Malignancy of breast presenting as cystic lesion is a complex entity to the surgeon and pathologist especially when there is a large cyst at the previous mastectomy site. The incidence of papillary carcinoma is 0.5% of all the invasive carcinomas of the breast. In localised variety, it forms a mass which can be cystic or solid. It can be diffuse with terminal duct lobular units and correspond to papillary variant of Ductal Carcinoma in-situ (papillary DCIS). Here, authors reported an interesting case of a 62-year-old female who presented with large cystic lesion on left breast that after excision was reported as papillary carcinoma of breast. Another patient, 73-year-old also presented with cystic lesion on breast which was diagnosed as papillary carcinoma after excision biopsy. The main fact to be noted here is that approximately half of patients with intracystic carcinoma are associated with underlying ductal carcinoma (in-situ/invasive).
Breast lump, Mastectomy, Postmenopausal women
Case Report
Case 1
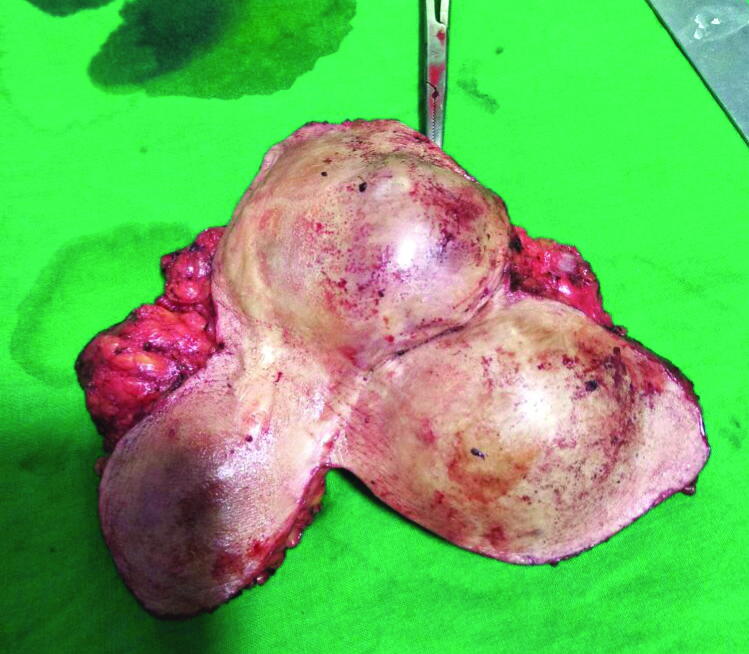
A 62-year-old postmenopausal female presented with multiple swellings on the left chest wall since one year which was progressively increasing in size. She gave history of breast lump excision done seven years back on the same side. Also had recurrence of swelling on the same side and she underwent left breast simple mastectomy five years back. The exact details of the surgery and the previous histopathology reports were not available. On examination, there were three swellings over the left chest wall involving the scar from previous surgery [Table/Fig-1]. The swellings were soft but tense, fluctuant and non transilluminant with restricted mobility. The axillary and supraclavicular lymph nodes were not palpable.
Clinical presentation of three swellings in the left side chest wall with scar from the previous surgery;

Ultrasound showed multiple cystic swellings with few solid components. The Fine Needle Aspiration Cytology (FNAC) showed fluid with suspicious malignant cells. Tru-cut biopsy was attempted but result was inconclusive, the cystic component was predominant. Patient underwent wide excision of tumour after proper workup and informed consent [Table/Fig-2].
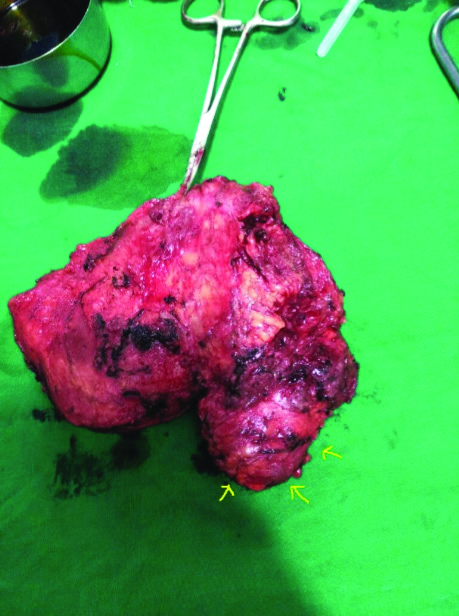
Intraoperative image of wide excision of the tumour;

During excision, the tumour was seen involving some part of pectoralis major muscle which was also shaved off [Table/Fig-3]. Patient later underwent axillary dissection and split skin grafting for the raw area [Table/Fig-4]. The lymph nodes were free of tumour. The patient had an uneventful recovery. The excised tumour in the present case has been shown in [Table/Fig-5]. Histopathology revealed intracystic invasive papillary carcinoma. On sectioning a single cyst, the tumour cells were found arranged in sheets with complex papillary architecture with fibrovascular cores. Individual tumour cells were round to oval to spindle with few showing apocrine changes, moderate pleomorphism with moderate amount of eosinophilic cytoplasm, hyperchromatic nuclei with few prominent nucleoli as shown in [Table/Fig-6].
