qRBBB: A Sinister ECG Pattern for Poor Outcome
Maharshi Patel1, Satish Mahajan2
1 Resident, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Wardha, Maharashtra, India.
2 Professor, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Maharshi Patel, Resident, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Wardha-442004, Maharashtra, India.
E-mail: maharship083@gmail.com
Acute coronary syndrome, Electrocardiogram, Right bundle branch block
Dear Editor,
A 40-year-old male patient presented with complaints of chest pain for one day, which was retrosternal, radiating to the left shoulder, squeesing type, and associated with uneasiness and sweating. The patient was a known case of systemic hypertension for 10 years and was on tablet amlodipine 5 mg OD. The patient had no previous history of such episodes.
On general examination, the pulse was 68/min, blood pressure was 140/90 mmHg, respiratory rate was 20 cycles/min, and Jugular Venous Pressure (JVP) was 6 cm of water. There was no pallor, cyanosis, icterus, clubbing, lymphadenopathy, or oedema. In the cardiovascular system, S1 and S2 were heard, and there was no murmur. In the respiratory system, bilateral air entry was present without any adventitious breath sounds.
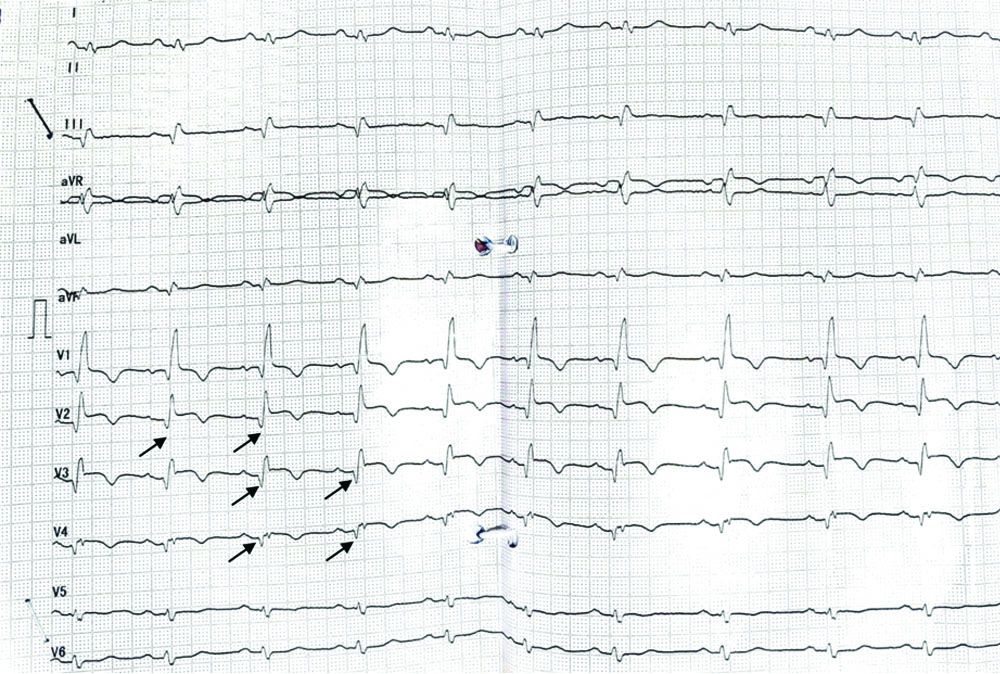
The Electrocardiogram (ECG) showed a qRBBB pattern with ST elevation and T wave inversion in leads V1, V2, V3, V4, and poor progression of the R wave [Table/Fig-1]. Laboratory investigations showed raised cardiac biomarkers, i.e., Creatine Kinase-MB-45 (CKMB) U/L, Troponin-I-30 ng/dL.
Electrocardiography (ECG) showing qRBBB pattern.
