Open fractures of tibia are a common occurrence following high energy trauma owing to its subcutaneous location with relative high frequency of soft tissue injuries, and have high rate of non union and malunion due to precarious blood supply [1]. Complications include joint stiffness, ankylosis, arthrodesis, malunion, skin and bone infections, amputation and even death [2,3]. The recommended treatment options for open fractures of the proximal tibia are open reduction and internal fixation with plate and screws, conservative management and external fixation of the fracture fragments. However, all of these complications are exacerbated if open reduction methods are employed [4,5].
The goals to achieve in complex proximal tibial fractures are infection prevention, maintenance of normal length, alignment and rotation of the extremity; minimising additional damage to soft tissue and bone and therefore preserving the remaining circulation and providing a mechanical environment which stimulates periosteal and endosteal responses favouring bone healing [6-8]. These goals are more or less achieved with ilizarov fixation as being a closed process it avoids any additional vascular and soft tissue trauma and bone devitalisation to already compromised tissue, thereby diminishing infection rate, and stimulates bone growth by ligamentotaxis principle [9]. Its biggest advantage lies in the fact that as an definitive intervention, it can be used irrespective of the skin condition (fracture blisters or extensive subcutaneous haemorrhage and bruising) [10]. Once the alignment of limb is achieved, immediate postoperative mobilisation of knee and weight bearing ambulation can be started as this system is very stable and rigid along with providing rotational and angular stability [11,12]. Maintenance of the mechanical axis can be continually monitored by adjustment of the frame. Multiple studies across the world have shown lesser incidence of infections (0-6%) and high union rate (96-100%) in cases treated with ilizarov external fixation when compared with open reduction and internal fixation [9,13-16].
At our hospital open reduction and fixation methods were routinely employed for management of complex proximal tibial fractures and ilizarov external fixation was only recently introduced by one of our surgeons for management of these types of fractures. This study was undertaken to know whether ilizarov external fixation with or without minimal internal fixation as an initial and definitive mode of fracture fixation for high energy tibia fractures with compromised skin condition can provide satisfactory outcome with few complications.
Materials and Methods
This prospective clinical interventional study was undertaken after approval of the Institutional Ethics Committee (order no: SNMC/IEC/2019/536-538) for cases of complex proximal tibial fractures with compromised skin treated with ilizarov external fixation with or without minimal internal fixation between June 2018 to October 2020 at a single tertiary level government hospital associated with Dr S N Medical College, Jodhpur in western Rajasthan, India.
Inclusion criteria: Skeletally mature patients of less than 70 years, with proximal tibia fracture with compromised skin condition (blister on skin, extensive subcutaneous haemorrhage, bruise or open fractures) and severely comminuted compound proximal tibia fractures were included in the study.
Exclusion criteria: Patients with close proximal tibia fracture with good skin condition, associated neurovascular injuries, presence of other fractures or systemic injuries, or who underwent damage control measures like fasciotomy or temporary spanning external fixation, and with fixation modalities other than ilizarov were excluded.
Sample size calculation: Sample size was calculated on the basis of previous study by Ramos T et al., [9]. Sample size was calculated at 95% confidence interval to verify an expected 83% favourable outcome of ilizarov technique among proximal tibial fracture patients at an allowable error of 20% and was found to be of minimum 21 subjects. Considering 20% drop out due to long follow-up, it was enhanced and rounded off to 30 subjects.
Study Procedure
Informed consent was taken from all patients. A Case Record Form (CRF) was specially designed by principal invigilator and guide [Annexure-1] before approval of study plan and was filled while admitting the patient which included demographics, history of illness, staging of fracture (Tscherne’s classification [17] for closed fractures and Gustilo Anderson’s classification [18,19] for open fractures) and detailed clinical examination along with relevant investigations like complete haemogram, routine urine examination, coagulation profile, liver and renal function test, electrocardiogram and chest X-ray. Also, blood grouping and cross matching were carried out if found necessary.
