Lower urinary tract symptoms (LUTS) is characterised by storage symptoms of urgency, urgency incontinence, frequency, nocturia, voiding symptoms of slow and/or interrupted stream, terminal dribble hesitancy, straining, and post micturition symptoms of post micturition dribble or incontinence, sensation of incomplete emptying which are quite bothersome [1]. The prevalence of LUTS, according to an international study showed rise with increasing age [2]. The lifetime prevalence of BPH was found to be 26.2% [3]. LUTS in males is often associated with BPH that increases in frequency and symptoms with age [4]. Benign prostatic hyperplasia is a pathological process found in males over 40 years of age that contributes to LUTS [5].
The end results of BPH treatment should be aimed at relief of patients’ symptoms, improvement of quality of life, and altering the progression of the disease [6]. The corner stone of treatment planning in such cases has been established based on the degree of severity and the botherations caused by the disease [7]. Hence, symptom scores are utilised in planning an individualised management policy for BPH patients. The most commonly used symptom score is the International Prostate Symptom Score (IPSS), which assesses the severity of urinary symptoms [8].
Men with BPH had a greater level of bother and interference in selected daily living activities due to urinary symptoms [9]. The improvement of QoL should be a major concern while proposing a treatment modality for any disorder, the improvement of quality of life (QoL) should be kept in mind. The drawback of IPSS is that it is not an accurate tool as its questionnaire does not concern QoL [10].
A new easy to use BPH-specific QoL scale was introduced which is helpful to guide the treatment policy in BPH [11]. The BPH-specific QoL tool should be incorporated in the management of the patients of LUTS with BPH instead of relying on IPSS alone. The objective of the present study was to assess the QoL in patients with LUTS with BPH and compare the outcomes of BPH-specific QoL scale with IPSS.
Materials and Methods
This was an observational study conducted from November 2019 to November 2020, approved by the Institutional Ethical Committee (Approval No. IPGME&R/IEC/2020/647). The study population consisted of patients attending the Out Patient Department (OPD) at the Department of Urology, Institute of Post Graduate Medical Education and Research and Seth Sukhlal Karnani Memorial Hospital, Kolkata, West Bengal, India.
Inclusion criteria: All males aged 50 years, or above aged with LUTS with BPH who voluntarily participated, understood, and signed the consent form were included in the study.
Exclusion criteria: Patients of age less than 50 years, those with the presence of prostate cancer or with history of, previous failed invasive treatment for BPH, having the possibility of any neurological disease, history of pelvic surgery or trauma, history of venereal disease and those taking medications that affect bladder function were excluded from the study.
A total of 400 men were selected for the study. The research protocol consisted of:
(i) BPH-specific QoL scale
The BPH-specific Qol scale was developed by Cam K et al., which consisted of 20 questions related to the QoL due to BPH [11]. A score was given to each of the 20 items on the basis of the degree of the complaint for each particular question [Table/Fig-1]. According to the answers of the patients to each item, the following scores were given as from 0 to 3 with 0/none=no bother at all, 1=little bother, 2=quite a lot (moderate bother), 3=a great deal (severe bother).
BPH Specific Quality of Life (QoL) scale questionnaire.
