The children are the future human capital of any nation and their health status is highly reliable index of nation’s progress on health [1]. The surrogate index of children’s health also shows the level of social protection of a county. Children, especially of the age group of under-five face many ravages in the community and they suffers from diseases like diarrhoea, breathing infections, measles, and pneumonia [2,3]. The initial part of human life during early childhood plays an important part of life, during this period 40% of physical and 80% of psychological development occurs [4]. It is well recognised that a child may got affected several times in a year, the incidence of morbidities increases with the aggravation of a state of infections [4]. Worldwide, 29,000 children among under-five years of age die due to causes which are of preventable in nature [5]. The tackling of morbidity among under-five is not a simple task to be done in an underdeveloped tribal area. Various interrelated determinants come into play in the morbidity and mortality of children [6]. Thus a series of approaches and policies have to be made to deal with such kind of health hazards among under-five children [6]. The policies have to be targeted to remove the issues of access to healthcare for better outcomes.
Indian health system is more vulnerable for children, with higher chances of diseases like diarrhoea, Acute Respiratory Infection (ARI), pneumonia, fever, anaemia, and malnutrition [7,8]. Worldwide, India had the highest number of under-five children (127 million), which has also the largest number of under-five mortality (2.1 million) according to a report [9]. According to National Family Health Survey-4 (NFHS-4), the common morbidities among under-five are diarrhoea, ARIs and anaemia [10]. The incidence of diarrhoea remains nearly constant among under-five children, whereas the prevalence of ARI was halved in between NFHS-3 and NFHS-4 [10-12]. Worldwide, diarrhoea is creating havoc in terms of morbid conditions and cause of mortality among the most vulnerable under-five children [13]. The diarrhoea is one of the main causes of childhood mortality responsible for death of one in ten child seriously affected by it [14]. Nearly seven lac of under-five children constituting approximately 16% of childhood death occurs due to diarrhoea [3]. Around 88% of diarrhoeal death occurs due to unsafe water, poor sanitation, and unhygienic conditions [15]. The nutritional deficiency is a factor for increased morbidity burden in poor countries which are otherwise classified as low and middle income countries. The malnourished children are likely to die out of illness, also belongs to poor families and lack of resources for the treatment of diseases in poverty laden countries [16,17]. It is a sensitive indicator of inequity and poverty, worldwide, 25 to 35 million of children among under-five age groups are suffering from severe acute malnutrition [18]. Prevalence of under nutrition almost the same in all Indian states [19]. The situation is very difficult for Governments to provide care.
Acute Respiratory Infection (ARI) is also a common concern of disability and death among under-five children of poor nations [20]. According to World Health Organisation (WHO), ARI in under-five is responsible for 3.8 million death worldwide [21]. Although the vaccine can tackle diseases like measles, poliomyelitis, diphtheria, tetanus, and whooping cough, still these diseases pose a threat, they continue to infect the children [22]. Globally, 2.3 million of under-five children still die due to vaccine preventable diseases [22]. The reduction of morbidities depends on the effective interventions like provision of clean water and sanitation [22,23]. Children from the backward communities are more prone to diseases due to certain adverse realities like cultural and socio-economic factors, unhealthy personal habits, lack of nutrition, illiteracy, overcrowding and lack of health facilities [24].
The objective of the study was to understand the socio-demographic and morbidity pattern among the children of under-five in a district of Telangana state, India. The study further enquires about the accessibility of healthcare needs at community level.
Materials and Methods
A cross-sectional study was undertaken by interviewing mothers with the help of a predesigned and pretested questionnaire to understand the under-five child morbidity pattern in the rural areas of Narnoor Mandal of Adilabad district, Telangana, India. Ethical approval for the study was cleared from the Institute Ethics Committee University of Hyderabad prior to the commencement of the study with reference number UH/IEC/2015/98 dated 04.02.2015. The study was conducted in 30 villages of tribal area out of 146 villages of Narnoor Mandal of Adilabad district, which has a population of 51,065. The population of the study area is served by PHC Narnoor, PHC Jharia and PHC Gadiguda under Narnoor cluster. The study was conducted during 1st of March to 25th of March 2015 in 30 villages. The study assess various determinates of morbidity by applying scientific principles.
