Metastasis to the brain as a first presentation is very rare and challenging. Metastasis to the brain as a first presentation is very rare and challenging one. Metastatic tumours are ten times more common in brain, than primary intracranial neoplasms. Brain metastasis causes severe neurological morbidity in a patients with cancer. While metastasis to the brain usually occurs late in the course of the disease, but sometimes can be the first clinical presentation of an occult primary tumour. The World Health Organisation (WHO) [1] defines brain metastasis as a tumour that originates outside the CNS and spreads secondarily to the CNS via the haematogenous route or by direct invasion from adjacent tissue [2]. The incidence of CUP in the brain is about 9-17% [2] In adults, the most common sources of brain metastasis are lung cancer, followed by breast cancer, melanoma, Renal Cell Carcinoma (RCC) and colorectal carcinoma.
Metastasis to the brain is more common than other sites due to endogenous microenvironmental niches that favour thriving of metastatic cells [3]. Since the advent of immunohistochemistry in 1941 [4], the ability to discriminate metastatic lesions has gone through a leap into improved accuracy. Histopathology plays a pivotal role in the analysis of metastatic carcinomatous deposits, especially when they present as carcinoma of unknown primary (CUP). Histopathological examination helps determine the nature of the deposits. Immunohistochemical analysis helps in determining the lineage of the metastasised cells and also can help to find the primary cancer [5] at the time of presentation.
Cytokeratin 7 (CK7) and Cytokeratin 20 (CK20) are two individual keratin proteins which have a partially overlapping expressions yet exhibit unique distributions in normal epithelium and corresponding carcinomas. CK7 is a cytoplasmic intermediate filament protein expressed in most ductular and glandular epithelial tissues, including those of the lung, breast, bladder and Female Genital Tract (FGT), but is not found in prostate, hepatocyte, or squamous epithelium [6]. CK7 expression is absent in colon cancer, prostate cancer and squamous carcinoma; this restricted expression makes it a useful marker for identifying the origins of adenocarcinoma when combined with CK20.
The CK20 is an intermediate-sized filament protein found in mature enterocytes and goblet cells, commonly found in the mucosal epithelium of the gastrointestinal tract, especially in the colon. CK20 expression is consistently found in colon carcinoma in combination with negative CK7 expression. The combination of CK7 and CK20 expression in metastatic carcinoma can be useful for determining the origin of the primary tumour [7].
Thyroid Transcription Factor 1 (TTF1) is a nuclear transcription factor belonging to the NKX2 family of homeodomain transcription factors. It promotes embryonic pulmonary and thyroid differentiation and is expressed by most, but not all, lung or thyroid neoplasms.
The present study is presented for its uniqueness and rarity in the presentation of brain carcinoma originating from an unknown primary source.
To analyse the histomorphology and immnuohistochemical patterns obtained using CK7, CK20 and TTF1 in cases presenting with metastatic carcinomatous deposits of unknown primary origin. The present study aimed to provide clinical guidance and suggestions for evaluating metastatic carcinomatous deposits in the CNS with carcinoma of unknown primary (CUP) using antibodies to CK7, CK20 and TTF1.
In institutions with limited availability of immunohistochemistry markers, a basic panel including CK7, CK20 and TTF1 can be helpful in ruling out the common sites of primary tumours that usually metastasise to the brain. Although the application of these markers individually may not be specific, the use of them as a panel has found to be helpful in the search for the primary tumour. This approach not only suggests potential sites for clinicians and also suggesting, the further markers especially in public sector settings where the present study was conducted.
Materials and Methods
This is a cross-sectional study conducted in the Department of Pathology at the Institute of Neurosurgery, Rajiv Gandhi Government General Hospital, Chennai, Tamil Nadu, India, the highest tertiary care referral center in the state, between June 2016 and June 2018. The Institutional Ethical Committee number is 1812017.
Inclusion criteria: Patients who were histopathologically proven cases of metastatic deposits with an unknown primary were included in the study.
Exclusion criteria: Patients presenting with lesions other than metastatic deposits (known primary tumours, melanoma, sarcoma, lymphoma and other non neoplastic conditions) were excluded from the study. Data from autopsy cases were not included in the study.