| 1. Do you have dribbling or sensation of not empty after voiding? If yes, what degree have they interfered your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 2. Do you urinate frequently? If yes, what degree it interfered your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 3. Do you have intermittent voiding or difficulty during voiding? If yes, what degree have they interfered your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 4. Do you have strong desire to void or urine leakage? If yes, what degree have they disturbed your daily activities?a) None b) Little c) Quite a lot d) A great deal |
| 5. Have smaller or weaker force of your urinary stream disturbed your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 6. Do you wait for urination to start or strain during voiding? If yes, what degree have they interfered your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 7. Does getting up to void during the night interfere your life?a) None b) Little c) Quite a lot d) A great deal |
| 8. Do you have pain or burning sensation during voiding? If yes, what degree have they disturbed your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 9. Will you worry if your urinary complaints related with prostate disease keep on in the same way?a) None b) Little c) Quite a lot d) A great deal |
| 10. Have your urinary complains related with prostate disease brought trouble to your daily life?a) None b) Little c) Quite a lot d) A great deal |
| 11. Have you been worried that you would not be able to void or have prostate surgery?a) None b) Little c) Quite a lot d) A great deal |
| 12. Have you been worried that you would have prostate cancer?a) None b) Little c) Quite a lot d) A great deal |
| 13. Have you been worried that you would have urinary infection or blood in urine?a) None b) Little c) Quite a lot d) A great deal |
| 14. How much has your physical condition (activities) been disturbed due to your urinary complaints?a) None b) Little c) Quite a lot d) A great deal |
| 15. Do you think that your urinary complaints disturb your daily activities outside (e.g., shopping, visiting friends?a) None b) Little c) Quite a lot d) A great deal |
| 16. Do you think that your urinary complaints disturb your activities like a long bus or train trip?a) None b) Little c) Quite a lot d) A great deal |
| 17. Have your urinary complaints brought trouble to your appetite or eating habits?a) None b) Little c) Quite a lot d) A great deal |
| 18. Do you think your urinary complaints affect your sexual life?a) None b) Little c) Quite a lot d) A great deal |
| 19. Do you think that your emotional status has been disturbed due to your urinary complaints?a) None b) Little c) Quite a lot d) A great deal |
| 20. Do you think your urinary complaints bring trouble to your general health status?a) None b) Little c) Quite a lot d) A great deal |
| Total Quality of Life (QoL) SCORE:a (none)=0 b (little)=1 c (quite a lot)=2 d (a great deal)=3 |
A total QoL score for all the questions answered by the patient was calculated by adding the score of all 20 questions. The total Questionnaire to assess QoL (Quality of Life) score range was 0 to 60. In the present study, this questionnaire was evaluated and the results were compared.
(ii) International Prostate Symptom Score (IPSS)
The IPSS measures the following seven symptoms with single questions:
(1) Sensation of incomplete bladder emptying
(2) Voiding frequency
(3) Intermittence
(4) Urgency
(5) Urine stream force
(6) Strain to begin urination
(7) Nocturia.
Each question had a range from 0 to 5 for its answer. The highest score of 5 indicated the most severe symptom grade [Table/Fig-2]. On the basis of total score, the symptoms were categorised into mild, moderate, and severe. The total score of IPSS does not take into account the score of the QoL question.
Total International Prostate Symptom Score (IPSS).
| In the past month: | Not at All | Less than 1 in 5 times | Less than half the time | About half the time | More than half the time | Almost always | Your score |
|---|
| 1. Incomplete emptying- How often have you had the sensation of not emptying your bladder? | 0 | 1 | 2 | 3 | 4 | 5 | |
| 2. Frequency- How often have you had to urinate less than every two hours? | 0 | 1 | 2 | 3 | 4 | 5 | |
| 3. Intermittency- How often have you found you stopped and started again several times when you urinated? | 0 | 1 | 2 | 3 | 4 | 5 | |
| 4. Urgency- How often have you found it difficult to postpone urination? | 0 | 1 | 2 | 3 | 4 | 5 | |
| 5. Weak stream- How often have you had a weak urinary stream? | 0 | 1 | 2 | 3 | 4 | 5 | |
| 6. Straining- How often have you had to strain to start urination? | 0 | 1 | 2 | 3 | 4 | 5 | |
| None | 1 Time | 2 Times | 3 Times | 4 Times | 5 Times | |
| 7. Nocturia- How many times did you typically get up at night to urinate? | 0 | 1 | 2 | 3 | 4 | 5 | |
| Total IPSS Score | | | | | | | |
| Quality of Life (QoL) (IPSS score) due to urinary symptoms | Delighted | Pleased | Mostly satisfied | Mixed | Mostly dissatisfied | Unhappy | Terrible |
| If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that? | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
1-7: Mild; 8-19: Moderate; 20-35: Severe
In the study, all the 20 questions from BPH-specific QoL scale were correlated with QoL question of IPSS scale and total IPSS. Self-administration of questionnaires was preferred. The participants with visual deficits and illiteracy, face to face interviews were conducted. Along with the questionnaire, chief complaints, demographic details, and co-morbidities were also taken. The responses on both the scales (IPSS and BPH-specific QoL scale) were noted and the total score was calculated.