Preoperative radiographs were taken for all cases. Computed Tomography (CT) scan of the affected area was taken in 10 cases as they were taken only for complex fractures. These cases were clinically and radiologically evaluated and interdepartmental references were taken when found necessary to make the patient fit for surgery. All patients underwent ilizarov apparatus application [Table/Fig-1].
Postoperatively, all the cases were followed-up until fracture union occurred for a minimum period of 6-12 months. Results were analysed both clinically and radiologically using Johner and Wruh’s criteria [Table/Fig-2] [4].
Clinical and radiological outcomes of patients as assessed by Johner and Wruh’s criteria [4].
| Variables | Excellent (N) | Good (N) | Fair (N) | Poor (N) |
|---|
| Neurovascular injuries | None (30) | Minimal (0) | Moderate (0) | Severe (0) |
| Deformities |
| Varus/valgus | None (30) | 2-5 (0) | 6-10 (0) | >10 (0) |
| Pro-recurvatum | 0-5 (28) | 6-10 (2) | 11-20 (0) | >20 (0) |
| Rotation | 0-5 (30) | 6-10 (0) | 11-20 (0) | >20 (0) |
| Shortening | 0-5 mm (28) | 6-10 mm (0) | 11-20 mm (2) | >20 mm (0) |
| Mobility |
| Knee | Full (25) | >80% (4) | >75% (1) | <75% (0) |
| Ankle | Full (29) | >75% (1) | <75% (0) | <50% (0) |
| Subtalar | Full (30) | >75% (0) | <75%(0) | <50% (0) |
| Pain | None (29) | Mild (1) | Moderate (0) | Severe (0) |
| Gait | Normal (29) | Normal (0) | Mild limp (1) | Significant limp (0) |
| Strenuous activities | Possible (29) | Limited (1) | Severely limited (0) | Impossible (0) |
In number of patients having that outcome are given
All subjects with open fracture were started on triple antibiotics which includes 3rd generation cephalosporins, metronidazole for anaerobic bacteria and aminoglycoside for gram negative bacterial coverage for three days. Immediate and thorough wound irrigation with normal saline in the emergency department itself was done for all open fractures. Meticulous debridement of any obvious devitalised tissue was undertaken in operating room and primary wound closure with tension free sutures was done. Patients who required plastic surgery interventions were operated in the same sitting with plastic surgery procedures like flap coverage and Split Skin Grafting (SSG), if the wound was healthy.
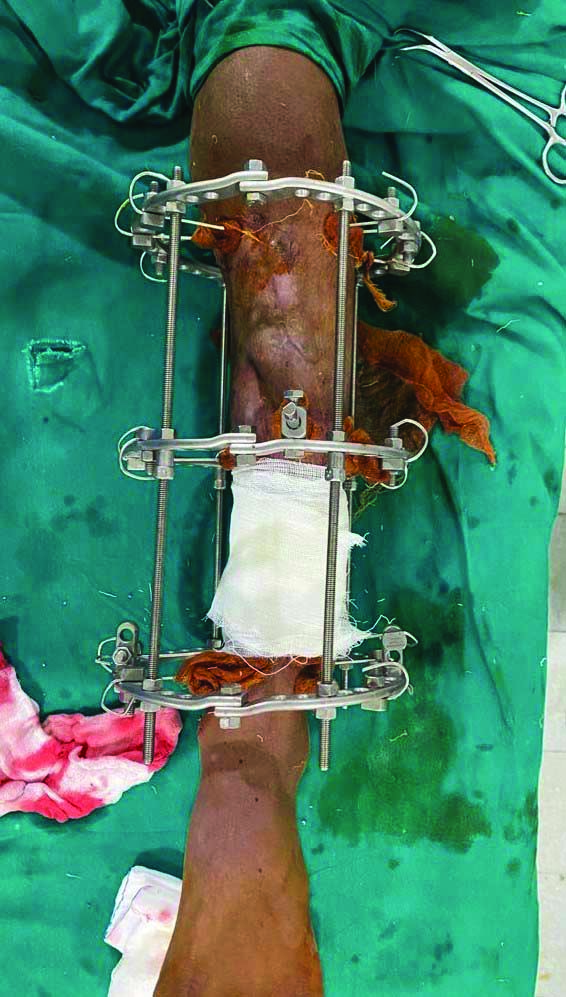
After proper preoperative anaesthetic evaluation, the surgery was performed under spinal anaesthesia. All patients underwent a standard ilizarov operative procedure without a tourniquet on operation theatre table [Table/Fig-1]. Axial reduction, pin insertion and assembly of the frame was done under biplanar C arm guidance. Assembly of the frame, consisting of three appropriately sized rings connected by threaded rods was done on table. The proximal ring was placed at the juxta-articular region of tibia, with second and third rings at just distal to any shaft fracture component and supramalleolar region of tibia, respectively were placed. The proximal most and the distal most rings were placed around 2 cm away from the respective joint line. For additional stability two or more 2 mm wires were secured and tensioned parallel to the articular surface depending on the fracture fragments. All rings were then connected with connecting rods restoring the mechanical axis. A 5% w/v povidone iodine-soaked gauze pieces were applied on pin tracts.
