Medullary Thyroid Carcinoma Presenting with Calcified Thyroid Nodule, Calcified Lung and Cervical Lymph Node Metastasis
Pabbisetty Sushma1, Senthil Kumar Aiyappan2, Sangavi Jeyaraj3, Madhu Sowmitha Pachipala4
1 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRMIST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
2 Professor and Head, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRMIST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
3 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRMIST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
4 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRMIST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Senthil Kumar Aiyappan, Professor and Head, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRMIST, Kattankulathur, Chengalpattu-603211, Tamil Nadu, India.
E-mail: asenthilkumarpgi@gmail.com
Multiple endocrine neoplasia, Nodal metastasis, Thyroidectomy, Thyroid gland
A 64-year-old male patient was admitted to the General Medicine ward for uncontrolled type 2 diabetes mellitus and peripheral vascular disease. On examination, there was presence of neck swelling on the right-side. The swelling was insidious in onset, initially small in size, and slowly progressed to its current size over the past five years. There was no associated pain. There was no history of fever, nausea, vomiting or difficulty in swallowing or breathing. There was also no history of loss of appetite, weight loss, or weight gain. On examination, the swelling moved with deglutition and was noted in the right lower neck in the region of thyroid gland. The approximate size of the swelling was 4×4 cm and the lower border of the swelling was visible. On palpation, the swelling was firm in consistency and partially mobile. There were palpable lymph nodes on the right-side of the neck in level IB and III regions. Clinically, a diagnosis of thyroid carcinoma was kept, in view of palpable lymph nodes. Blood investigations showed a reduced haemoglobin level of 10.4 g/dL. Rest of the investigations, including thyroid function tests were normal.
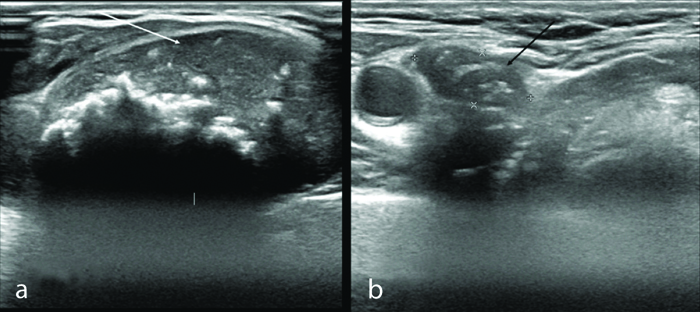
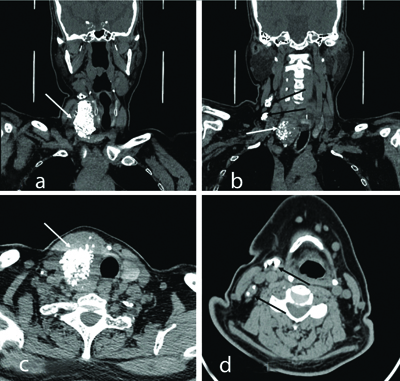
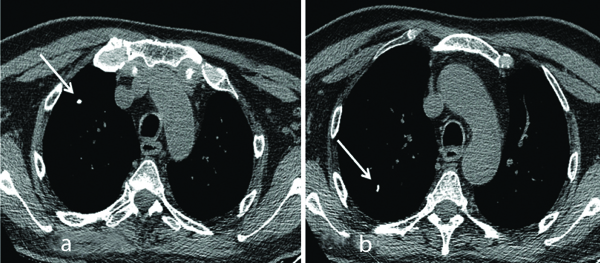
The patient was subjected to ultrasound and Contrast-enhanced Computed Tomography (CECT) of the neck for further evaluation. Ultrasonography (USG) of the neck showed a well-defined wider than taller heterogeneously hypoechoic lesion arising from the right lobe of the thyroid showing dense linear areas of macro calcifications within it [Table/Fig-1a]. On USG, Thyroid Imaging Reporting and Data System (TIRADS) 4 lesion which is moderately suspicious for malignancy was considered. In addition, a few enlarged cervical lymph nodes showing similar calcification were noted in right level IB, II, III, and IV, the largest measuring ~ 1.6×1.0 cm [Table/Fig-1b]. Non contrast and contrast CT of the neck confirmed the above findings with calcified right lobe thyroid lesion and multiple calcified right level IB, II, III, and IV group of lymph nodes [Table/Fig-2a-d]. There was no evidence of retrosternal extension. Chest CT revealed small calcified nodules in the right upper lobe, suggestive of lung metastasis [Table/Fig-3a,b]. The patient was further subjected to Fine Needle Aspiration Cytology (FNAC) of the right lobe of the thyroid lesion which revealed medullary carcinoma. Preoperative serum calcitonin was 309 pg/mL and carcinoembryonic antigen level was 5 ng/mL. The patient underwent total thyroidectomy and right functional neck dissection. Postoperative serum calcitonin was 92 pg/mL indicating improvement. In the present case, the adrenal gland and parathyroid glands were normal, hence this case was sporadic. The patient is presently on follow-up.