Statistical Analysis
The BPH-specific QoL was compared with total IPSS and IPSS QoL score by using the Pearson’s coefficient relation test and Cronbach’s alpha test. All data were analysed using appropriate statistical tests using software such as Statistical Package for the Social Sciences (SPSS) version 24.0 Statistics.
Results
The most men were in the age group 50-60 yrs with median age of 58 yrs. The common presenting complaints were; increased frequency of micturition (100%), intermittency (100%), straining on micturition (98%), poor stream (97%), feeling of incomplete voiding (94%), urgency (87%), nocturia (47%), and incontinence (5.75%). Among the co-morbidities, hypertension (29.5%) and diabetes (23.5%) were prevalent. The urine cultures of all patients in the study were obtained amongst which 309 were sterile, 77 had Escherichia coli and 14 had Klebseilla pneumoniae positive culture. The mean of total score of BPH-specific QoL (mean±SD) of patients was 40.71±6.858. The mean IPSS QoL (mean±SD) of patients was 3.52±.693. In moderate, the mean total score IPSS (mean±SD) of patients was 33.9176±6.6498. In severe, the mean total score IPSS (mean±SD) of patients was 42.5397±5.6648. The BPH- specific QoL and IPSS scales responses were analysed. The correlation of BPH-specific QoL scale questions with QoL question of IPSS was found to be statistically significant [Table/Fig-3,4]. The correlation coefficient of BPH-specific QoL questionnaire was found to be r=0.560 (p<0.0001) with the total IPSS and r=0.376 (p<0.0001) with the QoL score of IPSS [Table/Fig-5]. The correlation of all 20 questions of BPH-specific QoL questionnaire with IPSS QoL score for patients with BPH was also found to be significant [Table/Fig-6]. The reliability i.e., Cronbach’s alpha for BPH-specific QoL was found to be 0.879. The BPH-specific scale questionnaire was more comprehensive regard to QoL than IPSS.
Pearson’s correlation of BPH specific QoL with IPSS QoL score.
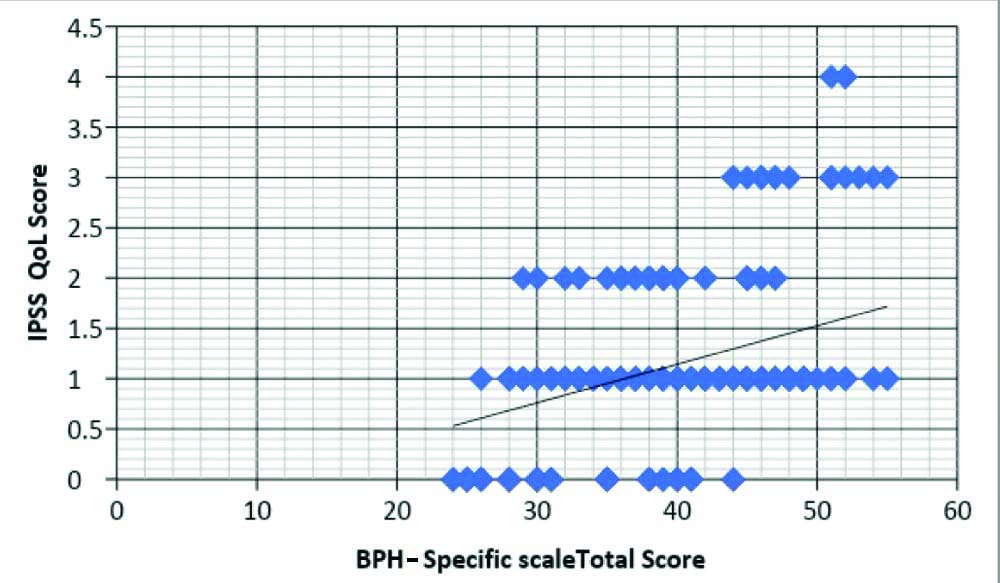
Pearson’s correlation of BPH-specific QoL with total IPSS score.