Postoperative care: Postoperatively, physiotherapy was started immediately within 24 hours of procedure in the form of quadriceps strengthening and hip, knee and ankle range of motion exercises. All patients were encouraged to full, unrestricted weight bearing with the help of an adjustable walker immediately after surgery as much as their tolerance level and fixator allowed [Table/Fig-3]. Postoperative radiographs were taken on the next day after ilizarov fixation. Once, patients were able to walk using adjustable walker and independently climb stairs, they were discharged directly to their homes.
Postoperation mobilisation and weight bearing with ring in situ.

First follow-up was done after two weeks of discharge after ilizarov fixation and thereafter at four, eight and 12 weeks, following which the frequency was decreased to once in six weeks till radiographic union was achieved. Serial radiographs were taken at all follow-up. At each follow-up, wires were checked for loosening or infection, knee and ankle mobilisation were assessed. Patients were demonstrated pin tract care at each visit to the Outpatient Department (OPD). Radiological evaluation was done at each monthly visit. The patients were assessed clinically and radiologically for pain and functional limitations. Patients were examined for any malalignment, range of motion and bony union. Following complications like pin tract infection, deformity, stiffness, re fractures, non union, deep vein thrombosis and osteomyelitis were also assessed.
As described by Ramos T et al., clinical and radiological assessment was done before implant removal was planned [9]. Once union was achieved, implant was removed under spinal anaesthesia.
Radiological criterion: During follow-up, radiographs of the affected limb were taken in anteroposterior view and lateral view. The fractures were considered to be united when anteroposterior and lateral radiographs show bridging callus in three of the four cortices [9].
Functional criterion: Fracture union was considered when it was stable when stressed manually and the patients were able to walk after removal of the connecting rods. Fixator was then removed under local anaesthesia. Patient’s leg length was measured clinically to assess limb length discrepancy. Varus and valgus angulation were assessed by full length X-ray of tibia in anteroposterior view, procurvatum and recurvatum deformity were assessed by full length X-ray of tibia in lateral view. Postoperative rotational deformities were assessed clinically.
Movements at knee, ankle and subtalar joint were assessed clinically and compared to normal range of motion. Pain and strenuous activities of patient were assessed and used in Johner and Wruh’s criteria, which was used for final evaluation of the patients [4].
Statistical analysis
Descriptive statistical analysis was carried out in the present study with Statistical Package for the Social Sciences (SPSS) 15.0 software. All continuous variables were presented as mean±Standard Deviation (SD). Categorical measurements were described in number, proportion and percentage. Further statistical comparisons between the open and closed fracture groups were not done as the number of patients was small and unequal in both groups.
