Posterior fossa tumours are more common in children than adults. They account for 54-70% of all brain tumours in children and 15-20% of adult brain tumours [1]. Cushing reported a large series of posterior fossa tumours and published information of 61 patients with the medulloblastoma with poor outcome [2]. Critical location of tumour leads to brainstem compression and death. Posterior fossa tumours like medulloblastoma, ependymoma and pilocytic astrocytoma are more common in children, while tumours including metastasis, lymphoma, glioma and haemangioblastomas are more common in adults [3]. Hydrocephalus is common presentation of children with posterior fossa tumours, but CSF diversion alone in children with resectable posterior fossa tumour is controversial [4].
Clinical presentation varies according to site, rate of growth and biological behavior of tumour. Symptoms may be due to focal compression on the cerebellum, brainstem, cranial nerves or due to raised intracranial tension [3].
Surgery achieves decompression of posterior fossa, provides information about type of tumour and helps in planning further treatment. Gross total resection is appropriate treatment in all posterior fossa tumours. A 25 years survival in case of pilocytic astrocytoma exceeds 94%. In Medulloblastoma 5-year progression free survival is 20-70%. In Ependymoma 5-year survival rate is 67-80% [5-7]. Choroid plexus carcinoma has poor prognosis. Surgical outcome has improved over years of evolution of surgery. With operating microscopes, better imaging modalities, complications following surgery have also significantly reduced. In a similar study, it was observed that absence of hemiparesis papilloedema and meningismus had more chances of satisfactory surgical outcome [8]. Aim of the study was to analyse data regarding surgical outcome of posterior fossa tumours.
Materials and Methods
A retrospective study was conducted in the Department of Neurosurgery, Government Medical College Thrissur, Kerala, India, from March 2015 to February 2020. Analysis of data obtained was done in April 2020 to May 2021. Case sheets of patients who underwent surgery in the specified time period for posterior fossa tumour were collected from library records after getting permission from Institutional Ethics Committee (IEC/GMCTSR/092/2021).
Inclusion and Exclusion criteria: All the posterior fossa tumours operated in the Department of Neurosurgery, Government medical college Thrissur, Kerala, India, from March 2015 to February 2020 were included in the study. Cases without recording of preoperative and postoperative clinical findings and investigations were excluded from the study.
Preoperative clinical examination and results of imaging investigations like Computed Tomography (CT) scan, Magnetic Resonance Imaging (MRI) were recorded from the case sheet. Postoperative clinical examination findings till discharge were also noted. Histopathology of the tumour was obtained from the register maintained in the department. Surgical outcome was assessed as excellent, good, acceptable or poor according to the clinical examination findings and radiological assessment at the time of discharge.
Near total excision of tumour without neurological deficit or complications was considered as excellent outcome. Decompression of tumour with reversible neurological deficit was considered as good outcome. Decompression of tumour with pre-existing neurological deficit was considered as acceptable outcome. Patients with irreversible neurological deficit, poor Glasgow Coma Scale (GCS), bedridden patients, comatose patients and death was taken as poor outcome [9].
Statistical Analysis
Statistical software Statistical software Statistical Package for the Social Sciences (SPSS) version 20.0 was used to analyse data. Frequency and percentage computed for categorical variables like age, gender, age group, diagnosis, surgical outcome, complications and histopathology were noted. Mean, median and standard deviation at 95% confidence interval was computed for quantitative measurement.
Results
A total of 63 patients were operated during the study period. There were 14 (22.22%) paediatric and 49 (77.77%) adult patients were operated. Mean age of the patients was 41.86±21.75 years. Of the total 63 patients, 29 (46%) were males and 34 (54%) were females [Table/Fig-1,2].