The sample size was calculated as 210 according to the scientific sampling frame obtained from Anganwadi centers of each village. All respondents were identified by door to door survey. Verbal informed consent was obtained from each of the mother and they were assured that the information obtained will be confidential, and only be used for the purpose of this study in an aggregated manner. Ethical approval for the study was cleared from the Institute Ethics Committee University of Hyderabad prior to the commencement of the study with reference number UH/IEC/2015/98 dated 04.02.2015.
Inclusion and Exclusion criteria: The parents (preferably mothers) of under-five children residing permanently in the study area were included in the study. The inclusion criteria for respondents were considered due to the responsibility of parents as key information regarding morbidity pattern. The mothers having major health concerns were excluded due to biases and incomprehensiveness in detailing the issues. The mothers having grown up children above the age of five were also excluded. The mothers having children below the age of five and identified by the Anganwadi workers were mostly included in the study. Under-five years old children those parents (preferably mothers) are not residing permanently in the study area were excluded.
Pretested and semi-structured questionnaire following standard questionnaire of UNICEF was used for interviewing mothers to collect information on childhood diseases among under-five years of children [26]. The questionnaire contains parameters related to socio-demographic factors. The prevalence of various morbid conditions like ARI, worm infestation, diarrhoea, ARI were also studied along with fever, scabies, asthma and fits (seizure).
Statistical Analysis
The data was analysed by using MS Excel spread sheet and Statistical Package for the Social Sciences (SPSS) Version 21.0 software to understand the morbidity pattern. Descriptive statistical tests were done by using SPSS to find out the results according to the objective of the study.
Results
The finding section reports the details of socio-demography of children and patterns of illness. Cross tabulation was also done to understand the nuances of disease pattern among gender, age group, and tribes. All the mothers (n=210) of children under-five years of the rural areas of Adilabad district, Telangana were administered the questionnaire.
Out of 210 study subjects, 14 (6.7%) were from Kolams community, 62 29.5%) were from Gonds community, 82 (39%) belong to Lambadies community, 10.9% belong to Naikpods (n=23) community and 29, 13.9% belong to Pradhan community, all of them were from scheduled tribe. Majorities of study subject (52.8%, n=111) were male and 47.2% (n=99) were female under-five children. The number of children in the age groups 0-1 year is 18%, 1-3 years is 65.3% and 3-5 years is 17.1%, respectively. The details of demographics were given in [Table/Fig-1].
