Pancreatic panniculitis is a rare triad of pancreatitis, panniculitis and polyarthritis. Due to underlying pancreatic disease, there is subcutaneous fat necrosis forming erythematous nodules especially in the lower extremities. This is accompanied with history of multiple joint pain. Timely diagnosis is the key to treatment, as pancreatic disease can progress rapidly causing life threatening complications. Authors hereby presented a rare case of pancreatic panniculitis in a 48-year-old male. Patient had a recent history of acute pancreatitis (alcohol induced) with development of erythema nodosum with pain and swelling in joints. Histopathological examination of the skin nodules revealed panniculitis, associated with elevated pancreatic enzymes on laboratory investigations and patient responded to anti-inflammatory medicines, thereby confirming the diagnosis of pancreatic panniculitis. He was treated with analgesics and steroids which reduced the erythematous nodules.
Case Report
A 48-year-old male patient presented at the Outpatient Department unit in December 2019, with pain and swelling in joints of both the hands, first and fourth toe of right leg for the past three days. Patient had pain in left heel with oedema in both legs (near ankle) 20 days back. Had difficulty in walking due to pain over ankle and feet and difficulty in routine work due to swelling of hands joints.
Patient gave history of hospitalisation for abdominal pain which was diagnosed as acute pancreatitis 20 days back. He had history of alcohol abuse 5-7 days prior of hospitalisation. It was managed with antibiotics, antacids, analgesics, intravenous fluids and supportive management. Within the next 4-5 days he developed polyarthritis and skin lesions. Similar episode of mild pancreatitis had occurred three years back for which he was admitted. He also had history of Koch’s pleural effusion 15 years back for which he had completed anti-tuberculous therapy. There was no history of any drug reaction till date. On enquiring he even confirmed of no family history of any rheumatologic disease. On questioning about his personal habits, he mentioned history of tobacco and alcohol abuse which he had stopped four years back. There were no complaints (in past/present) of chronic headache, any visual disturbances, cough, breathlessness, mouth/genital ulcers, eye redness, high fever for long period, Reynaud’s phenomena, dysphagia, muscle weakness, significant hair fall, bleeding from nose or per rectum/urine.
His general physical examination was normal except pedal oedema. On musculoskeletal examination, he had swelling and tenderness of second metacarpophalangeal joint, second and fourth proximal interphalangeal joint of right hand and first metacarpophalangeal joint of left hand [Table/Fig-1a] along with tenderness of both elbow joints. He had erythematous, nodular, tender swelling over skin of both lower legs above ankle along the medial aspect [Table/Fig-1b] and few non tender, non erythematous swelling over medial side of right thigh. His systemic examinations were normal.
a) Swelling of second metacarpophalangeal and second and fourth proximal interphalangeal joint (right hand); b) Erythematous, nodular, tender swelling along the medial side of ankle.

Laboratory investigations showed elevated serum lipase (1490 UI/L); haemoglobin level of 9.0 gm/dL and white blood corpuscles 7750/cc of blood. His abdominal ultrasound report showed reactive inflammatory wall thickening of the anteropyloric region of stomach, cholelithiasis without cholecystitis, bulky pancreas, hepatomegaly and splenomegaly with enlarged periportal lymph nodes. Based on above laboratory findings he was diagnosed with acute pancreatitis. He was further investigated for rheumatoid factor (7.11 IU/mL), serum uric acid (2.8 mg/dL), serum creatinine (0.8 mg/dL) and routine urine analysis which were within reference range. A dermatologist consultation was obtained with skin biopsy from two different sites of nodular lesions over lower leg. Analgesics were used to reduce the pain with provisional diagnosis of pancreatic panniculitis.