Age group of posterior fossa tumour.
| Age group (years) | Number | Percentage (%) |
|---|
| 0-10 | 11 | 17.46 |
| 11-20 | 1 | 1.58 |
| 21-30 | 3 | 4.76 |
| 31-40 | 6 | 9.52 |
| 41-50 | 2 | 3.16 |
| 51- 60 | 15 | 23.80 |
| 61-70 | 13 | 20.63 |
| 71-80 | 12 | 19.04 |
Sex distribution of posterior fossa tumours.
| Sex | Number | Percentage (%) |
|---|
| Male | 29 | 46.0 |
| Female | 34 | 54.0 |
| Total | 63 | 100.0 |
It was observed that 38 (60.31%) patients had preoperative hydrocephalus of which 26 (68.42%) underwent preoperative Ventriculoperitoneal Shunt (VP shunt). Preoperative motor deficits were found in 15 (23.80%) patients. Motor deficit noted was hemiparesis or unilateral lower limb weakness. Preoperative cerebellar dysfunction was noted in 42 (66.66%) patients [Table/Fig-3]. A total of 34 (53.96%) patients had preoperative cranial nerve involvement and four of them had more than two cranial nerve involvement before surgery.
| Preoperative status | Finding | Number | Percentage (%) |
|---|
| Hydrocephalus | Present | 38 | 60.31 |
| Absent | 25 | 39.69 |
| Ventriculoperitoneal shunt | Present | 26 | 41.26 |
| Absent | 37 | 58.74 |
| Cerebellar dysfunction | Present | 42 | 66.66 |
| Absent | 21 | 33.34 |
| Motor deficit | Present | 15 | 23.80 |
| Absent | 48 | 76.20 |
Most common complication was CSF leak with or without pseudomeningocele.
Postoperative Cerebrospinal Fluid (CSF) leak was found in 9 (14.28%) patients. Seven (11.11%) patients had pseudomeningocele without CSF leak. Hydrocephalus was observed in 15 (23.80%) patients following surgery who needed intervention. Twelve (80%) of them were managed with external ventricular drainage and only 3 (20%) of them needed fresh VP shunt or revision of shunt. New postoperative cranial nerve deficit was observed in 9 (14.28%) patients. Of which eight patients had new onset facial nerve palsy and one had lower cranial nerve palsy [Table/Fig-4].
| Complications | Number (Percentage) |
|---|
| Cerebrospinal Fluid (CSF) leak and pseudomeningocele | 16 (25.39%) |
| Postoperative haematoma | 12 (19.04%) |
| New onset cranial nerve palsy | 9 (14.28%) |
| Wound infection | 6 (9.52%) |
| Meningitis | 4 (6.34%) |
| Shunt obstruction | 3 (4.76%) |
| None | 13 (20.63%) |
Forty-four patients had GCS of 14 or 15 at the time of discharge. Fifteen patients had GCS of 8 to 13 and 4 patients had score less than 8. Near total excision of tumour was noted in eight patients in postoperative CT. Decompression of the tumour with relief in brainstem compression and hydrocephalus was noted in 36 patients.
Of the 63 patients, 25 (39.68%) had vestibular schwannoma, 5 patients (7.93%) had pilocytic astrocytoma, of which four of them were paediatric patients. Four patients (6.34%) had ependymoma of which two were paediatric patients. Metastasis was reported in 4 patients (6.34%). Two each from carcinoma breast and carcinoma lungs. Three patients (4.76%) had medulloblastomas, of which two were paediatric patients [Table/Fig-5,6].
Type of tumour histopathology.
| Histopathological diagnosis | Number (%) |
|---|
| Vestibular schwannoma | 25 (39.68%) |
| Meningioma | 7 (11.11%) |
| Glioma | 7 (11.11%) |
| Haemangioblastoma | 6 (9.52%) |
| Pilocytic astrocytoma | 5 (7.93%) |
| Ependymoma | 4 (6.34%) |
| Metastasis | 4 (6.34%) |
| Medulloblastoma | 3 (4.7%) |
| Epidermoid | 1 (1.5%) |
| Other schwannoma | 1 (1.5%) |
Distribution of tumour among paediatric patient.