Out of the 1553 histopathological specimens received, 82 cases were identified as metastatic deposits in the brain, of which 53 cases were deposits from unknown primaries and 29 cases were metastatic carcinomatous deposits from known primary like lung, breast, endometrium and stomach. Among the 53 cases, one case was identified as a melanomatous deposit and 2 were sarcomatous deposits, which were therefore excluded from the study. Rest 50 cases were chosen and subjected to immunohistochemical examination.
Study Procedure
Case details, such as age, sex, presenting complaints, relevant investigations, procedures performed and histopathological diagnosis, were obtained from pathology registers. The squash cytology smears and sections from the paraffin-embedded tissue blocks were reviewed.
After histomorphological analysis, the slides were subjected to Immunohistochemistry (IHC). The markers used were CK7, CK20 and TTF1. IHC was done on three-micron paraffin sections on charged slides, using prediluted antibodies with known positive controls, employing the polymer Horse Radish Peroxidase (HRP) IHC detection system using manufacturer’s instructions. All the markers were from Pathinsitu rabbit monoclonal antibodies (CK7-PRO37, CK20-PRO36, TTF1-PR162). The slides were stained with 3,3′-Diaminobenzidinetetrahydrochloride (DAB) chromogen, counterstained with haematoxylin and subsequently mounted and analysed.
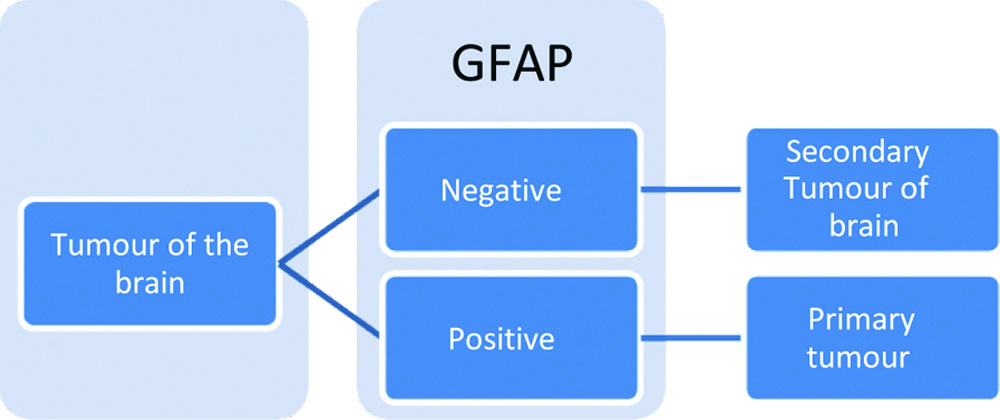
Evaluation of results of immunohistochemical staining: Initial work-up using GFAP was done in all cases and those with GFAP negativity (100%) in the tumour cells were subjected to further marker analysis [8].
The results of IHC for CK7 and CK20 were analysed by a semi-quantitative scoring system. A score ranging from 1 to 4 was assigned: score 4 indicates cytoplasmic staining in >50% of cells; score 3 indicates cytoplasmic staining in 20-50% of cells; score 2 indicates cytoplasmic staining in 5-20% of cells; and score 1 indicates cytoplasmic staining in <5% of cells. For CK7, scores 2, 3 and 4 were considered positive staining, while score 1 was considered negative staining. For CK20, scores 3 and 4 were considered positive, while scores 1 and 2 were considered negative [9]. For TTF1, nuclear positivity in >10% of tumour cells was considered positive and scoring of <10% nuclear staining was considered negative [10].
Statistical Analysis
The results were analysed and presented in tabular form, showing both numbers and percentages. The results were analysed using the IBM Statistical Package for the Social Sciences (SPSS) software version 20.0, using Chi-square test and Fisher’s-exact test.