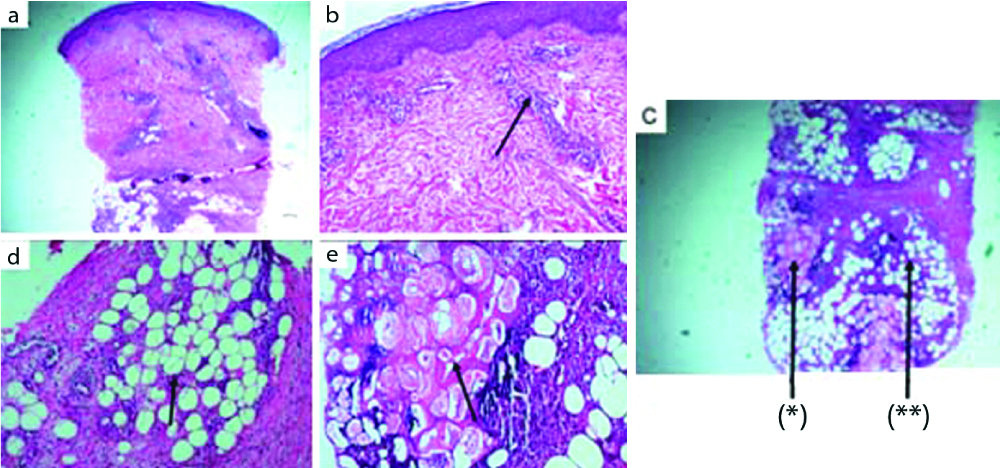
He consulted after five days with reports, Anti-neutrophil Cytoplasmic Antibodies (ANCA) was negative (PR3, MPO <1.0), anti-Cyclic Citrullinated Peptide (CCP) was <7.0 U/mL, Erythrocyte Sedimentation Rate (ESR) 25 mm/hr, C-Reactive Protein (CRP) 21.1 mg/L and Angiotensin-Converting Enzyme (ACE) was 5.9 U/L. His liver enzymes were within normal range and no abnormality was detected on chest x-ray. His skin nodule biopsy revealed characteristic features of fat necrosis with septal and lobular inflammation in deep dermis and subcutaneous tissue. Inflammatory cells were seen mixed with predominantly polymorphs, absence of granuloma and vascular inflammation which were suggestive of panniculitis [Table/Fig-2].
Fat necrosis with septal and lobular inflammation. Inflammatory cells mainly polymorphs seen with vascular inflammation and absence of granuloma: a) Scanner view of punch biopsy skin showing epidermis, dermis and subcutis (H&E stain, 5X); b) Epidermis and dermis with dermal perivascular lymphoid infiltrate (H&E stain, 20X); c) (*) Subcutis with fat necrosis (**) and lobular panniculitis (H&E stain, 40X); d) Lobular panniculitis (H&E stain, 40X) and e) Fat necrosis (H&E stain, 40X).
In view of history of acute pancreatitis (likely alcohol induced) followed by nodular, erythematous swelling and polyarthritis, with skin biopsy showing features of lobular panniculitis confirmed the diagnosis of ‘pancreatic panniculitis’. He was started with non steroidal anti-inflammatory drug.
On repeat follow-up after five days, the joint pain and swelling increased (right hand more) [Table/Fig-3] with significant laboratory findings {White Blood Cell (WBC) was 16830/cmm, serum amylase was 3889 U/L, serum lipase was 28518 U/L, Antinuclear Antibody (ANA)1:100 not detectable, Complement C3 :78 mg/dL, Complement C4: 30 mg/dL, serum IgG was 42.72 and creatinine: 0.65 mg/dL}. Ultrasonography of abdomen was repeated after nine days of first follow-up which showed normal size of pancreas with mild heterogenous echo pattern. Main Pancreatic Duct (MPD) was dilated at the head and body suggesting changes of chronic pancreatitis and pseudocyst. Cholelithiasis without changes of cholecystitis were seen with fatty infiltration of liver and dilated portal vein. Reactive inflammatory wall thickening of the antropyloric region of stomach was decreased as compared to his previous report. Mild to moderate splenomegaly was seen.
Increase in the joint pain and swelling especially right hand in ten days.

He was started with prednisolone (10 mg), non steroidal anti-inflammatory drugs (naproxen 500 mg and paracetamol) and cholecalciferol 60000 units weekly. Patient showed improvement to treatment and his erythematous tender nodules over lower leg also reduced after 10 days [Table/Fig-4]. His laboratory investigations were repeated on follow-up (two months after first consultation in Outpatient Department), which showed, haemoglobin was 11.0 gm/dL, White Blood Cell (WBC) was 9500/cumm, platelet count was 2,52,000/cumm. Serum glutamic pyruvic transaminase (SGPT) was 17 U/L and serum lipase 3000 U/L. Patient was tapered off steroids and was continued only on analgesics. On his last follow-up his skin nodules disappeared, joints pain improved.