Socio-demographic profile of the children according the respondents (parents of the children).
| Parameters | Number (N) | Percentage (%) |
|---|
| Age (years) |
| 0-1 | 37 | 17.6% |
| >1-3 | 137 | 65.3% |
| >3-5 | 36 | 17.1% |
| Gender |
| Male | 111 | 52.8% |
| Female | 99 | 47.2% |
| Name of tribe (tribe wise distribution pattern) |
| Kolam | 14 | 6.7% |
| Gonds | 62 | 29.5% |
| Lambadies | 82 | 39% |
| Naikpods | 23 | 10.9% |
| Pradhan | 29 | 13.9% |
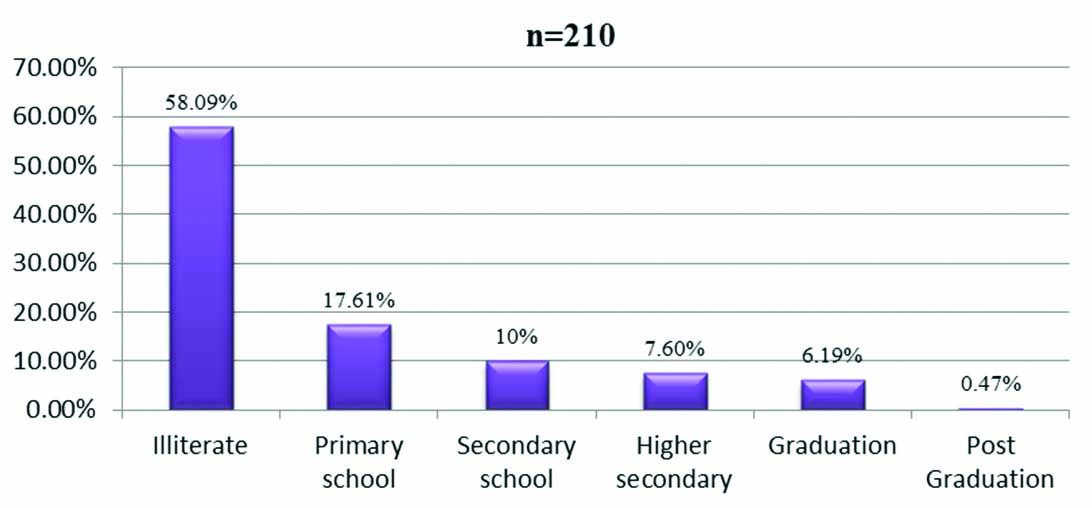
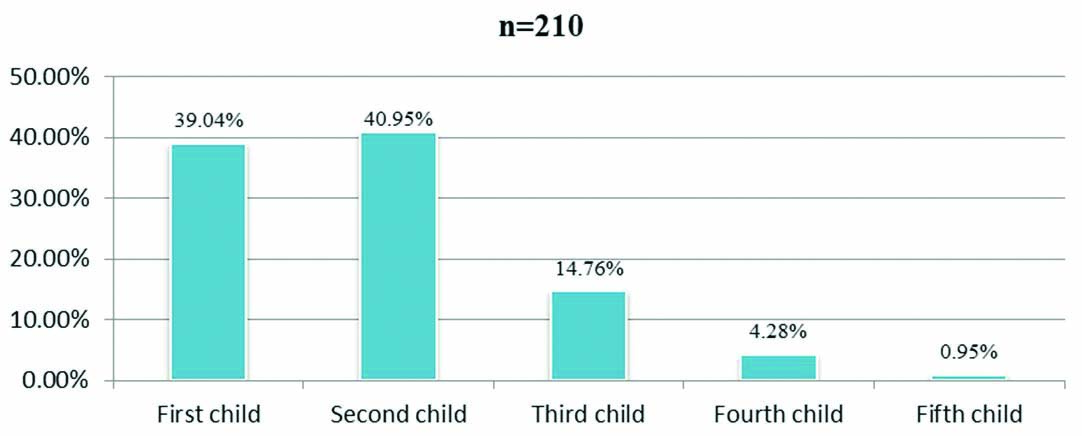
The majorities 58.09% of the mothers were literate, 17.61% mothers are from primary schools, 10% are from secondary schools, 7.6% are from higher education, 13% had completed their graduation and only 1% had completed postgraduation. Out of 210 children from the community, 39.04% were the first child, 40.95% were second child, 14.76% were third child, 4.28% were fourth child and 0.95% was the fifth child. The details of mothers education and birth order is given in [Table/Fig-2,3].
Percentage distribution of mother’s education among the subjects.
Birth order wise distribution of children under five years.
The current study found that 154,73.33% of under-five children are facing some form of morbidities. The most common morbidity was ARI (26%, n=54) which is followed by diarrhoea (20%, n=42) worm infestation (8%, n=17). The ARI is a cause of concern for the children in the area among all he tribes of rural community. The details of the morbidity condition are depicted in [Table/Fig-4].
Pattern of under-five children in the factors of sex and illness.
| Present illness | Male (n=111) | Female (n=99) | Total (n=210) |
|---|
| n | % | n | % | n | % |
|---|
| Diarrhoea | 21 | 18.9% | 21 | 21.2% | 42 | 20% |
| Asthma | 2 | 1.8% | 3 | 3% | 5 | 2.38% |
| Malaria | 0 | 0 | 0 | 0 | 0 | 0 |
| Worm infestation | 6 | 5.4% | 11 | 11.1% | 17 | 8.09% |
| Acute respiratory infection | 24 | 21.7% | 30 | 30.3% | 54 | 25.71% |
| Fever | 10 | 9% | 6 | 6.1% | 16 | 7.61% |
| Scabies | 11 | 9.9% | 5 | 5.1% | 16 | 7.61% |
| Seizure (fits) | 2 | 1.8% | 2 | 2% | 4 | 1.9% |
| No disease | 35 | 31.5% | 21 | 21.2% | 56 | 26.7% |
| Total | 111 | 100% | 99 | 100% | 210 | 100% |
Cross tabulation was done to understand the morbidity pattern of under-five children in relation to gender (sex) and illness condition. Interestingly female under-five-children were affected more (30.3%, n=30) by ARI more than the male (21.7%, n=24). Overall, male children (31.5%, n=35) are less affected by morbid condition and free from diseases than their female (21.2%, n=21) counterparts. The details of the pattern of under-five children in relation to the factors of sex and illness are given in the [Table/Fig-4].
