Refracture at the same site after implant removal is a rare complication, as fractures generally occur close to the plate end due to stress concentration. The reported case involves a patient with refractures of forearm bones at the previous site three months after implant removal. A 48-year-old, right-handed man complained of pain and swelling in his right hand after falling on a wet floor. He had a history of a similar injury three years earlier and was treated with plate osteosynthesis. The plates were removed three months before the present trauma. Radiographs revealed fractures of the distal one-third radius and distal one-fourth of the ulna with evidence of previous screw holes. He has been treated with a Low-contact Dynamic Compression Plate (LCDCP) and remains under follow-up. Refracture three months after implant removal at the site of the previous fracture site in both bones is a very rare occurrence and the present case report highlighted the importance of making a proper decision regarding union, when considering implant removal and post-implant removal care.
Fracture, Plate osteosynthesis, Radius, Stress concentration
Case Report
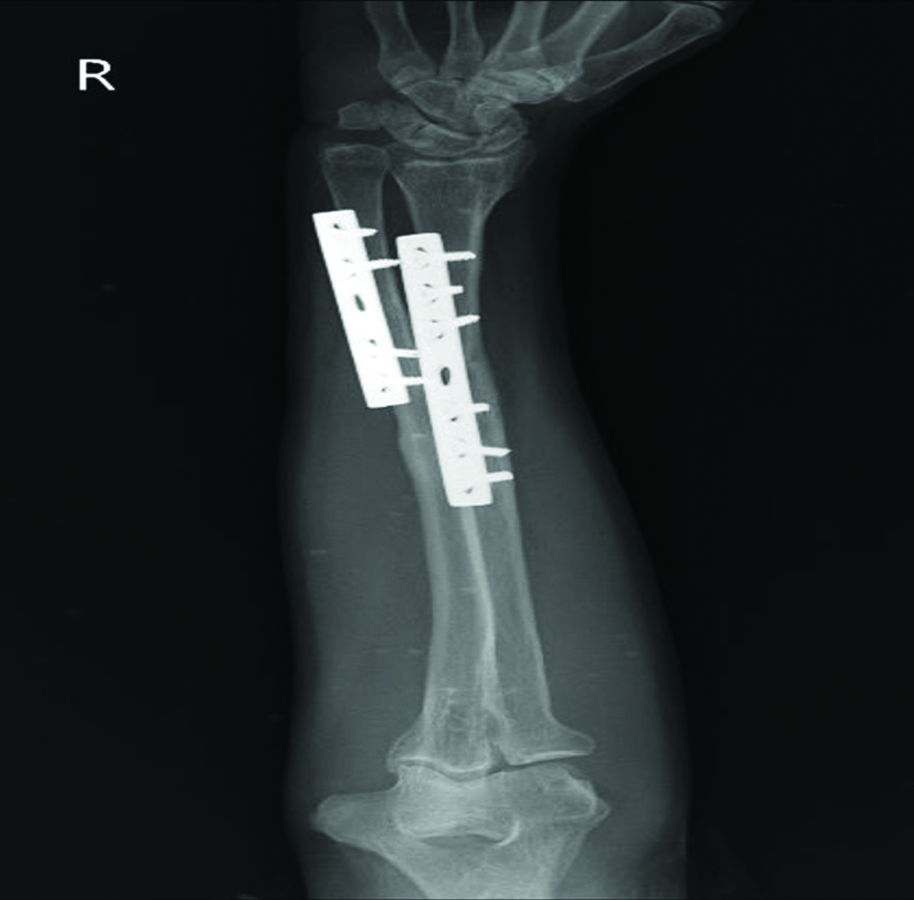
A 48-year-old, right-handed dominant male presented to a tertiary health facility in central India with chief complaints of pain and swelling in the lower part of his right forearm for 10 days following a fall on the forearm with a palmar flexed wrist. The patient was unmarried and worked as a priest in a village temple. He did not have any habits or addictions. There was no significant medical history. The pain was severe in degree, sharp in nature, localised and did not radiate. It was associated with diffuse swelling and localised deformity in the lower half of the forearm. Swelling gradually progressed to the wrist and palm. The patient reported a similar fall three years back, resulting in a fracture in the forearm bones. The fracture was treated with open reduction and plate osteosynthesis. After the treatment, the patient resumed normal activities for two and half years. The plates in the forearm bones were removed through elective surgery three months before the current trauma. The forearm was supported by an above-elbow slab for three weeks after the implant removal. The X-ray taken immediately after the implant removal showed six screw holes in the radius and four screw holes in the ulna, with a united fracture site in both bones [Table/Fig-1]. The fracture site in the radius exhibited a faint gap despite consolidation across the cortices, indicating incomplete remodelling of the fracture. There was evidence of new bone formation in the mid ulna near the expected proximal tip of the plate used for fixation of the fracture.