Reduction in the erythematous nodules in response to treatment in 20 days

Discussion
Pancreatic panniculitis is a rare variant of panniculitis with evidence of underlying pancreatic disorder in 0.3-3% of cases [1]. Few cases of pancreatic diseases develop subcutaneous fat necrosis leading to formation of nodules with accompanying polyarthritis. Though the exact pathogenesis is unclear, it is suggestive that due to underlying pancreatic disease, the increased pancreatic enzymes cause necrosis of the fat with basophilic alteration of lipocytes seen as ghost cells with no nuclei [2]. Accurate clinical assessment is helpful in early diagnosis as the underlying pancreatic disease might progress to fatal outcomes. Histopathological evaluation of the nodules helps in detecting lobular panniculitis which is suggestive of the diagnosis of pancreatic panniculitis. The case presented here is one such rare occurrence of pancreatic panniculitis with a history of alcohol induced acute pancreatitis. Later patient developed erythematous nodules accompanied with joint pain.
Panniculitis is classified as septal, lobular, or mixed form. Based on histopathological findings, panniculitides are divided into four categories, mostly septal panniculitis without vasculitis, septal panniculitis with vasculitis, lobular panniculitis without vasculitis and lobular panniculitis with vasculitis. A variety of associated systemic diseases and clinical syndromes occur in patients with panniculitis and vasculitis [3]. Therapy depends on the severity and systemic involvement.
Patients with pancreatic diseases may develop subcutaneous fat necrosis (lobular panniculitis) with accompanying polyarthritis and osseous intramedullary fat necrosis [4]. Several pancreatic pathological disorders may lead to the development of panniculitis such as pancreatitis, pancreatitis secondary to cholelithiasis, pancreatic carcinoma (acinar cell), post-traumatic, pancreatic Ischaemia, pancreatic pseudocyst, and pancreatic divisum [5]. The exact pathogenesis is not clear, but it is proposed that the released pancreatic enzyme trypsin indirectly damages the subcutaneous fat causing necrosis and saponification followed by inflammatory process. These mechanisms result in lobular panniculitis which consists of necrotic ghost cells and anucleate adipocytes along with granular amorphous matrix [6]. Histopathologically, extensive fat necrosis with a basophilic altered lipocytes and ghost cells with absent nuclei are commonly seen. Pancreatic panniculitis is a rare variety of panniculitis with anincidence of only 0.3-3% of patients with pancreatic disease [1]. Rarely, it is seen in patients with subclinical pancreatic disease or with no evident pancreatic disease but have high serum levels of pancreatic lipase due to unknown reasons [7]. Clinically, it manifested as characteristic erythematous, tender subcutaneous nodules which might occasionally ulcerate with oozing of thick oily discharge. Pancreatic panniculitis is commonly seen at the distal parts of the lower extremities such as pretibial region, thighs and buttocks; along the breasts and abdomen [6].
Evaluation of panniculitis should include careful history and physical examination. In cases of upper respiratory tract infection, throat swab should be screened for streptococcal infection, skin test and chest radiograph to rule out tuberculosis. Tests for pancreatic enzymes, amylase and lipase should be considered since these are known to have a pathogenic role in causing subcutaneous fat necrosis. This is supported by the findings of these enzymes in the areas of subcutaneous fat necrosis [8]. Histopathological examination is required for confirmatory diagnosis of this entity as it shows characteristic features of lobular panniculitis with intense necrosis of adipocytes.
The treatment of pancreatic panniculitis is chiefly directed at the underlying pancreatic disease like managing pancreatitis, surgical resection of pseudocysts, dissection of necrotising part of pancreas or endoscopic ultrasound guided cyst gastrostomy [9,10]. Acute erythema nodosum is often self-limiting and in majority of cases bed rest and leg elevation are helpful. Polyarthritis should be treated with non steroidal anti-inflammatory medicines. Usually, those cases associated with pancreatitis slowly undergo resolution once the inflammatory episode of the pancreas regresses. When there is involvement of subcutaneous fat other than the lower extremities, persistent disease, frequent relapses, or ulceration, the possibility of an occult underlying carcinoma of the pancreas should be considered [6]. Absence of abdominal symptoms may lead to misdiagnosis or might delay the diagnosis and further delaying the specific treatment of the underlying pancreatitis. This in turn might worsen the prognosis, with mortality rate as high as 24% [11]. Around 45% of the patients with arthritis follow a chronic course showing poor response to nonsteroidal anti-inflammatory drugs and corticosteroids, with rapid progress in joint damage as seen in radiographic images [11].