Cross tabulation was done to understand the morbidity pattern of under-five children in relation to age and illness condition. Interestingly, diarrhoea was prevalent among the children of 0-1 years of age (24.4%, n=9) and 1-2 years of age groups (23.3%, n=23) than the higher age groups of 3-5 years (2.8%, n=1). In a similar fashion the conditions like acute respiratory diseases and fever are also higher among the lower age group of under-five children. The details of the pattern of under-five children in relation to the age group and illness are given in the [Table/Fig-5].
Pattern of under-five children in accordance to age and suffering from illness.
| Present illness | 0-1 years | >1-3 years | >3-5 years |
|---|
| (n=37) | (n=137) | (n=36) |
|---|
| No. | % | No. | % | No. | % |
|---|
| Diarrhoea | 9 | 24.4% | 32 | 23.3% | 1 | 2.8% |
| Asthma | 0 | 0% | 5 | 3.6% | 0 | 0% |
| Malaria | 0 | 0% | 0 | 0% | 0 | 0% |
| Worm infestation | 1 | 2.7% | 2 | 1.5% | 14 | 38.9% |
| Acute respiratory infection | 15 | 40.5% | 37 | 27% | 2 | 5.6% |
| Fever | 4 | 10.8% | 12 | 8.8% | 0 | 0% |
| Scabies | 2 | 5.4% | 3 | 2.2% | 11 | 30.5% |
| Seizure (fits) | 0 | 0 | 3 | 2.2% | 1 | 2.8% |
| No Disease | 6 | 16.2% | 43 | 31% | 7 | 19% |
| Total | 37 | 100% | 137 | 100% | 36 | 100% |
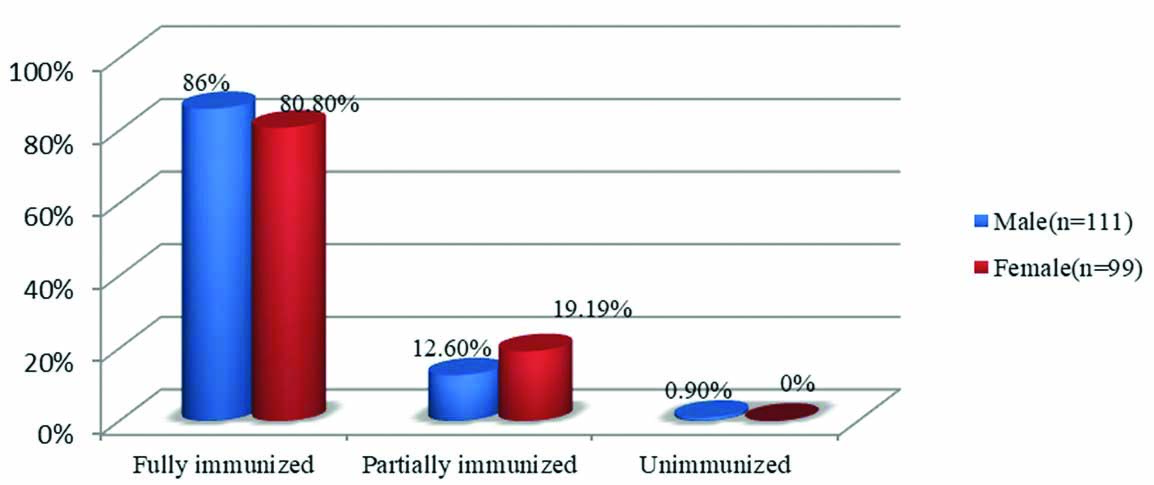
The male children were slightly higher rate of immunisation in relation to the female under-five children. The details of the immunisation pattern are also given in the [Table/Fig-6].