X-ray immediately after implant removal showing screw holes.

Upon examination, an obvious deformity was noted in the right forearm along with mild diffuse swelling. On palpation, the local temperature was normal, and bony tenderness was present in the distal 1/3rd of the radius and ulna. Crepitus was appreciated upon palpating the ulna and radius, and abnormal mobility could be demonstrated. Bony irregularity was noted in the lower 1/3rd of the radius and ulna. There was no neurovascular deficit in the upper limb. The fresh anteroposterior and lateral view X-ray of the forearm revealed a displaced transverse fracture of the lower 1/3rd radius and lower 1/4th ulna [Table/Fig-2]. The shafts of the bones showed evidence of disappearing holes in both proximal and distal fragments. The relationship between the ulnar and radial styloid processes was disturbed, indicating inferior radioulnar joint subluxation. The fracture margins were not sharp, suggesting the possibility of a refracture of the radius and ulna at the site of the previous fracture caused by a similar mode of trauma.
Anteroposterior and lateral view X-ray showing displaced fracture in the distal one-third radius and lower fourth ulna with evidence of old screw holes.

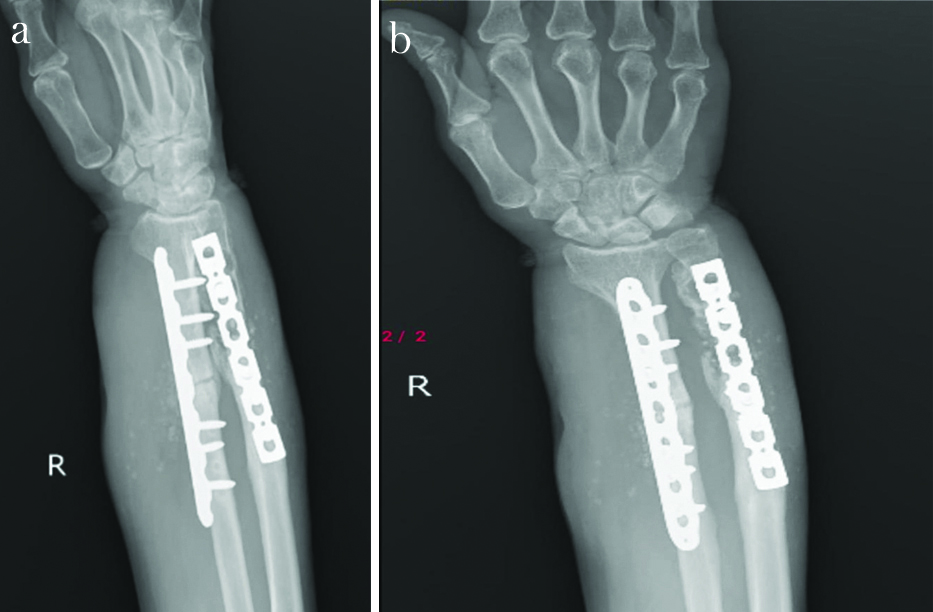
The patient underwent treatment with open reduction and internal fixation under brachial block anaesthesia. The radius and ulna were fixed with a LCDCP. Follow-up X-rays indicated an acceptable position and stable fixation of both bones in the proximal and distal fragments. The radius fracture was stabilised with a 7-hole plate and six cortical screws, three in each of the proximal and distal fragments. The ulna fracture was stabilised with a 5-hole plate and two screws in each fragment [Table/Fig-3]. The inferior radioulnar relationship improved after the fixation.
X-ray showing the fixation of radius and ulna with LCDC plate.