| Histopathological diagnosis | Number (%) |
|---|
| Pilocytic astrocytoma | 4 (28.57%) |
| Ependymoma | 2 (14.28%) |
| Medulloblastoma | 2 (14.28%) |
| Glioma | 2 (14.28%) |
| Meningioma | 2 (14.28%) |
| Schwannoma | 1 (7.14%) |
| Hemangioblastoma | 1 (7.14%) |
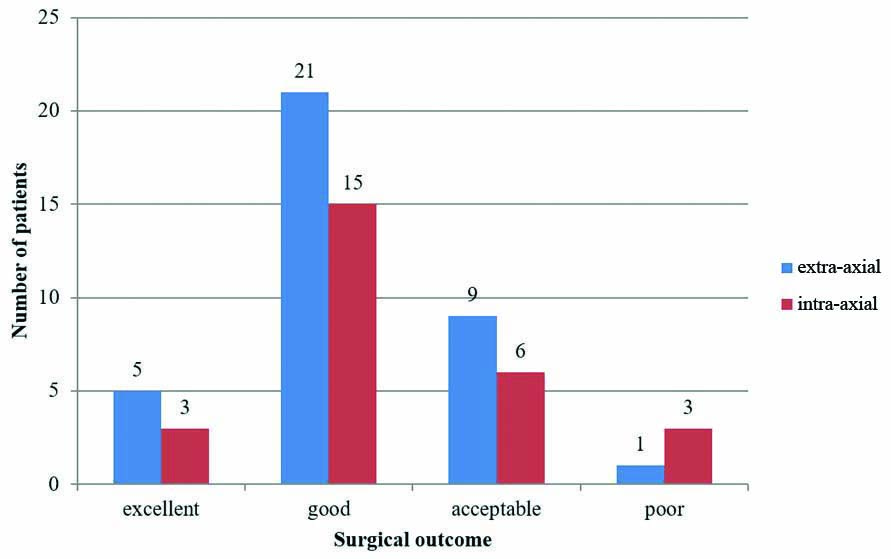
Excellent to good outcome was seen in 44 (69.84%) patients. Fifteen (23.80%) patients had acceptable outcome while 4 (6.34%) patients had poor outcome [Table/Fig-7]. It was observed that 72.22% (26) extra-axial tumours had excellent to good outcome while only 72.22% (26) intra-axial tumours had excellent to good outcome [Table/Fig-8]. Among intra-axial tumours pilocytic astrocytoma had best outcome. All 5 patients (100%) with pilocytic astrocytoma had excellent to good outcome. Preoperative and postoperative image of one of the cases is shown in [Table/Fig-9].
| Outcome | Number (%) |
|---|
| Excellent | 8 (12.69%) |
| Good | 36 (57.14%) |
| Acceptable | 15 (23.80%) |
| Poor | 4 (6.35%) |
Surgical outcome in intra-axial and extra-axial tumours.
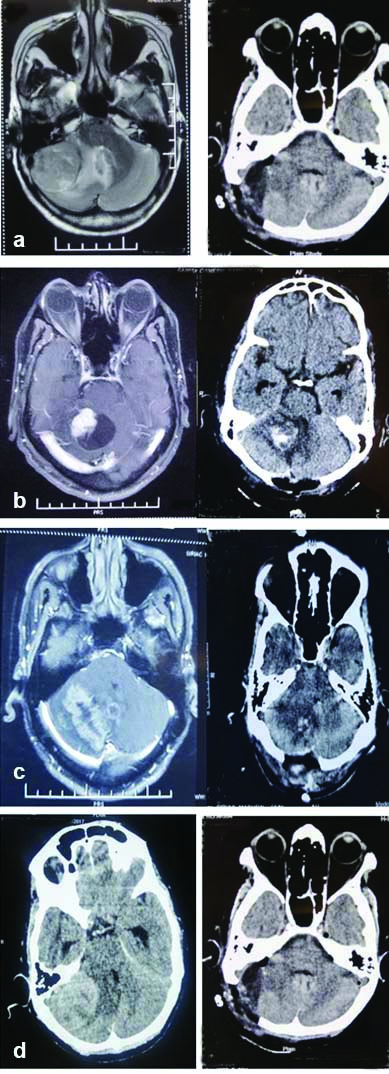
Preoperative and postoperative images of different posterior fossa tumours: a) Vestibular schwannoma; b) Haemangioblastoma; c) Metastasis; d) Meningioma.