Resected specimen of tumour with skin and scraped out part of the underlying pectoralis major.
Skin grafting over the excised area.

The excised tumour specimen from case 1. It showed a cystic component (arrow pointing) as well as a solid component (forceps pointing).
Histopathology section of the encysted mass which shows papillary architecture H&E (2X).
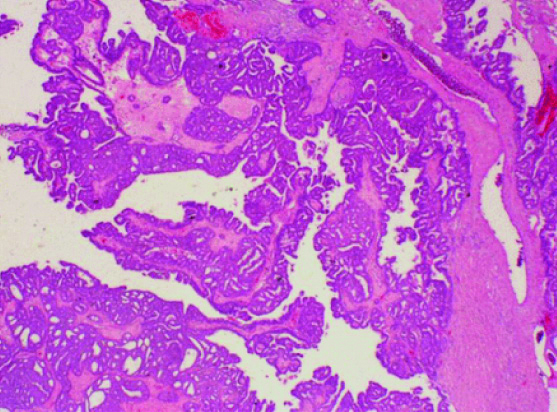
Immunohistochemical (IHC) analysis showed absence of myoepithelial cells surrounding the tumour nodules thereby differentiating it from solid papillary carcinoma or papillary Ductal Carcinoma in-situ (DCIS). All margins of tumour were free from tumour thereby achieving an R0 resection. Hormone receptor studies showed Estrogen Receptor (ER) strongly positive, Progesterone Receptor (PR) strongly positive and C-erb B2 negative. She was advised tamoxifen by Oncologist and reported no recurrence after three years of follow-up.
Case 2
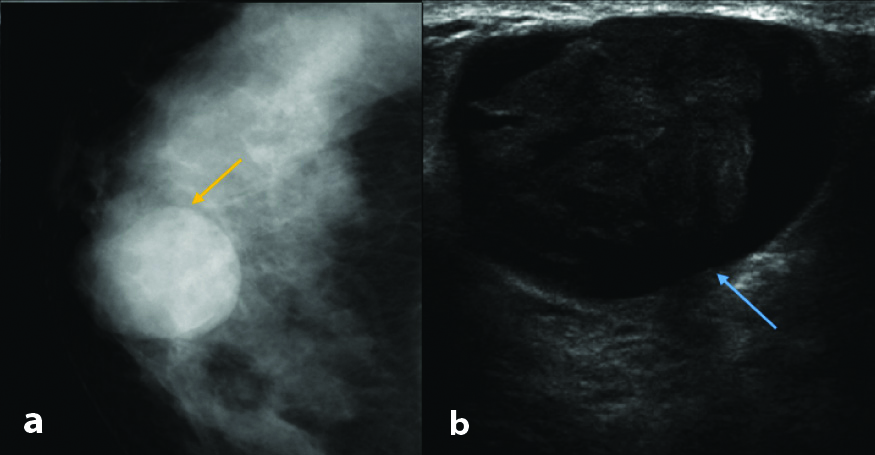
A 73-year-old female presented with lump in the left breast of three months duration. On examination, it was 4x3 cm lump located in upper inner quadrant of breast and variable in consistency on palpation. Mammography and ultrasound showed a cystic lesion with solid component as shown in [Table/Fig-7].
a) Mediolateral oblique view of left breast (left) with yellow arrow pointing to the lesion; b) Ultrasound shows a cystic lesion with few heteroechoic solid component pointed by the blue arrow.
The FNAC was inconclusive as the aspirate was haemorrhagic fluid. In view of lump being well encapsulated and free from skin and chest wall, the patient underwent lumpectomy which confirmed the diagnosis of intracystic papillary carcinoma breast which was invasive variety and all margins were found positive. In view of the elderly age and inner quadrant tumour, there was a higher chance of locoregional and distant spread so patient later underwent modified radical mastectomy. Histopathology showed no residual tumour left and axillary nodes were free of tumour. The IHC confirmed the diagnosis of invasive intracystic papillary carcinoma. Receptor status revealed ER weakly positive, PR weakly positive and HER2/neu negative. Patient was given adjuvant chemotherapy with four cycles of docitaxel and cyclophosphamide and no recurrences reported till now in follow-up.