Immunisation status of the children in the study.
Discussion
In this study, all the mothers of 210 under-five children of rural areas of Adilabad of Telangana were interviewed and disease condition of their wards assessed. The majority of the population were 39.04% (n=82) belongs to Lambadies community, which is followed other tribal communities like Gonds, Kolams, Naikpods and Pradhan community from schedule tribe. In this study, ARI (25.71%) and diarrhoea (20%) are the major health problems, and leading cause of morbidity among the study population. Similar prevalence of diseases among various communities were also reported by many researchers [27,28]. These findings are similar with the findings of Mihir G and Geeta K with the incidence of respiratory tract infection and diarrhoea was higher among the children below four years of age [27]. The study also report presence of 7.4% of respiratory infections and 3.7% diarrhoea among the study population [27].
Another evidence confirmed by Ukey UU and Chitre DS, was that the ARI, pneumonia, and gastrointestinal tract infections consists the major cause for high morbidity among the children [28]. Similar studies by Vyas S et al., also showed that diarrhoea is a concern for ill health for long time among the children below five years of age [4]. A study by Ganguly E et al., also confirmed about the prevalence of diarrhoea between the years 2002 and 2013 was 21.70%, which is significantly associated with malnutrition, anaemia, and low socio-economic status among the children [3]. During 1990s diarrhoeal diseases were the major cause of morbidities and during 2000s ARIs were the major cause of morbidities among the children as revealed by different authors [4].
This study shows that other morbidities like worm infestation (8.09%), viral fever (7.61%), scabies (7.61%), asthma (2.3%), and fits (1.9%) were present among the under-five children. The prevalence might have been increased due to the harmful effects of environment, poor hygiene, lack of sanitation, unfavourable socio-cultural practices, and open field defecation. A similar study by Srinivasan K and Prabhu GR, showed that the common diseases among the children were skin infection (25.7%), dental disorders (21.5%), worm infestations (21.6%), Vitamin B deficiency disorders (3.2%), ARIs (1.7%), diarrhoea (1.2%), anaemia, and helminthiasis was highest among boys [29]. Researchers also found that the major diseases are acute respiratory diseases, skin diseases, injuries, Vitamin B deficiency, diarrhoea and eye diseases [29].
The newborns are more prone to the morbidities like ARIs, diarrhoea, and malnutrition due to inadequate food intake, decreasing immunity and faulty weaning and breast feeding practice. So the importance of continued breast feeding after six months of age as a critical intervention to protect the children from some of the morbidities throughout the first two years of life. So the breastfeeding promotion programs, policies and strategies should be developed to inspire mothers to provide breast feeding for six continuous months and to be continued for the following 18 months along with other supplements. Another study in tribal area revealed that anaemia (96.5%) and splenomegaly (30.1%) were common morbidities found among the children [30]. Evidence from tribal area of Maharashtra, India revealed that the anaemia (30%) and acute painful events (20%) are the most common morbidities among the children [31].
In the current study, the majorities (58.09%) of the mothers were illiterate among the study population, which is strongly associated with the occurrence of diseases among children. Illiteracy of the parents is found to be a predicting and predisposing factor for the childhood morbidities, hence, it is necessary to increase education of the parents. Further, there is requirement of improvement in the housing, sanitation, and hygienic conditions. To make child healthy, the regular anthropometric measurements should be taken for measuring the growth and development of the children in the Anganwadi centers as well as at the schools. Evidence from Pakistan found that diarrhoeal cases among children increased with decrease in educational attainment of mothers [32]. A similar finding in Southern Ethiopia, revealed that the prevalence of diarrhoea (30.5%) is the highest among under-five children which is strongly associate with lack of education and poor hand washing practices of mothers [33]. The findings of a study in Southern Ethiopia showed that poor housing, poor sanitation condition, poor personnel hygiene and lack of relevant knowledge are strongly associate with the occurrence of diarrhoeal diseases among the children below five years of age [34]. A study in Odisha reveals that educational intervention and health promotion minimises the prevalence of diarrhoea among children [35].