The postoperative wound was inspected on the fourth day, and the stitches were removed on the tenth day. The patient was discharged and was advised to take 1000 mg of calcium and 500 mg of vitamin C daily for six weeks, along with wrist and elbow mobilisation instructions. By the 4-month follow-up, the patient had full function of the elbow, wrist and forearm. However, in the sixth month, the patient developed diffuse swelling in the lower half of the forearm [Table/Fig-4a,b].
a,b) Clinical photograph after 4 months follow-up showing diffused swelling in lower half of forearm.

Fresh X-rays showed properly fixed plate and uniting fracture of radius with lysis around holes in ulna [Table/Fig-5a,b].
a,b) Oblique view X-ray of forearm after 4 month follow-up; b) AP view X-ray of forearm after 4 month follow-up.
Discussion
Forearm fractures are common fractures in all age groups [1]. The annual incidence of midshaft fractures of both bones of the forearm is around 10 per 10,000 individuals [1]. Forearm fractures are commonly caused by falls on outstretched hands, direct hits to the forearm, falls from heights, road traffic accidents and sports-related injuries. A direct strike to the forearm is the most frequent cause, typically resulting in a fracture of the radius, ulna, or both [2].
The present case has shown promising outcomes with compression plating for transverse fractures of the lower third of the radius and the lower fourth of the ulna, similar to a case reported by Dankwa KNA et al., [2]. In their case, a 40-year-old motorcyclist suffered a left midshaft radius and ulna fracture in a road accident and was treated under general anaesthesia by open reduction and internal fixation using plates and screws for all four fractures. A gradual recovery was made in six months with a complete range of movements. Another case by Bai X et al., involved a 29-year-old male patient who suffered a forearm fracture while riding a bicycle [3]. X-ray scans revealed both bone forearm fractures classified as 2R2A2 and 2U2A2 fractures based on Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification. The patient was treated with open reduction and internal fixation.
Furthermore, Open Reduction Internal Fixation (ORIF) using plates and screws is the current gold standard for surgical treatment. Using intramedullary fixation plates for internal fixation is an alternate strategy [4]. Surgical treatments such as intramedullary nailing are also preferred [1,5]. Current literature concludes that the plating method leads to better recovery rates, a complete range of movement, and alignment with the least reported complications [6,7].
Different surgical modalities for transverse fractures in the radius and ulna are available, including plating and intramedullary nailing [5]. Al-Sadek TA et al., reported the functional outcome using Anderson’s scoring method, which was 87% for the plating group and 68% for the nailing group [6]. In the plating group, there was 100% union, while in the nailing group, it was 86%. Delayed or non union outcomes were found in 9% of the nailing group compared to 0% in the plating group. The average period of union was 9.4 weeks in the plating group and 10.2 weeks in the nailing group [6]. Raghute S and Maheshgauri D discussed four distinct treatment approaches including the hybrid technique of ulna nailing and radius plating, ulna plating and radius nailing, both ulna and radius nailing, and both ulna and radius plating [5]. Most cases resulted in excellent to good functional outcomes in both bone plating groups (100%), followed by hybrid techniques of radius plating and ulnar nailing (83.3%), ulnar plating and radius nailing (75%) and lastly, both bone nailing groups (66.7%). Malunion was observed in one instance of radius plating and ulnar nailing, and in two cases of both bone nailing and ulnar plating and radius nailing. The incidence of complications was highest in both bone nailing groups (33.3%), followed by hybrid techniques, i.e., ulnar plating and radius nailing (25%), and radius plating and ulnar nailing (16.7%), with both bone plating showing no complications. This concludes that the technique utilising both bone plating, namely ulna and radius plate fixation, had the most significant functional recovery results, the lowest rate of complications, and good biomechanics among the four distinct fixation techniques used to treat adult diaphyseal forearm fractures [5].
Stress concentration after implant removal in the vicinity of the plate’s limit can cause limb fractures [8]. Refracture in the forearm after implant removal in the area adjacent to the plate’s limit has been described due to stress concentration. A microfracture close to a screw hole might result from removing the cortical screw [9]. This generally occurs within three months of implant removal [10]. Orthopaedic surgeons should take caution to prevent locally concentrated stress, also referred to as ‘point loading’, ‘edge loading’, ‘line loading’, etc., that can occur when the bone comes into contact with implant points. This is particularly crucial when prosthetics or nails are implanted [11].
