2.95048 | -22.25000 | -3.598 | 0.007 |
| Class 3 | 2 | 79.0000 | 1.41421 | 1.00000 |
The pairwise comparison of MP in Class 2 defects at different time intervals revealed differences of -17.25 and -31.25 between T0-T1 and T0-T2, respectively. The difference in mean at T1-T2 was -14.00. The differences in mean were statistically significant between T0-T1 and T0-T2 [Table/Fig-7]. Due to the small sample size for Class 3, no time period-wise comparison was conducted.
Pairwise comparison of Masticatory Performance (MP) in Class 2 defects at different time intervals.
| Multiple comparisons |
|---|
| Dependent variable: Masticatory Performance (MP) Class 2 |
|---|
| Tukey HSD |
|---|
| (I) Time interval | (J) Time interval | Mean difference (I-J) | Std. Error | p-value | 95% Confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| T0 | TI | -17.25000* | 5.97315 | 0.023 | -32.3058 | -2.1942 |
| T2 | -31.25000* | 5.97315 | <0.001 | -46.3058 | -16.1942 |
| T1 | T2 | -14.00000 | 5.97315 | 0.071 | -29.0558 | 1.0558 |
*The mean difference is significant at the 0.05 level
The null hypothesis was rejected, and the alternative hypothesis was accepted because there was a substantial improvement in masticatory function while using the interim guiding flange prosthesis. The results indicated a definitive advantage of using an interim guiding flange prosthesis for patients with a hemi-mandibulectomy.
Discussion
The loss of mandibular continuity disrupts the balance and symmetry of mandibular function, resulting in the deviation of the remnant fragment toward the operative side. The differences in the postsurgical envelope of mobility and the severity of deviation are determined by a variety of complex and interconnected variables. Generally, patients suffering extensive soft-tissue loss, resulting in tight wound closure, those receiving a full course of radiation therapy, and those requiring a classical radical neck dissection experience the most severe mandibular deviation and dysfunction [4].
The earlier mandibular guidance therapy is initiated, more successful is the outcome. If patient has undergone extensive resection, including a classical radical neck dissection, and has received radiation therapy, the guidance procedures become significantly more challenging if a considerable amount of time has elapsed since the surgical procedure. This may lead to a compromised occlusal relationship. The guidance prosthesis can be constructed for either the mandible or the maxilla. All guidance prosthesis are utilised on an interim basis until acceptable occlusal relationships and proper proprioception are re-established [5].
Few studies have been carried out to evaluate the MP in mandibulectomy patients pre- and post-definitive prosthesis. Additionally, there are studies related to the MP in pre- and post-complete denture prosthesis in edentulous patients [6]. However, none of the studies have been carried out using interim prosthesis in mandibulectomy patients.
Yurkstas A and Manly RS studied the value of different test foods in estimating masticatory ability between natural dentition and complete dentures. They concluded that the food substances needed to meet the following criteria: they should be soft to avoid local tissue injury or pain; pliable to allow for mastication; particulate for sieve analysis; and acceptable in taste. The corn flakes (Kellogg’s) used in the present study satisfied these criteria, and as shown by the data, the chips are an acceptable test substance for head and neck cancer patients [7].
Shibuya Y et al., studied the evaluation of masticatory function after mandibulectomy using colour-changing chewing gum. They concluded that the colour-changing gum is effective in evaluating MP after mandibulectomy [8]. Marunick MT et al., investigated masticatory function in patients who underwent hemi-mandibulectomy. They concluded that surgery resulting in the loss of mandibular continuity may cause impairment of mastication that cannot be consistently reversed by prosthetic rehabilitation, which was not in accordance with the results of this study [1].
Curtis DA et al., studied the modelling of jaw biomechanics in reconstructed mandibulectomy patients. They concluded that there were no significant differences in occlusal force between the six mandibulectomy subjects with bony reconstruction of the mandible and six non cancer subjects with an intact mandible. However, the average molar and incisal occlusal force values were 22% and 32% less, respectively, in mandibulectomy subjects with bony reconstruction [9].