Results
The incidence of metastatic deposits in the CNS at the study institute was 82 out of 1553 (5.2%). The peak incidence of age at presentation with metastatic carcinomatous deposits in the brain of unknown primary origin was between 5th and 6th decades, accounted for 20 (40%) of cases, with a mean age of presentation of 52.7 years. CUP is more common in males accounting for 30 cases (60%) comparison to 20 cases (40%) of females, resulting in a male-to-female ratio of 1.5:1. Among the 50 cases studied, headache was the most common presenting complaint, accounting for 18 (36%). Solitary lesions were the predominant finding in imaging, observed in about 36 (72%) of cases, with most of these being solid lesions, which accounted for 32 (64%). The imaging studies are tabulated in [Table/Fig-1].
Imaging studies of the lesion.
| Imaging of brain | Frequency | Percentage % |
|---|
| Solid lesions | 32 | 64% |
| Ring enhancing | 7 | 14% |
| Cyst with mural nodule | 1 | 2% |
| Cystic lesion | 4 | 8% |
| Solid and cystic lesions | 6 | 12% |
| Total | 50 | 100% |
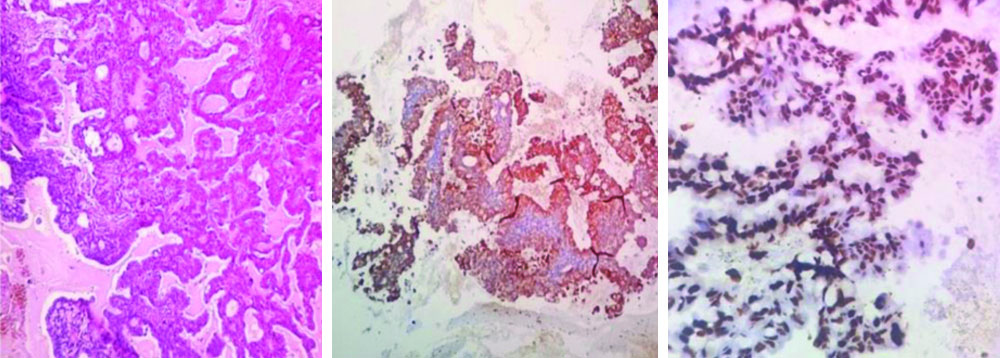
Metastatic carcinomatous deposits in the CNS were more common in the left hemisphere, accounted for 25 (50%), followed by right-sided lesions, which accounting for 18 (36%). Also, frontal lobe was the most favoured site, found in 14 (28%) of cases. A comparison of histomorphology and squash cytology is mentioned in [Table/Fig-2]. Squash cytology done intraoperatively was compared with histomorphology and it was found that the present study was able to detect 41 (82%) of metastatic deposits in squash cytology, which were later confirmed by histopathological examination. In the histopathological examination, adenocarcinoma was the most common morphology observed, accounting for 45 (90%) of cases. In the immunohistochemical analysis of the 50 cases [Table/Fig-3,4], the predominant pattern observed was CK7+CK20-TTF1+, seen in 21 (42%) of cases. The microscopic histology and immunohistochemistry profile of the common CK7+CK20-TTF1+ pattern are shown in [Table/Fig-5]. This immunoprofile was 94.74% sensitive in identifying the primary tumour as lung carcinoma and this combination had a negative predictive value of 96.55% and hence the negative co-expression of CK7 and TTF1 is less likely to indicate a primary lung adenocarcinoma.
Comparison of histomorphology and squash cytology reports.
| Distribution of metastatic carcinomatous deposits based on histomorphology pattern | Corresponding squash reports |
|---|
| Pattern | No. of cases | Metasatic carcinomatous deposit | Others |
|---|
| Adenocarcinoma | 45 | 38 | 7 |
| Squamous cell carcinoma | 2 | 1 | 1 |
| Poorly-differentiated carcinoma | 2 | 1 | 1 |
| Total no. of cases | 50 | 41 | 9 |
Distribution of various patterns of CK7 CK20 and TTF1.