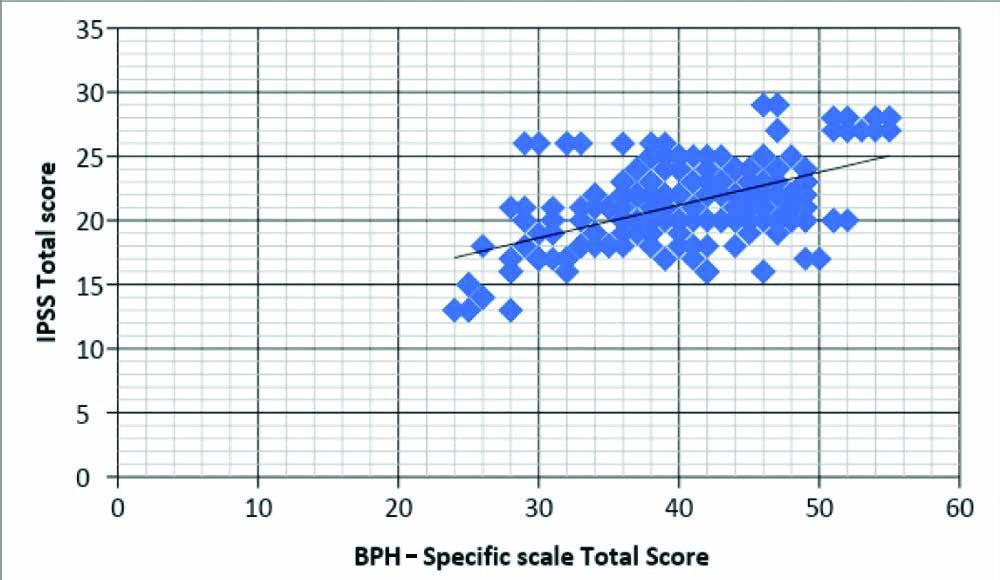
Pearson’s correlation between total score of BPH scale and QoL score on IPSS Scale.
| Comparative analysis | BPH specific scale total score |
|---|
| IPSS Total score | Pearson’s correlation | 0.560** |
| p-value | <0.0001 |
| N | 400 |
| IPSS QoL score | Pearson’s correlation | 0.376** |
| p-value | <0.0001 |
| N | 400 |
*bold p-values are significant
The correlation of all 20 questions of BPH-specific QoL questionnaire with IPSS QoL score for patients with BPH.
| Q. No. | Correlation coefficient |
|---|
| 1 | 0.207 |
| 2 | 0.207 |
| 3 | 0.242 |
| 4 | 0.169 |
| 5 | 0.288 |
| 6 | 0.261 |
| 7 | 0.260 |
| 8 | 0.118 |
| 9 | 0.257 |
| 10 | 0.146 |
| 11 | 0.289 |
| 12 | 0.253 |
| 13 | 0.154 |
| 14 | 0.288 |
| 15 | 0.167 |
| 16 | 0.260 |
| 17 | 0.160 |
| 18 | 0.045 |
| 19 | 0.198 |
| 20 | 0.349 |
Discussion
Lower urinary tract symptoms due to BPH worsens with increasing age. History, physical examination, laboratory investigations and urodynamic tests are helpful to identify the lower urinary tract symptoms. A validated questionnaire usually the international prostate symptoms scale (IPSS) is a simple and reliable score to assess the presence, type, and severity of urinary symptoms and to measure the response to treatment. The IPSS has high internal consistency with good test-retest reliability. It is of paramount importance to plan treatment strategy and to monitor response to treatment given or the progression of the disease during the follow-up [8].
In most of the clinical cases, the treatment planning based on the severity of the symptoms and the amount of inconvenience to the patient. In patients with mild (IPSS <7) symptoms, a wait and watch approach is considered. In such scenario, the patient is closely monitored by the urologist without any intervention for LUTS. In patients with moderate to severe (IPSS >8) symptoms which are causing bother, treatment options available are medical therapy, minimally invasive surgical therapy, and conventional surgical therapies [7]. The drawback of IPSS noted in such cases is that it does not take into account the botherations caused due to LUTS and their interference with daily activities [8].