Ihara K and Goto M investigated masticatory function following jaw resection and subsequent rehabilitation with dental implants. Their study aimed to assess the effectiveness of prosthodontic treatment in restoring masticatory function. They found significant differences in the action potential amplitudes of the masseter muscle between patients who underwent jaw resection and those in other groups. The study concluded that appropriate soft-tissue reconstruction combined with dental implants can nearly restore masticatory function to normal levels, even in patients who have had jaw resections [10].
Hannam AG et al., studied the simulated jaw dynamics in models of segmental mandibular resection versus resection with alloplastic reconstruction. They concluded that composite mandibular resection resulting in mandibular discontinuity can affect jaw motion, occlusal forces, and mastication, regardless of whether the jaw is reconstructed [11].
Patil PG and Patil SP investigated the use of a guide flange prosthesis for the early management of reconstructed hemi-mandibulectomy. They concluded that surgical resection of the mandible, often due to benign or malignant tumours, is the primary cause of mandibular deviation. This case report describes the early prosthodontic treatment of a patient who underwent hemi-mandibulectomy, using a modified mandibular guide flange prosthesis. The prosthesis helps the patient achieve proper mandibular movement without deviation during activities such as speaking and mastication [2].
Komagamine Y explored the relationship between MP, assessed using colour-changeable chewing gum, and jaw movements. The study aimed to determine the connection between the effectiveness of mastication, as measured by the colour change in chewing gum, and the motions of the mandible [12]. Hazari P et al., compared the MP and efficiency of complete dentures made from high-impact and flexible resins. They concluded that for patients with significant tooth loss, restoring masticatory function and aesthetics is a primary concern for prosthodontists. This study used standardised mesh sieves to evaluate and compare the performance and efficiency of different denture materials [13].
Bahri R et al., examined the management of hemi-mandibulectomy patients using a guidance flange prosthesis through a combination technique. The study concluded that a guide flange prosthesis can serve as a training tool to achieve optimal occlusal relationships and maximise masticatory efficiency. Early prosthodontic intervention is crucial for establishing better occlusal contacts, as redirecting the mandible to minimise deviation becomes more challenging over time [14].
Hazra R et al., studied the mandibular guidance prosthesis using both conventional and innovative approaches and concluded that patients should maintain central occlusion for mastication, which can be achieved with a Guide Flange Prosthesis (GFP). When a suitable intercuspal position is obtained, occlusal equilibration is typically required to maintain the mandibular position [15]. According to Liu R et al., the occlusal ramp used as a definitive prosthesis for rehabilitation after a mandibulectomy and its effects on mastication were studied with and without the prosthesis. His study concluded that MP was significantly improved with the definitive prosthesis in place [16].
The findings of the present study align with those of Liu R et al., who demonstrated that MP significantly improved in participants with mandibular deviation post-mandibulectomy when utilising a definitive occlusal ramp prosthesis. In contrast, the current study employed an interim guide flange prosthesis and similarly observed enhancements in masticatory function [16].
This study demonstrated that MP can be effectively restored in post-mandibulectomy patients through the use of an interim guide flange prosthesis to correct mandibular deviation. Successful rehabilitation of head and neck cancer patients necessitates a collaborative effort among oral medicine specialists, oncology surgeons, oral surgeons, and prosthodontists, along with extensive pre- and post-surgical treatment planning.
Limitation(s)
As the present study was time-bound, only a limited number of subjects were analysed. Additionally, since only males were included in the study, gender differences could not be assessed.
Conclusion(s)
Based on the findings of this clinical study, the following conclusions were drawn: The use of guided flange prosthesis therapy significantly improved MP. Additionally, continued use of the guided flange prosthesis over a longer period led to further improvements in MP. Continuing the present research in the future and increasing sample sizes will provide greater clarity regarding MP.
Values presented in percentages
*The mean difference is significant at the 0.05 level