The route to an individual’s general well-being, health and quality of life begins with good oral health [1]. A study conducted by the World Health Organisation (WHO) in 2021, titled the Global Oral Health Status Report, concluded that about 3.5 billion people worldwide are suffering from oral health issues [2]. With the increase in age and edentulism, the health, immunity and quality of life of individuals have deteriorated [3]. The host’s dietary intake and overall state of health have a substantial effect on the oral microbiota. The advent of acrylic resins as denture base resins has revolutionised prosthetic treatment modalities, significantly increasing the number of patients seeking rehabilitation [4].
An erythematous inflammation of the mucosal areas covered by dentures is the hallmark of denture stomatitis, a common inflammatory reaction in individuals who wear dentures. Candida albicans is the primary aetiological agent of this complex clinical entity and treatments for denture stomatitis linked to Candida have been proposed [5].
Denture stomatitis is a prevalent inflammatory response among denture wearers. Throughout history, many communities worldwide have employed herbal hygiene practices. The development of plant-based medicines and Ayurveda to treat various illnesses and maintain health through daily experiences is part of India’s cultural legacy and is being utilised as complementary or alternative medicine globally. Chewing neem sticks (Azadirachta indica) is still practiced in rural India as a substitute for toothbrushes. The triple myrobalans known as ‘Triphala’ have been widely utilised in Ayurveda due to their antibacterial and anticariogenic properties [6].
Antifungal medications are limited and treatment may result in resistance, recurrence, or adverse effects. Consequently, novel therapeutic approaches are required and natural remedies may prove to be highly beneficial. When a patient has extensive tooth decay, conventional methods alone are insufficient; additional medications with antifungal qualities are needed to eradicate the candidal reservoir. As antibiotic resistance increases, we must turn our attention to holistic approaches to combat infections [7].
In addition to herbal remedies, a number of researchers have proposed that probiotics, or friendly bacteria, may improve native flora and contribute to dental health. According to the World Health Organisation (WHO) (2001), “Probiotic refers to live microorganisms which, when administered in adequate amounts, confer health benefits on the host” [8]. Probiotics are naturally present in fermented dairy products like yogurt and cheese. Organisms commonly used in probiotics include certain species of Lactobacilli, Streptococcus and Bifidobacteria. In addition to regulating the bacterial population to preserve a healthy ecosystem, probiotics possess immunomodulatory properties that include modulating humoral and cellular immune responses and stimulating non specific immunity [9,10].
With the increasing number of patients suffering from denture stomatitis and the immunocompromised status of their health, probiotics and Triphala have emerged as a boon against Candida growth. However, due to a lack of awareness, probiotics are not frequently utilised in clinical dental practices. This necessitates action, as the incorporation of probiotics into dentistry could simultaneously enhance dental and systemic health in humans, serving as a potential remedy for health promotion [11]. Thus, the current investigation was designed to evaluate and compare the antimicrobial efficacy of probiotics and herbal oral rinse (Triphala) against Candida, as well as to assess improvements in oral hygiene status.
Materials and Methods
The present randomised double-blinded study clinical study was conducted in the Department of Prosthodontics at Maharishi Markandeshwar College of Dental Sciences and Research in Mullana, Ambala, Haryana, India, between March 2023 and May 2023. The study was approved by the Institutional Research Committee and the Institutional Ethical Committee (Project No: 1782).
Sample size calculation: Using Open Epi software version 3, with a 95% confidence interval and 80% research power, the sample size for the study was calculated. Each group consisted of 28 samples, which were rounded up to 30 samples per group.
Inclusion criteria: Completely edentulous and systemically healthy subjects aged over 55 years who consented to participate in the study visits were included.
Exclusion criteria: Subjects who have used antifungal agents and/or antiseptic mouthwashes in the last six months, as well as those who report the consumption of probiotics, were excluded. Additionally, subjects with a medical or pharmacological history that could jeopardise the conduct of the study, as well as those who have received antibiotic therapy in the previous three months, were also excluded.