Results
This was a prospective interventional study consisting of 30 patients who underwent ilizarov apparatus application with no sample loss in follow-up. Their demographic data and baseline information is given in [Table/Fig-4]. There were 23 closed fractures with compromised skin condition and seven open fractures [Table/Fig-5]. Among these 30 patients, all cases had three rings. There were two patients who underwent secondary procedures as split skin graft. Fracture union was achieved in all cases with a maximum period of 22 weeks on fixator and minimum being 12 weeks. Average time for fracture union was 15.26 weeks and number of days on fixator was 105 [Table/Fig-6].
Patient demographics and baseline data.
| Parameter | Number (%) |
|---|
| Age (years) (Mean±SD) | 39.66±11.32 |
| Gender |
| Male | 24 (80) |
| Female | 6 (20) |
| Laterality |
| Right | 19 (63.33) |
| Left | 11 (36.67) |
| Mode of injury |
| Road traffic accident | 26 (86.66) |
| Fall from height | 2 (6.67) |
| Assault | 2 (6.67) |
| Co-morbidity |
| Hypertension | 4 (13.33) |
| Diabetes mellitus | 1 (3.33) |
Distribution of patients according to injury.
| Type of tibial fracture | No. of patients | Total patients |
|---|
| Close fracture (Tscherne’s classification) [17] | 0 | | 23 (76.67%) |
| 1 | 10 (43.48%) |
| 2 | 13 (56.52%) |
| 3 | |
| Open fracture (Gustilo Anderson’s classification) [18,19] | I | 2 (28.57%) | 7 (23.33%) |
| II | 2 (28.57%) |
| III A | 1 (14.29%) |
| III B | 2 (28.57%) |
| III C | |
Number of weeks of fixator.
| Number of weeks of fixator | Close fracture cases, n=23 (%) | Open fracture cases, n=7 (%) | Total cases, n=30 (%) |
|---|
| 12-14 | 10 (43.48) | 4 (57.14) | 14 (46.67) |
| 15-17 | 9 (39.13) | 0 | 9 (30.00) |
| 18-20 | 4 (17.39) | 2 (28.57) | 6 (20.00) |
| ≡21 | 0 | 1 (14.29) | 1 (3.33) |
At the final follow-up average range of motion of knee was 115.52±13.32° with all patients having more than 90° of knee flexion [Table/Fig-7]. Seven patients had loss of extension with one having up to 15° losses of extension remaining six patients had extension deficit up to 10°.
Range of motion of knee at final follow-up.
| Variables | Closed fracture cases, (n=23) | Open fracture cases, (n=7) | Total fracture cases, (n=30) |
|---|
| Knee range of motion (flexion) | 114.35±14.7° | 118.57±6.90° | 115.52±13.32° |
| Extension lag | 6 (26.09%) | 1 (14.28%) | 7 (23.33%) |
In present study, pin tract infection was observed in 6 (20%) patients, knee stiffness in 3 (10%) patients and limb shortening in 2 (6.67%) patients of 1.2 and 1.5 cm.
Radiological and functional outcome parameters as assessed by Johner and Wruh’s criteria are given in [Table/Fig-2]. By using these criteria, we excellent results were obtained in 23 (76.66%), good in 5 (16.67%) and fair in 2 (6.67%) patients [Table/Fig-8]. In this study, no one reported poor outcome. The [Table/Fig-9,10] shows the radiological and functional outcome in a 30 year male patient who reported excellent result in present study.
Results according to Johner and Wruh’s criteria in relation of fracture type.
| Johner and Wruh’s criteria | Closed cases n=23 (%) | Open cases n=7 (%) | Total cases n=30 (%) |
|---|
| Poor | 0 | 0 | 0 |
| Fair | 0 | 2 (28.57) | 2 (6.67) |
| Good | 1 (4.35) | 4 (57.14) | 5 (16.67) |
| Excellent | 22 (95.65) | 1 (14.28) | 23 (76.66) |
Radiological outcome of 30-year-old male patient with fracture of left tibia. a,b) Preoperative anteroposterior and lateral radiograph; c,d) Immediate postoperative anteroposterior and lateral radiograph; e) Three months after Ilizarov fixation anteroposterior radiograph; f) After removal in follow-up radiograph.