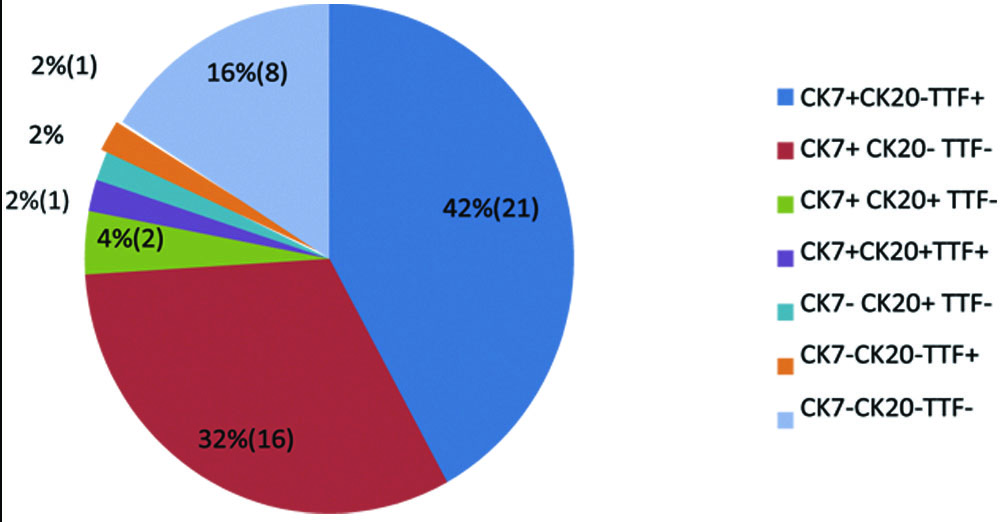
Pattern of staining of CK7 CK20 and TTF1 in metastatic carcinomatous deposits from unknown primary.
| Immunoprofile | Frequency | Percentage |
|---|
| CK7+ CK20- TTF+ | 21 | 42% |
| CK7+ CK20- TTF- | 16 | 32% |
| CK7+ CK20+ TTF- | 2 | 4% |
| CK7+ CK20+ TTF+ | 1 | 2% |
| CK7- CK20+ TTF- | 1 | 2% |
| CK7- CK20- TTF+ | 1 | 2% |
| CK7- CK20- TTF- | 8 | 16% |
| Total | 50 | 100% |
CK7+CK20-TTF1+pattern-adenocarcinoma lung. a) HPE-papillary and acinar pattern of tumour cells (100x); b) IHC-CK7 - cytoplasmic and membranous staining in >50% tumour cells; c) IHC- TTF1 nuclear staining in >10% of tumour cells. (Images from left to right)
In the follow-up of 50 cases of metastatic carcinomatous deposits where the primary was unknown, it was observed that the majority had lung adenocarcinoma as the primary source, accounted for 19 (38%), followed by the gastrointestinal tract at 8 (16%) and the breast at 6 (12%). These findings, along with suggested possible primary sources and further markers, are summarised in [Table/Fig-6]. In 41 (82%) of the cases, the suggested primary correlated with the detected primary when investigated clinically for the unknown primary. Using an initial panel of IHC (CK7, CK20, TTF1) in the search for primary sources in cases of unknown primary metastases to the CNS, the present study demonstrated a sensitivity of 91.67% and an accuracy rate of 90% in revealing the occult primary, which was statistically significant (p=0.014756). CK7+ CK20- TTF1+ was the most common staining pattern found in 21 (42%) of cases, of which 18 cases had lung carcinoma on follow-up. The sensitivity of this pattern in detecting lung carcinoma was 85.7%. Also, there was one case in which lung primary was suggested but no primary was detected; hence the positive predictive value of the test in detecting lung carcinoma was 94.7%, although the specificity was only 50%. The next most common staining pattern was CK+ CK20- TTF1-, which accounted for 16 (32%) of cases. The second most common tumour found to metastasise to the brain with an unknown primary was from the gastrointestinal tract, which showed the above pattern of staining pattern.