Study Procedure
The study was conducted on 60 completely edentulous patients aged over 55 years who attended the prosthodontics outpatient unit. The trial subjects were randomly divided into two groups (n=30 each, designated as Group-A and B) using simple random sampling via a random number table method. Each group was randomly assigned one material (Probiotics, Novobiotic capsule from Alkem Laboratories and Triphala from Patanjali) through a lottery method. In this double-blind study, the investigator provided each patient with the prescribed rinse in a sealed box without disclosing the precise contents of the rinse. Before beginning the sample collection process, a comprehensive health history of each patient was obtained. Written consent was secured from the patients in their native language.
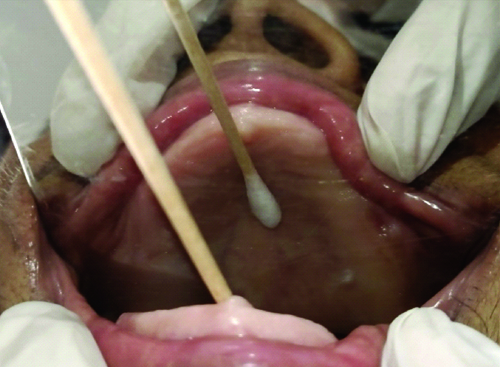
Group allocation: For Group-A Probiotics, patients were advised to pour the contents of the probiotic capsule onto the palatal surface of their dentures and wear the denture for half an hour daily for eight weeks [12]. In Group-B, Triphala, patients were instructed to rinse their mouths with a capful of Triphala (20-30 grams) for 30 seconds once daily in the morning and then wear the denture. Patients were periodically checked to ensure they were following the procedure and were recalled after eight weeks. The first sample was collected at baseline. Sample collection was performed by rubbing sterile cotton swabs across the palatal mucosa for 10 seconds [Table/Fig-1]. The sample taken with the cotton swab was placed in sterile, plugged test tubes. The test tubes were sent to the laboratory in sterile bags within four hours to maintain the vitality of the cells.
Sample collection from patient’s palate.
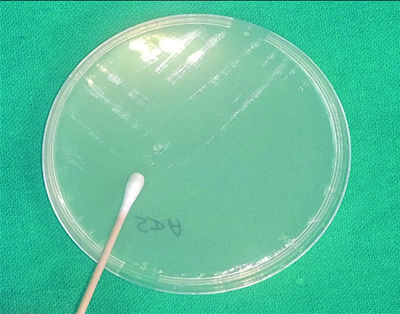
The agar used for the study was Sabouraud Dextrose Agar with Chloramphenicol. Chloramphenicol was added to the agar to eliminate bacterial growth, which can lead to inaccurate readings. The agar was stored in a refrigerator at -4°C. Prior to use, the agar was removed from refrigeration and kept in a BOD incubator for about 3-4 hours to reach room temperature. The petri dishes were autoclaved at 121°C for 30 minutes before preparing the agar for inoculation. The agar was passed over a flame for 5 to 10 seconds to remove any moisture present, as moisture can alter growth. The sample was inoculated onto the agar plate by dividing the plate into four quadrants and then covering the surface using a zigzag streak inoculation method [Table/Fig-1]. The agar plates were then incubated in the BOD incubator at a temperature of 37°C±2°C for 48 hours. The number of Candida colonies was counted using a digital colony counter as Colonies-forming Units (CFU).
Sample collection: The sample collection, conducted after eight weeks, involves rubbing sterile cotton swabs across the palatal mucosa for 10 seconds. The samples taken with the cotton swabs are then placed in sterile, plugged test tubes.
Transfer of sample: The sample taken in the test tube was sent to the laboratory in sterile bags within four hours to maintain the vitality of the cells.