While comparing similar cases [Table/Fig-5], it was seen that majority of cases are reported in middle aged patients with history of alcohol abuse, as was seen in the above case. The type of pancreatic pathology can vary from acute or chronic pancreatitis, pancreatic carcinoma, abdomen trauma, pseudocyst or fistulas [11-15]. In some cases, there were no abdominal complaints but derangement in the lipase or amylase levels [16].
Summary of previously reported cases [11-15].
| Authors (study) | Age/Sex | Clinical presentation | Development of skin in association with pancreatic disease | Diagnosis | Management | Prognosis |
|---|
| Narvaez J et al., [11] | 45/M | Abdomen pain, nausea vomiting, multiple painful erythematous nodule in both legs and joint pains | Three days after hospitalisation | Acute pancreatitis (alcohol induced), nodular panniculitis and synovitis | NSAIDS, prednisolone, topical therapy for joint wounds. | Abdomen and skin complaints were better but joint pain persisted on follow-up after five weeks. |
| Harris MD et al., [12] | 10/F | Acute pancreatitis from blunt abdomen trauma, painful nodules on legs and acutely painful joints of toes and fingers | After one month | Acute pancreatitis with enlarging pseudocyst, panniculitis | EUS guided cyst gastrostomy | Symptom free at six months follow-up |
| Menon P and Kulshreshta R, [13] | 13/M | Dysponea, generalised oedema, abdomen distension, tender subcutaneous swelling in extremities with tenderness swelling of peripheral joints | After eight weeks of chronic pancreatitis episode | Polyarthritis, panniculitis with chronic pancreatitis and pseudocyst | Aspiration of pseudopancreatic cyst and creating duodenal fistula | Complaints subsided after few weeks |
| Azar L et al., [14] | 47/F | Pain in hands, legs, ankles with painful rash on legs. Abdomen symptoms were not prominent | Not specified | Asymmetric polyarthritis, pancreatic panniculitis | NSAIDS, Prednisolone, conservative treatment for fracture | Symptoms resolved on six month follow-up |
| Dieker W et al., [15] | 62/M | Progressive joint and bone pains with history of acute necrotising head pancreatitis (alcohol induced) | Not mentioned | Pancreatitis, panniculitis, polyarthritis due to post pancreatitis pseudocyst and mesenteric fistula | Partial pancreatico-duodenectomy with resection of the mesenteric fistula and removal of the mesenteric thrombus | No symptoms on follow-up at two months |
EUS: Endoscopic ultrasound; F: Female; M: Male; NSAIDS: Non steroidal anti-inflammatory drugs
Conclusion(s)
In very rare instances, pancreatic diseases can cause inflammation of joints and panniculitis. In cases with these unrelated occurrences, clinicians must consider this diagnosis of pancreatic panniculitis, as if undetected it might be fatal. In such cases, a detailed clinical history and histopathological assessment is the key to diagnosis.