In the current study, the immunisation status of the study population was good, 86% of male children were fully immunised where as 80.80% of female children were fully immunised. Immunisation is the most important interventions for the reduction of the child hood morbidities like tetanus, poliomyelitis, and measles, so the program should be expanded as per the strategies of global immunisation vision for increasing immunisation coverage through regular monitoring and documentation regarding success and failure of immunisation activities at local levels. A study by Narkhede V et al., reported that, only 33.9% of the total children were completely immunised whereas majority of them were partially immunised [1]. Immunisation status of male child was comparatively better than the female child the reason for the differential immunisation status is the male child preference is higher compared to the female child in the northern Indian society [1]. Hence, emphasis on immunisation program could leads to immediate achievement of good health status among the tribal under-five children.
The finding of this study in comparison to recent 10 years studies of India is given in the [Table/Fig-7] [36-41]. The major points highlighted are regarding disease morbidity pattern and some of the socio-economic causes linked to the under-five health conditions across India.
Morbidity pattern of under five years children, and comparison of various recent studies [36-41].
| Authors | Year of study | Place of study | Main findings comparable with present study |
|---|
| Gulati B et al., [36] | 2021 | New Delhi, India | There is declining order of deaths among the age group below five years among male and female children from 1989 to 2015. |
| Roja VR et al., [37] | 2020 | Karnataka, India | The factors like under-nutrition and low income family was found to be very high among children of illiterate mothers. |
| Sharma A et al., [38] | 2020 | Ujjain, India | Factors like malnutrition, mother education, unhygienic condition pose risk to the under-five morbidity condition, which is also associated with dehydration among childhood making the situation much worse. |
| Vikram K and Vanneman R [39] | 2019 | Survey by Cambridge University | Parental knowledge plays an important role with medical care, immunisation, reduction of underweight, and reduction of diseases among children. |
| Neogi SB et al., [40] | 2016 | Bihar, India | The adoption of Kangaroo Mother Care (KMC) acts as a powerful method for reduction of morbidity and mortality of preterm/Low Birth Weight (LBW) neonates. The study shows by adopting KMC there is improvement in morbidity pattern among babies. |
| Raj A et al., [5] | 2010 | NFHS-3 data, entire India, 2008 | Incidence of malnutrition is dramatically higher among children born to those mothers who got married at an early age, of being minors, in comparison to those married after achieving the age of majority. |
| Tigga PL et al., [41] | 2015 | Bengal, India | Under-nutrition contributed very high to the under-five child morbidity pattern. The study found that the age-specific mean low Mid-Upper Arm Circumference (MUAC) in the range of 126.1-142.5 mm for boys, whereas, for girls it range in between 126.9-136.4 mm (girls). |
Limitation(s)
This study was cross-sectional type, which hinder the understanding of many diseases among under-five children having seasonal fluctuation. The longitudinal study can address many issues of causal and cyclical concerns among under-five children. The study area is of tribal dominated people, which limit the study to have a comparison with other areas. The inferences of the study can be compared with similar tribal areas instead of generalising with other parts of India. The health of mother and children needs to be studied together to understand the social determinants of health. By only including the health conditions of children, the study lacks insight of holistic approach.
Conclusion(s)
There is need for well-trained community health workers to tackle the common illness like ARI and diarrhoea among the children in the study area. Further, the provision of mobile health vans is required for treatment at door step, given the appalling situation and severity of disease profile of the under-five children among various tribal communities. The improvement of the knowledge on childcare need to be addressed immediately by provision of home healthcare management of common ailments and health education. The media need to be active to disseminate information on gender equity and equality by putting emphasis on the health of both male and female child without discrimination. There is immediate requirement of nutritional schemes to protect the health of under-five children according to targeted intervention. The health of children is paramount given the high prevalence of many preventable diseases in the study area. Further, micro level research studies could be conducted among tribal population to find out the health status of children, which would help in reducing morbidity and mortality ultimately. Hence, targeted intervention is required based on the theories of Social Determinant of Health (SDH). The control of biological causes of diseases can be managed by suitable intervention on SDH in short and long term plans in the study area.