A diagnosis of anteroseptal wall Myocardial Infarction (MI) was made, and the patient was given injection (inj.) LOMOH 0.6 mL subcutaneous (Sc) stat and a loading dose of tab ecosprin 300 mg stat, tab clopidogrel 300 mg stat, tablet (tab.) atorvastatin 80 mg stat. The patient was started on anticoagulant inj. lomoh 0.6 mL Sc BD, dual antiplatelet agent tab ecosprin 75 mg OD, tab clopidogrel 75 mg OD, statin tab atorvastatin 40 mg hs, nitrates tab sorbitrate 5 mg SL SOS. 2D-echo showed moderate Left Ventricular (LV) systolic dysfunction, anterior and antero-septal wall hypokinesia, and the presence of regional wall motion abnormalities with Left Ventricular Ejection Fraction (LVEF) of 40%. Coronary angiography was done the next day, revealing 70% stenosis in the proximal Left Anterior Descending artery (LAD), 90% stenosis in the proximal Left Circumflex artery (LCxA), 100% occlusion in proximal OM, and 100% occlusion in the mid RCA. The patient was advised Coronary Artery Bypass Graft (CABG).
Acute Anterior Wall Myocardial Infarction (AWMI) with Right Bundle Branch Block (qRBBB) and Q waves in right precordial leads in the ECG is a rare but sinister form of acute coronary syndrome that indicates proximal occlusion of the LAD artery along with septal arteries. The majority of patients who have an antero-septal infarction have aberrant Q waves in the right precordial leads during RBBB, displaying the typical qRBBB pattern due to delayed activation of the right ventricle. In certain individuals with antero-septal MI, early depolarisation of the right ventricular free wall may disguise the aberrant Q waves [1,2].
According to recent studies, patients with qRBBB AWMI have a high incidence of heart failure, cardiogenic shock, ventricular arrhythmias, and complete heart block [3,4]. The in-hospital mortality rate of qRBBB AWMI ranges from 24% to 42.6%, which is four times higher than that of non-qRBBB AWMI, which is 11%. One of the ECG predictors of mortality in qRBBB AWMI is the extreme deviation of the QRS axis to the right (180 to 269 degrees), reflecting severe septal involvement and Left Ventricle (LV) dysfunction [3,4]. Other ECG features that may suggest qRBBB AWMI are ST segment elevation in anterior leads, QR pattern in V1, and ST segment depression in inferior leads. However, these findings may not be specific or sensitive enough to diagnose qRBBB AWMI, especially in the presence of other confounding factors such as pre-existing RBBB, LV hypertrophy, or previous myocardial infarction. Therefore, a high index of suspicion and careful ECG analysis are required to identify qRBBB AWMI [3,5].
Therefore, it is imperative to recognise this ECG pattern early and initiate prompt re-perfusion therapy to improve the outcomes of these patients.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 13, 2023
Manual Googling: Sep 19, 2023
iThenticate Software: Sep 25, 2023 (13%)
[1]. Rosenbaum MB, Girotti LA, Lázzari JO, Halpern MS, Elizari MV, Abnormal Q waves in right sided chest leads provoked by onset of right bundle-branch block in patients with anteroseptal infarctionBr Heart J 1982 47(3):227-32. [Google Scholar]
[2]. Pozen JM, Mankad AK, Owens JT, Jovin IS, New right bundle branch block as a criterion for emergent coronary angiographyN Am J Med Sci 2015 7(12):569-71. [Google Scholar]
[3]. Paul A, Bhatia KS, Alex AG, Thomson VS, Mani T, Sharathbabu NM, Electrocardiographic predictors of mortality in acute anterior wall myocardial infarction with right bundle branch block and right precordial Q-Waves (qRBBB)Can J Cardiol 2020 36(11):1764-69. [Google Scholar]
[4]. Klein A, Baranchuk A, Identification of high-risk patients based on electrocardiogram during acute anterior ST-Elevation myocardial infarction: The qRBBB patternCan J Cardiol 2020 36(11):1708-09. [Google Scholar]
[5]. Widimsky P, Rohác F, Štásek J, Kala P, Rokyta R, Kuzmanov B, Primary angioplasty in acute myocardial infarction with right bundle branch block: Should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy?Eur Heart J 2012 33(1):86-95. [Google Scholar]