a) USG of neck showing a well-defined wider than taller heterogeneously hypoechoic lesion in right lobe of thyroid with dense linear areas of macrocalcifications within it (white arrow); b) USG of neck showing enlarged cervical lymph node with similar calcifications (black arrow).
a-d) Non contrast CT of neck showing calcified right lobe thyroid lesion (white arrows) and multiple calcified cervical lymph nodes on right-side involving level III and IV (black arrows).
a,b) Non contrast mediastinal window CT sections of chest showing calcified nodules in upper lobe of right lung (white arrows)- suggestive of calcified lung metastases.
Medullary Thyroid Carcinoma (MTC) is a rare malignancy of thyroid gland which arises from parafollicular C cells which secrete calcitonin [1]. MTC can be hereditary or sporadic. The hereditary type is usually part of multiple endocrine neoplasm II syndrome [1]. In our case, adrenal and parathyroid glands were normal ruling out Multiple Endocrine Neoplasia II (MEN II) syndrome. All patients with MTC diagnosed with FNAC usually require baseline calcitonin and carcinoembryonic antigen levels. Calcitonin levels greater than 500 pg/mL usually indicate metastatic disease [2]. All patients with MTC should also undergo analysis for Rearranged during Transfection (RET) mutation to diagnose MEN II syndrome [3]. In the present case, the patient could not afford to undergo genetic analysis.
Ultrasonography is the primary modality for the evaluation of thyroid swelling. Currently, Fludeoxyglucose Positron Emission Tomography (FDG PET) is most used. On USG, MTC shares imaging findings of other thyroid carcinomas. It has ill-defined margins, mostly hypoechoic with calcifications. Sometimes it may have a hypoechoic halo like a benign nodule. Lymphadenopathy and extra thyroidal extension usually indicate an advanced stage [3]. On Doppler, it usually shows increased colour flow. USG is also used to evaluate cervical lymph node metastases. The cervical lymph node metastases in MTC is usually seen in medial and infrahyoid compartments [3,4]. But in this case, both supra and infrahyoid compartments were involved. CT and MRI are usually advocated in patients with advanced disease to look for metastases. Most of the time, calcifications are noted both in primary and lymphnodal secondaries like in the present case of MTC. Nuclear Medicine imaging can provide both functional and morphological information especially the hybrid imaging techniques like PET-CT and Positron Emission Tomography-Magnetic Resonance Imaging (PET-MRI) which are useful for staging and restaging of MTC [1,5].