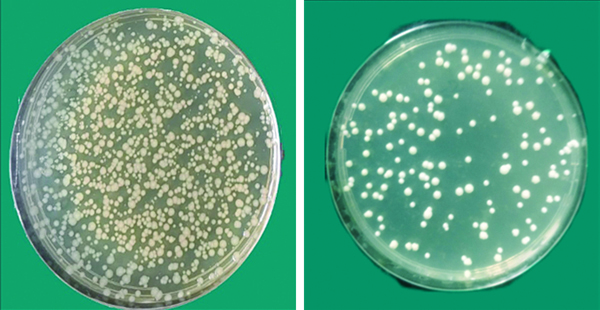
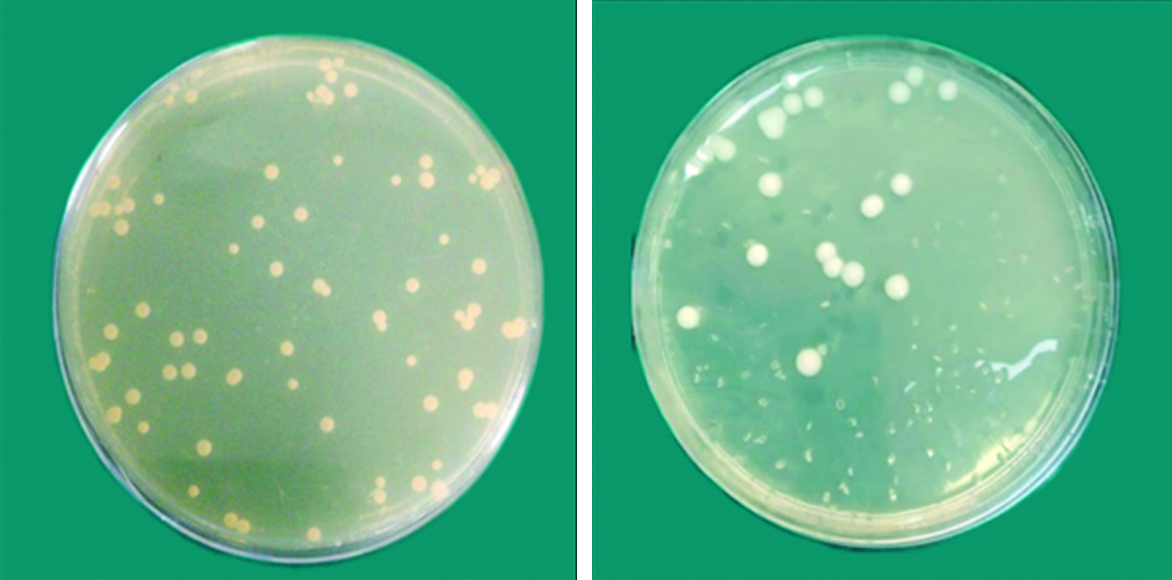
Microbiology study of samples: The number of Candida colonies was scored and counted using a digital colony counter, resulting in the measurement of CFU. The CFUs were then counted with the colony counter and the results obtained were compared using statistical analysis [Table/Fig-2,3,4 and 5].
Inoculating the swab into agar.
Antimicrobial efficacy of Group-A against Candida albicans (before and after).
Antimicrobial efficacy of Group-B against Candida albicans (before and after).
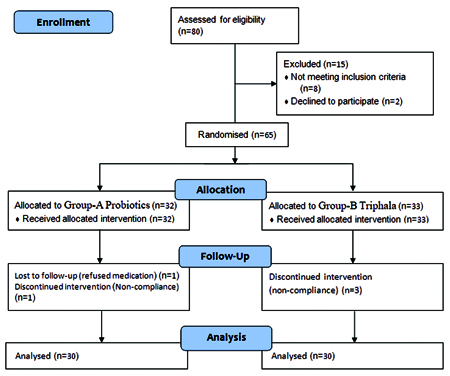
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) software, version 22.0 (Chicago, IL, USA), was used to conduct the statistical analysis. To compare the groups, statistical analysis was performed on the obtained data. For pair-wise comparisons, the Mann-Whitney U test was employed, while the Wilcoxon matched-pairs test was used for group comparisons. The significance level was set at p<0.05.