Discussion
Papillary carcinoma presenting as cystic lesion on the breast is a rare entity and reported rarely in literature. Incidence of papillary carcinoma of breast is about 0.5% [1] of the cases of invasive breast cancers presenting with blood stained nipple discharge, a breast mass, or radiological abnormalities. Papillary carcinoma can be either localised or diffuse [2]. In localised variety it forms a mass which can be cystic or solid. Diffuse variety corresponds to papillary variant of DCIS [3].
The first case of Intracystic Papillary Carcinoma (IPC) was reported in 1969 [4]. In 1983, in a study by Carter D et al., IPC was considered as a form of DCIS in view of its nodular growth, non aggressive behaviour without associated desmoplastic reaction [2]. Nevertheless, it was impossible to highlight the presence of a myoepithelial cell layer by IHC which did question the in-situ nature of the tumour. Solid papillary carcinoma are mostly multinodular predominantly characterised by mucin production and neuroendocrine features. Characteristic feature of papillary DCIS is a peripheral layer of myoepithelial cells [5].
The intracystic variant papillary carcinoma is predominantly found in postmenopausal women between 55 and 67 years old [6]. Many cases were also described in the male population in the literature, and it isthe second most common men’s breast cancer [7].
Mammography findings of intracystic papillary carcinoma appears as a round lobulated opacity, margins well circumscribed with focal areas of inflammation or invasion [4,8]. The differential diagnosis on mammography appearance includes haematoma, invasive ductal carcinoma, colloid or medullary variant of carcinoma, adenofibroma [9]. However, to rule out these differentials a FNAC is often required.
The FNAC is feasible to perform for cytological studies [10]. The aspirated fluid is often haemorrhagic however it is not pathognomonic for IPC. Core needle biopsy is a good tool for diagnosis of IPC, however the histopathology will vary between the centre and periphery of the lesion, hence it cannot distinguish between in-situ and invasive lesions [11]. Excision biopsy can be directly performed when papillary carcinoma is suspected on imaging [12].
Histopathology and IHC helps to classify the papillary lesion and the invasion to surrounding tissues [13]. Immunohistochemical identification of layers of myoepithelial cells helps in distinguishing in-situ from invasive papillary lesions [14]. Invasive carcinoma lacks a myoepithelial call layer in contrast to DCIS [15,16]. The same findings were comparable to the immunohistochemical analysis findings of both the present cases.
On gross examination, IPC appears as a cystic mass with a nodular or a papillary internal surface, with a rounded contour [12]. The excised tumour in case 1 has been shown in [Table/Fig-7].
The IPCs have a good prognosis with adequate local therapy. Many case reports and retrospective studies showed excellent prognosis with conservative surgery without axillary dissection in IPC not associated to DCIS or microinvasion lesions [17-19]. California Cancer Registry (CCR) [20] study is considered the largest series of intracystic papillary carcinoma in theliterature, with a retrospective analysis of over 900 cases of IPC from the years 1988 to 2005. Within the CCR, less than 8% of IPC cases were reported to have lymph node positivity. However, the rate may not be accurate as it was not reported as to what percentage of patients underwent axillary sampling. In the series by Rakha EA et al., 1% was lymph node positive [21]. In both the present cases, lymph nodes were found negative.
A study by Dhebri AR et al., reported three cases of intracystic papillary carcinoma which was managed with mastectomy followed by chemotherapy and hormonal therapy [18]. The data regarding surgical management of IPC is similar to invasive ductal carcinoma, with a lower rate of breast conservation reported in CCR study [20]. However some studies show a paradigm shift towards breast conservation with no significant risk of increase in tumour recurrence or mortality [3,17].
Many studies have reported on the role of adjuvant radiation, chemotherapy and/or hormonal therapy in the management of IPC though the need remains unclear [22-24]. In the study by Solorzano CC et al., it was reported that 30% of the patients hadreceived adjuvant radiotherapy [1]. However radiation did not change the incidence of local recurrence or mortality compared to those who did not receive radiation. Incidence of local recurrence is low and the incidence of distal metastasis or cancer related death is extremely low when compared to those patients with pure DCIS. These patients can be managed like DCIS and not like invasive breast carcinoma. Hormonal therapy can be considered for those who are positive for markers.
As per the CCR [20] there is an observed cumulative survival rate of more than 60% at 10 years and relative survival rate of more than 90% of that of general population at both five and 10 years. It was found that there was no statistically significant difference found in the long term survival of patients between the two histological subgroups of IPC. There is an excellent prognosis for patients diagnosed with IPC regardless of whether the tumour is diagnosed as in-situ or invasive. Comparatively the survival rate of patients with all other types of invasive breast cancer excluding IPC was lower. In 8% of IPC cases discussed in the series by Rakha EA et al., there were recurrences found. Both of our patients have not recorded any recurrences till date [21].