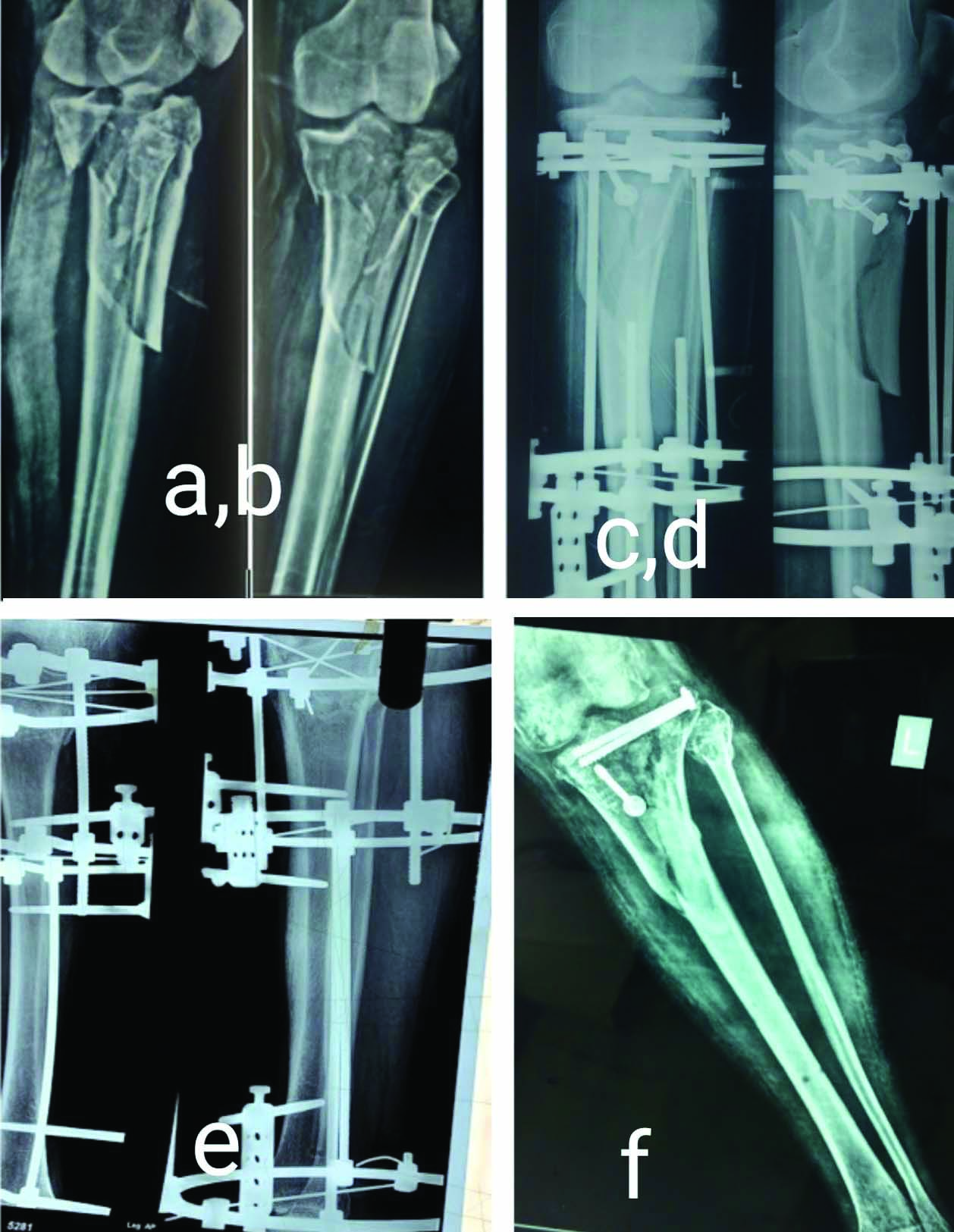
Limb alignment and functional outcome at final follow-up.