Results
The mean age of patients in Group-A was 61±3 years, while in Group-B it was 60±2 years, with a similar gender distribution: Group-A consisted of 18 (60%) females and 12 (40%) males, while Group-B had 17 (56.66%) females and 13 (43.33%) males.
The average CFU per mm2 varied significantly based on the results in both groups before and after the sample was taken over a duration of eight weeks (p=0.001) [Table/Fig-6]. The disparity in the standard deviation values between the two groups may be attributed to varied patient selection.
Intragroup comparison of colony forming units among two groups.
| Parameters | n | Mean | Std. Deviation | 95% Confidence interval for mean | p-value |
|---|
| Lower bound | Upper bound |
|---|
| Probiotic | Before | 30 | 44.70 | 72.519 | 17.62 | 71.78 | 0.001* |
| After | 30 | 24.70 | 58.740 | 2.77 | 46.63 |
| Triphala | Before | 30 | 79.60 | 271.458 | -21.76 | 180.96 | 0.001* |
| After | 30 | 50.67 | 196.422 | -22.68 | 124.01 |
Wilcoxon paired signed rank test, level of significance set at p<0.05; *significant
For the intergroup comparison, the Mann-Whitney U test was employed and the results were non significant (p>0.05) [Table/Fig-7]. This signifies that both agents were effective against Candida species. However, Triphala demonstrated higher efficacy than probiotics, as the mean reduction in CFUs was significantly greater for Triphala (p=0.021) [Table/Fig-8].
Intergroup comparison of colony forming units for two groups.
| Parameters | n | Mean | Std. Deviation | 95% Confidence interval for mean | p-value |
|---|
| Lower bound | Upper bound |
|---|
| Before | Probiotic | 30 | 44.70 | 72.519 | 17.62 | 71.78 | 0.499 |
| Triphala | 30 | 79.60 | 271.458 | -21.76 | 180.96 |
| After | Probiotic | 30 | 24.70 | 58.740 | 2.77 | 46.63 | 0.491 |
| Triphala | 30 | 50.67 | 196.422 | -22.68 | 124.01 |
Mann-Whitney u test, level of significance set at p<0.05
Comparison of mean reduction in CFU for Group-A and Group-B.
| Parameters | Paired differences | t | df | Sig. (2-tailed) |
|---|
| Mean | Std. Deviation | Std. Error mean | 95% Confidence interval of the difference |
|---|
| Lower | Upper |
|---|
| Probiotics | Before-after | 20.00 | 13.779 | 5.679 | 8.385 | 31.615 | 3.52 | 29 | 0.021 |
| Triphala | Before-After | 28.93 | 75.036 | 20.02 | -4.98 | 76.91 | 1.79 | 29 |
Wilcoxon paired signed rank test, level of significance set at p<0.05
Discussion
The present study compared the efficacy of probiotic herbal oral rinses (Triphala) against Candida species in patients who wear dentures. The results obtained showed that both materials were effective against Candida species. One of the major clinical manifestations of oral candidiasis is denture stomatitis, which occurs when a removable prosthesis is inserted into the oral cavity, causing various changes in the oral environment that may negatively impact the integrity of oral tissues. In 20-40% of healthy patients, Candida albicans is present as commensal flora; in 60% of immunocompromised individuals, it becomes the predominant flora [6,13]. One common disorder affecting denture wearers is denture stomatitis, characterised by erythema and inflammation of the oral mucosal tissues. Although the aetiology is multifactorial, the components of denture biofilm, such as C. albicans, are fundamental to the development of candidiasis [14].
Various disinfectants are used on impressions to avoid the transfer of infections from the clinical to the laboratory step [15]. The colonisation of Candida begins with yeast proliferation. In the oral cavity among denture wearers, this proliferation starts in the space between the palatal mucosa and the maxillary denture.