EUS: Endoscopic ultrasound; F: Female; M: Male; NSAIDS: Non steroidal anti-inflammatory drugs
[1]. Rongioletti F, Caputo V, Pancreatic panniculitisG Ital Dermatol Venereol 2013 148(4):419-25. [Google Scholar]
[2]. Camacho PC, Santos E, Pimentão BM, Fraga CE, Simões MJ, Almeida A, Pancreatic panniculitis: Case reportInt Surg J 2020 7(2):606-08.10.18203/2349-2902.isj20200327 [Google Scholar] [CrossRef]
[3]. Gupta P, Saikia UN, Arora S, De D, Radotra BD, Panniculitis: A dermatopathologist’s perspective and approach to diagnosisIndian J Dermatopathol Diagn Dermatol 2016 3:29-41.10.4103/2349-6029.195224 [Google Scholar] [CrossRef]
[4]. Jo S, Song S, Pancreatitis, panniculitis, and polyarthritis syndrome caused by pancreatic pseudocyst: A case reportWorld J Clin Cases 2019 7(18):2808-14.10.12998/wjcc.v7.i18.280831616696 [Google Scholar] [CrossRef] [PubMed]
[5]. Zundler S, Erber R, Agaimy A, Hartmann A, Kiesewetter F, Strobel D, Pancreatic panniculitis in a patient with pancreatic-type acinar cell carcinoma of the liver– case report and review of literatureBMC Cancer 2016 16:13010.1186/s12885-016-2184-626895632 [Google Scholar] [CrossRef] [PubMed]
[6]. Dahl PR, Su WP, Cullimore KC, Dicken CH, Pancreatic panniculitisJ Am Acad Dermatol 1995 33(3):413-17.10.1016/0190-9622(95)91385-8 [Google Scholar] [CrossRef]
[7]. Madarasingha NP, Satgurunathan K, Fernando R, Pancreatic panniculitis: A rare form of panniculitisDermatol Online J 2009 15(3):1710.5070/D37F08V0W919379661 [Google Scholar] [CrossRef] [PubMed]
[8]. Förström TL, Winkelmann RK, Acute, generalised panniculitis with amylase and lipase in skinArch Dermatol 1975 111(4):497-502.10.1001/archderm.1975.016301600870101122151 [Google Scholar] [CrossRef] [PubMed]
[9]. Fraisse T, Boutet O, Tron AM, Prieur E, Pancreatitis, panniculitis, polyarthritis syndrome: An unusual cause of destructive polyarthritisJoint Bone Spine Revue du Rhumatisme 2010 77:617-18.10.1016/j.jbspin.2010.05.00520599412 [Google Scholar] [CrossRef] [PubMed]
[10]. Mustafa KN, Hadidy A, Shoumaf M, Razzuki SA, Polyarthritis with chondronecrosis associated with osteonecrosis, panniculitis and pancreatitisRheumatol Int 2010 30:1239-42.10.1007/s00296-009-1046-919575201 [Google Scholar] [CrossRef] [PubMed]
[11]. Narváez J, Bianchi MM, Santo P, de la Fuente D, Ríos-Rodriguez V, Bolao F, Pancreatitis, panniculitis, and polyarthritisSemin Arthritis Rheum 2010 39(5):417-23.10.1016/j.semarthrit.2008.10.00119070353 [Google Scholar] [CrossRef] [PubMed]
[12]. Harris MD, Bucobo JC, Buscaglia JM, Pancreatitis, panniculitis, polyarthritis syndrome successfully treated with EUS-guided cyst-gastrostomyGastrointest Endosc 2010 72:456-58.10.1016/j.gie.2009.11.04020226449 [Google Scholar] [CrossRef] [PubMed]
[13]. Menon P, Kulshreshta R, Pancreatitis with panniculitis and arthritis: A rare associationPediatr Surg Int 2004 20:161-62.10.1007/s00383-003-1041-214986033 [Google Scholar] [CrossRef] [PubMed]
[14]. Azar L, Chatterjee S, Schils J, Pancreatitis, polyarthritis and panniculitis syndromeJoint Bone Spine 2014 81(2):18410.1016/j.jbspin.2013.08.00324075788 [Google Scholar] [CrossRef] [PubMed]
[15]. Dieker W, Derer J, Henzler T, Schneider A, Rückert F, Wilhelm TJ, Pancreatitis, panniculitis and polyarthritis (PPP-) syndrome caused by post-pancreatitis pseudocyst with mesenteric fistula. Diagnosis and successful surgical treatment. Case report and review of literatureInt J Surg Case Rep 2017 31:170-75.10.1016/j.ijscr.2017.01.03728152495 [Google Scholar] [CrossRef] [PubMed]
[16]. Milani-Nejad N, Johnson GA, Chung GC, Nonpancreatic pancreatic panniculitis: An incidental finding in individuals without pancreatic disease? A case series and review of the literatureJ Clin Aesthet Dermatol 2021 14(4):28-30. [Google Scholar]