Discussion
High energy fractures of tibia are very common and are associated with complex osseus and soft tissue injuries [1,20]. The degree of resulting comminution, soft tissue injury, displacement and the mechanism of injury determines their outcome, treatment and prognosis [4,21]. Tibia being subcutaneous, these fractures are open fractures most of the time with bone loss [1].
Ilizarov apparatus is a unique and versatile fixation system that permits functional axial loading of the injured limb and simultaneously allows early weight bearing unlike any other treatment by internal fixation. This system allows for adjustment of the alignment, compression and distraction both during surgery and at subsequent follow-ups without further surgical intervention on an already compromised tissue [9].
A number of studies from literature using Ilizarov fixation for proximal tibia fractures had reported the clinical success and low morbidity associated with its use for external fixation and minimal internal fixation. Results and clinicoradiological outcome of these studies are compared with present study in [Table/Fig-11] [9,10,13-15,22-25].
Comparison of studies on outcome and complications of Ilizarov fixation in proximal tibia fractures available in the literature with present study [9,10,13-15, 22-25].
| Author’s name and year | Sample size (Close/open fractures) | Average time for fracture union | Union rate | Results | Complications | Conclusion |
|---|
| Present study (2021) | 30 (23/7) | 15.26 weeks | 100% | Excellent/good/fair: (23/5/2)knee ROM: 115.52o | Pin tract infection: 6Knee stiffness:3Limb shortening:2Extension lag: 7 | Safe and effective method in cases of compromised skin. |
| Subramanyam KN et al., (2019) [10] | 30 (27/3) | 11.8 weeks | 100% | Excellent/good/fair/poor: 16/8/5/1 Knee ROM: 114.7o mean AKSS 81.5 mean RRS 16.7 | Pin tract infections: 7 Common peroneal neuropathy: 2 | Acceptable outcome for complex tibial plateau fractures. Minor loss of alignment, especially in Type VI Schatzker fractures after removal of the fixator. |
| Kartheek R and Kodandapani K, (2017) [22] | 15 | | | Good to excellent/ fair: 14/1Knee ROM: 124.6° | Pin tract infection: 2Deep infection: 1Arthritis: 3Equinus deformity: 1 | Decreased hospital stay, decreased waiting time for definitive surgery and early weight bearing |
| Sheshagiri V et al., (2016) [23] | 20 | | | Excellent/good/fair/poor (functional result): 11/8/1 | Pin tract infections: 3early implant removal due to non compliance | Early weight bearing and minimal soft tissue compromise |
| Ramos T et al., (2013) [9] | 30 | | 100% | Satisfactory result in 27 patients Knee ROM >10-1000 in 25 patients | Pin tract infection: 2Compartment syndrome: 2Deep venous thrombosis: 1 | Good clinical outcome and is a valuable alternative in proximal tibial fractures of all types |
| Mohamed OA and Youssef SA, (2013) [24] | 30 | 14.4 weeks | 100% | Excellent/good/fair/poor: 10/10/5/5 | | Recommended when extensive dissection and internal fixation are contraindicated due to fracture comminution and soft tissue compromise |
| Catagni M A et al., (2007) [13] | 59 (54/5) | 16.42 weeks | | Excellent/good/fair/poor: 30/27/1/1 | Deep venous thrombosis: 2Commom peroneal nerve palsy: 2 | Excellent to good results in most cases of complex tibial plateau fractures |
| Barbary HEl et al., (2005) [14] | 29 | 16.3 weeks | 100% | Excellent/good/fair/poor: (18/7/1/2) Median knee ROM: 0-1120 | Minor pin tract infection | High clinical success and low morbidity |
| Dendrinos GK et al., (1996) [15] | 24 | 14.4 weeks | 100% | | Deep venous thrombosis: 8Compartment syndrome: 3Delayed union: 1 | Very good modality of treatment in soft tissue damage and bony comminution |
| Zecher SB et al., (1996) [25] | 21 | | | Knee ROM >900 in all patients | Compartment syndrome: 7 | Much-needed tool in the treatment of high-energy tibial plateau fractures associated soft-tissue injuries |
ROM: Range of motion