Since the action of antifungal agents may be limited by their penetration and chemical reactions within the extracellular polymeric material that constitutes the biofilm matrix, there is a need for newer agents derived from natural resources that can inhibit the growth of microorganisms within the biofilm and enhance effective alternative therapeutic modalities [16]. Recently, incorporating medicinal plant extracts into biomaterials has gained popularity as a natural substitute with potent antifungal properties [17].
The concept of beneficial bacteria in probiotics was revolutionised by Nobel Prize winner Elie Metchnikoff, who demonstrated that the administration of probiotics can significantly improve an individual’s gastrointestinal health, potentially increasing lifespan [18]. The most common bacteria found in probiotics are Lactobacillus and Bifidobacterium, which are recognised as “Generally Regarded As Safe (GRAS).” The mechanisms by which probiotics act against oral pathogens occur through three primary methods: creating antagonism with the pathogens by modulating the biofilm composition, aggregating with oral bacteria to alter the biofilm composition and reduce virulence and interfering with oral epithelial cells to strengthen the barrier function of the epithelium while modulating both innate and adaptive immune responses [14].
In 2013, the Food and Drug Administration (FDA) classified probiotics as biotherapeutic drugs and provided a list of populations at risk from probiotics. These populations include pregnant women, immunosuppressed patients, individuals with structural heart defects, inpatients and those with weak bowel walls. However, if risks do occur, they are typically associated with patients consuming doses above the permissible limits [19]. Therefore, patients with systemic conditions were excluded from this study after thorough history taking.
Triphala has been used in the ancient Indian medical system of Ayurveda for many years. It is prepared by carefully combining equal proportions of three herbal fruits: Terminalia belerica, Terminalia chebula and Phyllanthus emblica. Triphala is known to have multiple beneficial effects on health, especially regarding digestion. It is a potent antioxidant, antimicrobial, antidiabetic and immune modulator. Biradar YS et al., conducted a chemical analysis of Triphala and found that its primary constituents include flavonoids, chebulic acid and tannic acid [20]. The tannins present in Triphala may limit the number of bacteria during the early stages of plaque formation, enhancing the physical clearance of germs from the oral cavity through aggregate formation and making them less accessible for binding to the tooth surface. Certain proteins are known to have a strong binding affinity for tannins, which causes the proteins to precipitate.
Triphala mouthwash is a good substitute for the gold standard Chlorhexidine (CHX) mouthwash, as it did not demonstrate any negative effects in any of the trials evaluated. Moreover, the majority of research indicates that Triphala mouthwash can be utilised as an alternative because it is economical, accessible and patient-friendly [21-24].
Both probiotics and Triphala are over-the-counter products that are easily accessible. These substances have been reported to be safe, with negligible side-effects, if any [25]. Experimental evidence supporting the immunomodulatory action of Triphala was provided by Srikumar R et al., [24]. Their findings clarified that using Triphala can raise Total Leukocyte Count (TLC) levels, which lowers glucocorticoid levels and boosts immunity by decreasing the number of pathogenic Candida [24]. A study by Shetty PJ et al., compared the anticandidal properties of water (control), cashew leaf, aloe vera, Triphala and denture cleaning pills on heat-polymerised acrylic complete dentures [26]. In line with the current investigation, it was determined that using Triphala churna and denture cleaning tablets resulted in a statistically significant decrease in Candida counts. The gallic acid components of Triphala are responsible for its anticandidal activity and the aqueous, ethyl acetate and ethanolic fractions of Terminalia chebula have been demonstrated to have a repressive effect on Candida species [27].