Observations, suggestion and follow-up in 50 cases studied and further markers to establish specific diagnosis.
| Immnuoprofile | Distribution | Suggested possible primary | Follow-up details | Suggested further IH C markers |
|---|
| CK7 | CK20 | TTF1 | Total cases (%) | Male n (%) | Female n (%) |
|---|
| Positive | Negative | Positive | 21 (42) | 11 (22) | 10 (20) | 1. Lung2. Thyroid | 18-primary lung adenocarcinoma1-primaryAdenocarcinoma of stomach2- death | 1. Lung - napsin for adenocarcinoma, P63 for squamous cell carcinoma2. Thyroid- thyroglobulin |
| Positive | Negative | Negative | 16 (32) | 10 (20) | 6 (12) | 1. Breast2. Upper GIT3. Sinonasal4. FGT | 6-upper GIT adenocarcinoma2-sinonasal adenocarcinoma1- primary Adenocarcinoma of lung1-death4-breast carcinoma1-ovarian carcinoma1-no primary was found | 1. Breast- GATA, GCDFP2. Upper GIT - CDX23. Sinonasal - PAN CK, EMA4. FGT - WT1, PAX8 |
| Positive | Positive | Negative | 2 (4) | 2 (4) | - | 1. Urinary Bladder2. Hepatobiliary | 1-primary bladder carcinoma1-hepatobiliary carcinoma | 1. Bladder-uroplakin, GATA2. Hepatobiliary -CK19 |
| Positive | Positive | Positive | 1 (2) | - | 1 (2) | 1. Lung2. GIT | 1-lung adenocarcinoma | 1. Lung - Napsin for adenocarcinoma, P63 for squamous cell carcinoma2. GIT - CDX2 |
| Negative | Positive | Negative | 1 (2) | 1 (2) | - | 1. Colon2. Mucinous carcinoma of ovary | 1-rectosigmoid carcinoma | 1. CDX22. Ovary- PAX8 |
| Negative | Negative | Positive | 1 (2) | 1 (2) | - | 1. Thyroid2. Lung | 1-death | 1. Thyroid- thyroglobulin2. Lung - napsin for adenocarcinoma, P63 for squamous cell carcinoma |
| Negative | Negative | Negative | 8 (16) | 6 (12) | 2 (4) | 1. Renal2. Liver3. Prostate carcinoma4. Squamous cell carcinoma | 2- AMA (patient discharged against medical advice)2-death1-had caecal mass1-carcinoma oesophagus1-liver malignancy1-prostatic adenocarcinoma | 1. Renal-RCC, PAX8, CD102. Liver-HEP PAR 13. Prostate- PSA, AMCAR4. Squamous cell carcinoma-P63, CK5/6 |
GCDFP: Gross cystic disease fluid protein; CDX2: Caudal-related homeobox transcription factor 2; PAX8: Paired box gene; AMA: Antimitochondrial antibodies; PAS: Prostate-specific antigen
Discussion
The present study is unique in the government sector, conducted at a tertiary care centre. It aimed to provide clinical guidance as well as suggesting further markers for detecting primary cancer in cases of metastatic carcinomatous deposits with an unknown primary. This approach is designed to be feasible and cost-effective in a resource-limited set-up. By the end of the discussion, the authors have framed an algorithm to address these needs.
Among the 50 cases studied, the peak incidence occurred between the ages of 50 and 60, with a mean age of presentation of 52.5 years. The lesions were more common in males (30 cases) than in females (20 cases), resulting in a male-to-female ratio of 1.5:1. Although bilaterality of metastatic carcinomatous deposits is found to be more common in other studies performed by Saha A et al., which documented that 40.3% of the lesions were bilateral, 34.7% were left-sided and 25% were right-sided [11], the current study found that only 16 (8%) cases presented with bilateral lesions. Additionally, 6 (3%) cases were centrally located, 18 (36%) cases were right-sided and 25 (50%) cases were left-sided lesions as observed in imaging.