All fractures were united with average time for fracture union of 15.26 week (range 12-22 weeks) in present study. Similar studies using ilizarov fixation had reported very high union rate with mean time to fracture union between 11-16 weeks [Table/Fig-9]. A high union rate with minimal mal union and non union of these fractures treated by ilizarov fixation can be attributed to the fact that ilizarov fixation induces axial micromotion at the fracture site and thus accelerates fracture healing. Ilizarov apparatus allows close reduction, provides 360° stability, and with minimal softtissue exposure, there is little interference to the periosteal and endosteal blood supply of fractured bone [26-28]. It has an added advantage of possibility to improve reduction and alignment while on fixator, thus diminishing chances of malunion and nonunion. It allows early joint mobilisation and early weight bearing which stimulates bone angiogenesis and promotes osteogenesis, leading to quicker re-modelling [26,29,30].
Average range of motion of knee was 115° with extension deficit up to 15° in seven patients in present study. No cases with significant deformities in sagittal or coronal plane and no rotational deformities were noted in present study. Similar results had been reported in literature in studies using ilizarov fixation for proximal tibia [Table/Fig-11]. Early definitive intervention, closed procedure and no need for staged surgeries avoiding further soft tissue trauma, immediate weight bearing and limb physiotherapy in postoperative period are possible reasons behind good knee and ankle functions [26]. Further no femoral ring was used in any of the patients, thus facilitating immediate knee physiotherapy.
Similar to other studies most common complication observed was the pin tract infections, which were resolved successfully with dressing with povidone-iodine 5% w/v-soaked gauze pieces and oral antibiotics alone [9,10,14,23]. The frame configuration of ilizarov apparatus is helpful in proper care of the injured soft tissue and procedures such as cross flaps and vascular procedures. It improves and increases venous and lymphatic return, preventing swelling and disuse osteopenia [26]. The risk of infection and subsequent osteomyelitis and septic non union associated with other forms of fixation is also minimised [24]. There were three patients who developed stiffness of knee joint, and had to undergo physiotherapy for the same. Among 30 patients, two patients had a leg shortening of 1.5 and 1.2 cm.
Using Johner and Wruh’s criteria, excellent result was obtained in 23 (76.66%), good in 5 (16.67%) and fair in 2 (6.67%) patients. Good to excellent results for complex proximal tibial fractures treated with Ilizarov fixation are shown in multiple other studies [10,13,14,22-24].
Limitation(s)
The limitations of the study were a small sample size along with the lack of control group and inclusion of both closed and open fractures, which may lead to bias in assessing the functional and radiological outcome with ilizarov fixation. Further, as no Magnetic Resonance Imaging (MRI) scanning was done, associated ligament injuries could not be assessed. Lastly, to better monitor the post-traumatic arthritis, a long term follow-up is needed.
Conclusion(s)
Ilizarov technique is a safe and effective method for treatment of proximal tibia fractures with compromised skin condition as it allows early definitive surgery irrespective of skin condition, early weight bearing with mechanical axis restoration and minimal soft-tissue complications resulting in improved functional capacity and fracture union and should be the treatment of choice for these fractures. However, small sample size and no control group limits from making firm conclusions about the results of ilizarov fixation in high energy proximal tibia fractures. Further studies with bigger sample size must be conducted to arrive at concrete conclusions.
ROM: Range of motion