Antibacterial and antifungal drugs that are injected systemically have raised hopes for the containment of these illnesses. However, recent reports of resistance have dampened dental practitioners’ enthusiasm for using these agents, leading them to continue their search for the ideal mouth rinse. Consequently, a variety of topical antimicrobials became the focus of investigation in an effort to prevent fungal overgrowth in the oral cavity [5]. The present study aimed to compare the efficacy of probiotics with popular and commercially available antibacterial medications, such as herbal oral rinses, against Candida albicans in the oral cavity. The results of the present study suggested that the reagents were effective against C. albicans when compared with the baseline after eight weeks, which is in agreement with an in-vivo study conducted by Ishikawa KH et al., [12]. In denture-wearing patients, it was shown that the efficacy of probiotic bacteria increases with the addition of multispecies bacterial strains to the probiotics. In his study, which lasted about five weeks, he demonstrated that Candida colonies were reduced in 83.3% of the participants. The strains that proved to be most potent against Candida were L. rhamnosus, L. acidophilus and B. bifidum. In the study conducted by Ramachandran VS et al., the antimicrobial effect of Triphala was assessed and they concluded that the reduction in biofilm formation by Triphala was significant [28]. Similarly, in the present study, Triphala caused a reduction in the CFU of Candida.
For the sample collection process, a sterile cotton swab was moved across the palate for approximately 10 seconds at baseline and after eight weeks of experimental time. This duration ensured that specimen collection was conducted thoroughly and not hastily, which could lead to inaccurate colony counts. According to Ahluwalia G et al., and Daniluk T et al., this time is adequate for the cotton swab to absorb the palatal secretions sufficiently for proper sample collection [29,30]. A comparative evaluation of similar studies has been provided in [Table/Fig-9] [5,23,31].
Comparison with similar studies [5,23,31].
| S. No. | Author name and year | Place of study | No. of subjects | Interventions | Parameters used | Conclusion |
|---|
| 1 | Mishra R et al., 2016 [5] | Lucknow | n=60 | Group-A: probiotic mint tablet Group-B: chlorhexidine digluconate oral rinse (0.2%). Group-C: herbal oral rinse | C. albicans CFU per millilitre | Probiotic rinse was equally efficient as 0.2% chlorhexidine digluconate rinse in reducing C. albicans counts |
| 2 | Deshmukh MA et al., 2017 [31] | Maharashtra | n=45 | Group-1- HiOra mouthwashGroup-2- CHX mouthwashGroup-3- Probiotic mouthwash | Gingival health, oral hygiene status and plaque accumulation | Mouthwashes containing herbs and probiotics can be useful substitutes for CHX that have less adverse effects |
| 3 | Raja BK and Devi K, 2023 [23] | Tamil Nadu | PubMed, PubMed Central, Campbell systematic review, Cochrane, Embase, Google Scholar and Scopus | Includes only randomised control trials comparing Triphala to CHX or placebo | Triphala when compared with placebos for gingival, plaque and modified plaque indices | Triphala mouthwash is more effective than placebo mouthwashes in reducing gingivitis |
| 4 | Present study | Mullana | n=60 | Group-A (Probiotics group) and Group-B (Triphala group) | C. albicans Colony-Forming Unit (CFU) per milliliter | Probiotics and Triphala showed significant reduction in CFU after their usage for eight weeks of time |
Limitation(s)
The conformity of product usage is solely based on the patient’s statements. Additionally, the impact of probiotics and Triphala on the patient’s overall health has not been determined. Furthermore, the method of intervention was not standardised in either group; Triphala was used as an oral rinse, while the probiotic was applied by pouring it onto the palatal surface of the denture.
Conclusion(s)
Within the parameters of the research, it can be stated that both agents were effective in improving oral health. However, the herbal oral rinse (Triphala) was more effective than probiotics against Candida albicans in denture-wearing patients. To determine the precise therapeutic mechanisms of these mouth rinses, a longer-term study with a larger sample size must be conducted.
Wilcoxon paired signed rank test, level of significance set at p<0.05; *significant
Mann-Whitney u test, level of significance set at p<0.05
Wilcoxon paired signed rank test, level of significance set at p<0.05