Discussion
Posterior fossa tumours are the most frequent primary neoplasm in the paediatric age group. Brainstem compression, cranial nerve involvement and hydrocephalus occur in most of the posterior fossa neoplasm. Reduction of intracranial pressure by tumour excision and CSF diversion thereby relieving brainstem compression is the main goal of treatment. Some may require adjuvant treatment [9].
In the present study of the total 63 patients, mean age of study population was 41±21.75 with age ranging from 1-71 years. Similar results were obtained in study by Roberti F et al., who studied a total of 161 patients with mean age of 47 years [10].
Of the 63 patients, 34 were females while 29 were males. Sex distribution of patients matched with studies conducted at Neurosurgical unit of Kenyatta National Hospital [11]. In most other series, males were predominant. In a study by Ahmed KB et al., out of 546 patients 306 were males and 240 were females [12]. Similar results were observed in another study by Vara Prasad KS et al., where 61.11% (22 out of 36) patients were females [13].
In the present study, 26 out of 38 patients who had preoperative hydrocephalus underwent VP shunt. Robert YS and James GS, found that permanent CSF diversion was needed in 33% patients [14]. In another study by Bartlett F et al., VP shunt was inserted in 53% patients [15].
In the present study, CSF leakage was the most common complication. Sixteen (25.4%) patients had CSF leakage either direct CSF leak or in the form of pseudomeningocele. In a study by Islam MR et al., CSF leak was the most common complication which occurred in 26.7% patients [16]. In another study conducted by Dubey A et al., CSF leak was most frequently encountered complication [17]. Other common complications noted were haematoma in 12 out of 63 (19.04%), of which only one needed surgical evacuation. In a study by Emara M et al., at Benha University, Egypt, haematoma was noted in 13.6% patients [18].
Excellent to good outcome was observed in 44 out of 63 patients (69.8%). Acceptable outcome was noted in 15 out of 63 (23.8%) and poor outcome was noted in 4 patients (6.3%). In a study by Emara M et al., at Benha University, Egypt they had excellent to good outcome in 77.3% (34 out of 44) poor outcome was observed in 22.7% (10 out of 44) [18]. In another study by Shaikh HA et al., at Jinnah Postgraduate University Karachi, they had good outcome in 75.6% (31 out of 41) and poor outcome in 24.4% [19].
Regarding histopathology, vestibular schwannoma was the most common posterior fossa tumour operated. Vestibular schwannoma accounted for 39.7% cases (25 out of 63) followed by meningioma, glioma (11.1% each) and haemangioblastoma (9.5%). These findings correspond to observations in study conducted by Rehman A et al., at King Edward Medical University in 2009 [20]. In another study by Shaikh HA et al., at Jinnah Postgraduate Center, Karachi, vestibular schwannoma was the most common tumour operated, 27% (18 out of 66) followed by 9 glioma (10.6%), 8 meningioma (9.1%) and 7 haemangioblastoma (7.6%).
Another study by Bhat R et al., at Sher-i-Kashmir Institute of Medical Sciences, Srinagar again vestibular Schwannoma was the most common 23.9% (98/4100) posterior fossa tumour [21].
Limitation(s)
The present study has the drawback of being a retrospective single centre study with limited number of patients. Many operated cases were excluded from study due to inadequate documentation of clinical and radiological findings in the library records.
Conclusion(s)
Despite surgical and technical advances posterior fossa tumour surgery still remains a challenge. With early presentation, selection of approach and equipments better results can be obtained. Extra-axial tumours like vestibular schwannoma and meningioma have a better surgical outcome. The CSF leak and haematoma are the most common complications encountered in posterior fossa tumour surgeries.