The present case is reported for the uncommon features of a fracture recurring at the previous site in the same forearm bones due to a similar pattern of trauma three months after elective implant removal. There is a possibility of incomplete remodelling of the fracture site after the previous surgery, due to which the bone might not have obtained normal strength. The second trauma might have concentrated the forces in such a way that the bone fractured again at the site of the first fracture. This highlights the need for proper clinical and radiological assessment of fracture union after internal fixation with plates. One must ensure visible secondary callus formation at the fracture site for union and continuity of cortices for remodelling and consolidation. After implant removal, the part should be immobilised for a few weeks to avoid fractures at the ends of the plate due to stress concentration.
The first fixation done for the fracture was satisfactory, but the decision to remove the plate might have been postponed to avoid refracture, as the union quality was probably not strong. Implants like plates that are not causing any symptoms may not be removed in many cases.
Conclusion(s)
In cases of stable plate osteosynthesis, union should be confirmed by secondary callus at the fracture site radiologically. During fixation, the terminal holes in the fixing plate may engage only one cortex to avoid stress concentration at the ends of the plate. The decision to remove the plate should be taken after confirming strong union of the fracture followed by satisfactory remodelling and consolidation. After implant removal, it is advisable to immobilise the part for a few weeks and keep the patient under follow-up to diagnose any unwanted complications of a fracture at the same site or at the site of the plate end.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 24, 2024
Manual Googling: Apr 15, 2024
iThenticate Software: Jun 13, 2024 (11%)
[1]. Saini R, Sharma A, Baisoya K, Ravalji D, A comparative study between plate osteosynthesis and intramedullary nailing for diaphyseal fracture of radius and ulna in adultsCureus 2023 15(4):e37277 [Google Scholar]
[2]. Dankwa KNA, Kuuzie E, Ofori SK, Rare bilateral radius and ulna fractures: A case reportOpen J Orthop 2024 14(1):01-11. [Google Scholar]
[3]. Bai X, Liu Z, Chen W, Wang B, Hybrid fixation with ESIN for both bone forearm fractures in adults: A case report and literature reviewFront Surg 2022 9:949727Available from: https://www.frontiersin.org/articles/10.3389/fsurg.2022.949727 [Google Scholar]
[4]. Hoogervorst P, van Dam T, Verdonschot N, Hannink G, Functional outcomes and complications of intramedullary fixation devices for Midshaft clavicle fractures: A systematic review and meta-analysisBMC Musculoskelet Disord 2020 21(1):395 [Google Scholar]
[5]. Raghute S, Maheshgauri D, Evaluation of functional and radiological outcomes of adult diaphyseal fractures of both bone of forearm operated with plating or nailingGlob J Res Anal 2022 :160-64. [Google Scholar]
[6]. Al-Sadek TA, Niklev D, Al-Sadek A, Diaphyseal fractures of the forearm in adults, plating or intramedullary nailing is a better option for the treatment?Open Access Maced J Med Sci 2016 4(4):670-73. [Google Scholar]
[7]. Garg A, Sharma R, Jain M, Yadav U, Nemani M, Singh A, Compression plating for diaphyseal forearm fractures and evaluation of functional outcomesInt J Orthop Sci 2019 5(4):1010-12. [Google Scholar]
[8]. Zhu Y, Hu J, Zhan T, Zhu K, Zhang C, Refracture after plate removal of midshaft clavicle fractures after bone union-incidence, risk factors, management and outcomesBMC Musculoskelet Disord 2023 24(1):308 [Google Scholar]
[9]. Tsai SW, Ma HH, Hsu FW, Chou TFA, Chen KH, Chiang CC, Risk factors for refracture after plate removal for midshaft clavicle fracture after bone unionJ Orthop Surg Res 2019 14(1):457 [Google Scholar]
[10]. Anantavorasakul N, Lans J, Wolvetang NHA, Walbeehm ET, Chen NC, Forearm plate fixation: Should plates be removed?Arch Bone Jt Surg 2022 10(2):153-59. [Google Scholar]
[11]. Yoo J, Ma X, Lee J, Hwang J, Research update on stress riser fracturesIndian J Orthop 2020 55(3):560-70. [Google Scholar]