Most of the patients presented with headaches 18 (36%) cases as the primary symptom, which is consistent with observations made by Patnayak R et al., and Singh S et al., [12,13]. The squash cytology performed for these cases was compared with histopathological observations, as shown in [Table/Fig-2]. In the current study, squash cytology was able to detected 41 cases of metastatic carcinomatous deposits prior to histopathology, yielding a sensitivity of 82%. Other studies available from Acharya S et al., and Tingner J et al., shows 92.7% sensitivities of 81.81% and 92.7%, respectively [14,15]. The discrepancies in diagnosis can be attributed to sampling errors. The results of immunohistochemistry on the 50 cases using CK7, CK20 and TTF1 [16] showed variety of patterns.
Based on the patterns observed, the authors suggested possible primary sites and conducted a thorough search for the primary tumour. was done and, further markers were also suggested and these patients were subsequently followed-up.
With these observations, the authors arrived at this approach to address metastatic carcinomatous deposits in the brain when the primary site is unknown. The authors also considered which immunochemical markers could be suggested after applying the basic panel of CK7, CK20 and TTF1 to help solve the diagnostic puzzle [17].
The initial work-up for any brain is in [Table/Fig-7]. All cases included in the study were Gliafaserproteins (GFAP) negative. Once the primary brain tumour is ruled out, the initial panel of CK7, CK20 and TTF1 should be applied based on the histopathological pattern and nature of the tumour.
Initial approach to brain tumours.
In the present studies, the authors found that this panel is very useful for the clinical approach and for conducting further marker investigations in the government sector at a feasible cost and the further markers suggested are tabulated in [Table/Fig-4].
As the authors followed-up with 50 cases, the primary site was detected in 41 cases. Six patients died postoperatively, one patient did not have a primary detected and two patients lost to follow-up. Based on the results obtained, a detailed statistical analysis was done statistically.
To conclude, the results indicate that immunohistochemical analysis of CK7, CK20 and TTF1 is valuable for classifying the probable site of the primary, in patients with secondary deposits in the CNS of unknown primary.
In a resource-limited setting, this simple algorithmic approach using histomorphology and IHC (CK7, CK20 and TTF1) can form a baseline for reasonably stratifying the possible sources of the primary and has been found to be statistically significant. In 82% (41) of the cases, the suggested primary correlated with the primary detected during clinical investigation for unknown primary clinically. When utilising an initial panel of IHC (CK7, CK20 and TTF1) in the search for a primary tumour in cases of unknown primary metastases to the CNS, the present study found a sensitivity of 91.67% and an accuracy rate of 90% in revealing the occult primary.
Further studies incorporating organ- or tumour-specific markers will help to clinicians to seek the source of primary malignancy in patients with metastatic carcinomatous deposits in the central nervous system of unknown primary.
Limitation(s)
Though the study helps to search for the hidden primary tumour, it does not pinpoint to as where the primary. To accurately identify the location of the primary tumour, more specific markers for each site need to be further done. But these three markers were selected based on data indicating that adenocarcinoma, especially from the lung, more commonly metastasises to the brain than other types of carcinoma.
Conclusion(s)
The results indicate that immunohistochemical analysis of CK7, CK20 and TTF1 is a useful panel for classifying the probable site of the primary tumour in patients with secondary deposits in the CNS of unknown primary. In a resource-limited set-up, this simple panel (CK7, CK20 and TTF1), along with histomorphology, can form a baseline to reasonably stratify the possible source of the primary tumour. The panel provides a window for the rational use of organ-specific immunohistochemical markers, thereby serving as a cost-effective way of investigation. The authors also found that once the histomorphology indicates carcinomatous deposits and this readily available panel is applied, it hastens the search for the primary. Hence, the present study helps initiation of treatment at the earliest opportunity, especially in public sector hospitals where there is dearth of a wide range of advanced immunohistochemical markers. The present study is feasible and cost-effective compared to other studies that use a battery of antibodies to evaluate CUP. Although the study does not provide a pinpoint diagnosis, it has helped the clinicians in their search for the primary and further management of cases with metastatic carcinoma of unknown origin. It addresses the question of where the probable primary tumour might be in cases where no known primary has been identified.
GCDFP: Gross cystic disease fluid protein; CDX2: Caudal-related homeobox transcription factor 2; PAX8: Paired box gene; AMA: Antimitochondrial antibodies; PAS: Prostate-specific antigen