In a study conducted regarding the impact of BPH on the general well-being of men with BPH showed that men with BPH had higher prevalence of negative feeling of well-being compared to those who did not have BPH. The negative well-being was caused by bother, and interference in daily living activities due to urinary symptoms. Patients’ state of being comfortable should be taken into account in the clinical management of BPH [9].
European Urology guidelines state that “the aim of the treatment is to improve LUTS and patient’s QoL as well as to prevent BPH-related complications” [12]. A recent comprehensive clinical guideline for LUTS suggests incorporation of a QoL scale in the treatment program [13]. Moreover, QoL seems to be much less sensitive to international differences than symptom prevalence [14]. Therefore, QoL should be used to guide the treatment of such patients.
To overcome the drawback of IPSS, the assessment of patient’s QoL specific to each of the seven questions on the IPSS was evaluated using a novel visual analog scale questionnaire. It was helpful to identify the patient’s chief complaint as well as its effect on patient’s specific quality of life [15]. The presence of symptom due to BPH and bother caused by it are two different things and IPSS fails to address the concern of QoL in these patients.
In 2003, a 74-item QoL scale for BPH which included five domains (disease, physical, social, psychological, satisfaction) of the bother by symptoms was developed for patients with BPH in China. This scale had good reliability and validity but it was found to be cumbersome and time consuming to complete 74 items [16]. So a 33-item QoL scale for BPH was constructed which was less time consuming. The 33-item scale and 74-item scale had no significant difference between them in terms of reliability [17].
Cam K et al., in 2012 developed the BPH-specific QoL scale consisting of questionnaire with 20 items. This questionnaire was found to have Cronbach’s alpha value of 0.8464 which confirmed its strong internal consistency. The correlation coefficients of BPH-specific QoL questionnaire were found to be r=0.801 (p<0.0001) with the total IPSS and r=0.567 (p<0.0001) with the QoL score of IPSS. They postulated that response to change in treatment of BPH can be assessed by comparing pre-treatment and post treatment QoL scores [11].
In the present study, we used the same BPH-specific QoL scale, and the correlation coefficients of the BPH-specific QoL questionnaire were found to be r=0.560 (p<0.0001) with the total IPSS and r=0.376 (p<0.0001) with the QoL score of IPSS. The correlation was found to be statistically significant. In a study by Haltbakk J et al., on the importance of LUTS in men and their impact on the QOL, they found that the World Health Organisation (WHO)-QOL was inconclusive to identify relations between specific symptom-related factors. The LUTS suggestive of BPH and LUTS-associated factors are not related to QOL [18]. Coyne KS et al., in their study found that the negative effect of LUTS was apparent across several domains of HRQL. These symptoms also affected the overall perception of bladder problems, general health status, and mental health [19].
Pintarelli VL et al., in their study regarding quality of life of the elderly men and lower urinary tract symptoms, concluded that for elderly men, moderate to severe LUTS had considerable impact on all parameters of QoL proposed by the WHO, particularly the social and environmental relations [20].
The present study showed validity of BPH-specific QoL scale for patients with LUTS with BPH. This score not only helps to know the bother caused by the symptoms but it may also be helpful to assess the success of medical and surgical treatment. This self assessment scale can be used to assess QoL in patients with BPH and also helpful to decide the treatment and monitor its outcome.
Limitation(s)
In BPH-specific QoL, a score cannot be assigned to the patient above 60 years for the question regarding sexual life in BPH-specific scale as these patients of age above 60 were either sexually inactive or had spouse death. So, proper response was not appreciated in such conditions.
Conclusion(s)
The correlation of BPH-specific QoL scale and IPSS was found to be significant. The BPH-specific QoL scale is very much useful and more comprehensive in addressing the QoL in patients with LUTS due to BPH than the IPSS scale. The BPH-specific QoL scale was brief, easy to administer, and revealed the psychological effects such as fear of cancer, fear of surgery associated with BPH.
1-7: Mild; 8-19: Moderate; 20-35: Severe
*bold p-values are significant