The primary modality of treatment is surgery, which is complete surgical resection of tumour and nodal metastases [2]. In the present case, total thyroidectomy and radical neck dissection was performed. MTC has high mortality rate and shows less favourable prognosis compared to other thyroid carcinomas. Most of the patients usually have lymph node metastases at the time of diagnosis and recurrence can be seen in about 50% of cases [1]. The factors that influence prognosis include baseline calcitonin, Carcinoembryonic Antigen (CEA) levels including their doubling time, genotype, histological findings, metastatic spread, gender, and age [1]. In MTC patients with distant metastases, therapeutic options are limited as they do not concentrate radioiodine and show poor response to chemo and radiotherapy [1]. In the present case, the patient was not willing to undergo chemo and radiotherapy and is currently on follow-up. Postoperative calcitonin levels were reduced in the patient, compared with preoperative values suggesting a response to treatment. Pombo F et al., reported a case of MTC with cervical lymph node metastases which also showed calcifications similar to our case [6]. In a study conducted by Wang L et al., out of 73 patients with MTC, 45 patients (61.6%) showed the presence of calcifications within the thyroid nodules indicating calcifications are common in MTC nodules [7]. In the present case also, there was calcification within the right lobe thyroid nodule which on histopathology turned out to be MTC. Jimenez JM et al., reported a case of MTC with calcified lung metastases, similar to the present case [8]. The other differential diagnosis for calcified lymph nodes includes metastatic adenocarcinoma from breast or lung, metastatic squamous cell carcinoma of head and neck, and treated lymphoma. Benign conditions like tuberculosis, sarcoidosis, amyloidosis and Rosai-Dorfman disease also should be considered as differential diagnosis for calcified cervical lymphadenopathy [9]. To conclude, MTC should be included in the differential diagnosis during evaluation of calcified thyroid nodule and cervical lymph nodes.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 13, 2024
Manual Googling: Jul 03, 2024
iThenticate Software: Jul 04, 2024 (13%)
[1]. Treglia G, Rufini V, Piccardo A, Imperiale A, Update on management of medullary thyroid carcinoma: Focus on nuclear medicineSemin Nucl Med 2023 53(4):481-89.Epub 2023 Jan 2410.1053/j.semnuclmed.2023.01.00336702731 [Google Scholar] [CrossRef] [PubMed]
[2]. Thomas CM, Asa SL, Ezzat S, Sawka AM, Goldstein D, Diagnosis and pathologic characteristics of medullary thyroid carcinoma-review of current guidelinesCurr Oncol 2019 26(5):338-44.Epub 2019 Oct 1. PMCID: PMC682111810.3747/co.26.553931708652 [Google Scholar] [CrossRef] [PubMed]
[3]. Delorme S, Raue F, Medullary thyroid carcinoma: ImagingRecent Results Cancer Res 2015 204:91-116.10.1007/978-3-319-22542-5_426494385 [Google Scholar] [CrossRef] [PubMed]
[4]. Kaliszewski K, Ludwig M, Ludwig B, Mikuła A, Greniuk M, Rudnicki J, Update on the diagnosis and management of medullary thyroid cancer: What has changed in recent years?Cancers (Basel) 2022 14(15):3643PMCID: PMC933280010.3390/cancers1415364335892901 [Google Scholar] [CrossRef] [PubMed]
[5]. Castinetti F, Taïeb D, Positron emission tomography imaging in medullary thyroid carcinoma: Time for reappraisal?Thyroid 2021 31(2):151-55.Epub 2020 Dec 2310.1089/thy.2020.067433191866 [Google Scholar] [CrossRef] [PubMed]
[6]. Pombo F, Rodríguez E, Cao JI, Martínez-Isla C, Cervical lymph node metastases of medullary thyroid carcinoma: CT findingsEur Radiol 1997 7(1):99-101.10.1007/s0033000501189000407 [Google Scholar] [CrossRef] [PubMed]
[7]. Wang L, Kou H, Chen W, Lu M, Zhou L, Zou C, The diagnostic value of ultrasound in medullary thyroid carcinoma: A comparison with computed tomographyTechnol Cancer Res Treat 2020 19:1533033820905832PMCID: PMC701131610.1177/153303382090583232031054 [Google Scholar] [CrossRef] [PubMed]
[8]. Jimenez JM, Casey SO, Citron M, Khan A, Calcified pulmonary metastases from medullary carcinoma of the thyroidComput Med Imaging Graph 1995 19(4):325-28.10.1016/0895-6111(95)00013-58653668 [Google Scholar] [CrossRef] [PubMed]
[9]. Eisenkraft BL, Som PM, The spectrum of benign and malignant etiologies of cervical node calcificationAm J Roentgenol 1999 172(5):1433-37.10.2214/ajr.172.5.1022753310227533 [Google Scholar] [CrossRef] [PubMed]