Conclusion(s)
Intracystic papillary carcinoma is a rare breast malignancy, with an excellent prognosis. Although the incidence is low, it is important for the surgeon to know about the natural course of the disease and its various subtypes to decide on an appropriate surgical treatment. Partial mastectomy without axillary lymph node dissection can suffice for non invasive IPC, while total mastectomy (modified radical) with axillary node clearance is required for invasive variants. Multidisciplinary team of the pathologist, radiologist, surgeon and oncologist is particularly useful for the diagnosis and management of this rare, difficult to diagnose, disease.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 22, 2020
Manual Googling: Jul 17, 2021
iThenticate Software: Jul 28, 2021 (12%)
[1]. Solorzano CC, Middleton LP, Hunt KK, Treatment and outcome of patients with intracystic papillary carcinoma of the breastAm J Surg 2002 184(4):364-68.10.1016/S0002-9610(02)00941-8 [Google Scholar] [CrossRef]
[2]. Carter D, Orr SL, Merino MJ, Intracystic papillary carcinoma of the breast. After mastectomy, radiotherapy or excisional biopsy aloneCancer 1983 52(1):14-19.10.1002/1097-0142(19830701)52:1<14::AID-CNCR2820520104>3.0.CO;2-N [Google Scholar] [CrossRef]
[3]. Baykara M, Coskun U, Demirci U, Yildiz R, Benekli M, Cakir A, Intracystic papillary carcinoma of the breast: One of the youngest patient in the literatureMed Oncol 2010 27(4):1427-28.10.1007/s12032-009-9290-019680826 [Google Scholar] [CrossRef] [PubMed]
[4]. Muttarak M, Samwangprasert A, Chaiwun B, Intracystic papillary carcinoma of the breastBiomed Imaging Interv J 2005 1(1):5210.2349/biij.1.1.e521625277 [Google Scholar] [CrossRef] [PubMed]
[5]. Akladios CY, Roedlich MN, Bretz-Grenier MF, Croce S, Mathelin C, Intracystic papillary carcinoma of the breast: A diagnostic challenge with major clinical impactAnticancer Research Journal 2014 34:5017-20. [Google Scholar]
[6]. Salem A, Mrad K, Driss M, Carcinome papillaire mammaire intra kystiqueJournal of Radiology 2009 90:515-18.10.1016/S0221-0363(09)74015-6 [Google Scholar] [CrossRef]
[7]. Levêque J, Watier E, Lesimple T, Goyat F, Grall JY, Intracystic breast carcinoma: A proposed observationJ Gynecol Obstet Biol Reprod 1998 27(3):329-32. [Google Scholar]
[8]. Ravichandran D, Rubin C, Carty NJ, Al-Talib RK, Royle GT, Taylor I, Cystic carcinoma of the breast: A trap for the unwaryAnnals of the Royal College of Surgeons of England 1995 77(2):123-26. [Google Scholar]
[9]. Shin HJ, Kim HH, Kim SM, Yang HR, Sohn JH, Kwon GY, Papillary lesions of the breast diagnosed at percutaneous sonographically guided biopsy: Comparison of sonographic features and biopsy methodsAJR Am J Roentgenol 2008 190(3):930-36.10.2214/AJR.07.266418287432 [Google Scholar] [CrossRef] [PubMed]
[10]. Ohlinger R, Frese H, Schwesinger G, Schimming A, Kohler G, Papillary intracystic carcinoma of the female breast; role of ultrasonogrophyUltraschall Med 2005 26(4):325-28.10.1055/s-2004-81342716123928 [Google Scholar] [CrossRef] [PubMed]
[11]. Tomonori A, Takayuki K, Tadahiko S, Hojo T, Akashi-Tanaka S, Murata Y, Clinical and pathological features of intracystic papillary carcinoma of the breastSurgery Today 2009 39(1):05-08.10.1007/s00595-008-3792-919132460 [Google Scholar] [CrossRef] [PubMed]
[12]. Farrokh D, Abedi M, FallahRastegar Y, An intracystic papillary carcinoma of the breastIran J Cancer Prev 2013 6(2):118-21. [Google Scholar]
[13]. Collins LC, Schnitt SJ, Papillary lesions of the breast: Selected diagnostic and management issuesHistopathology 2008 52(1):20-29.10.1111/j.1365-2559.2007.02898.x18171414 [Google Scholar] [CrossRef] [PubMed]
[14]. Hill CB, Yeh IT, Myoepithelial cell staining patterns of papillary breast lesions: From intraductal papillomas to invasive papillary carcinomasAmerican Journal of Clinical Pathology 2005 123(1):36-44.10.1309/XG7TPQ16DMJAV8P115762278 [Google Scholar] [CrossRef] [PubMed]
[15]. Collins LC, Carlo VP, Hwang H, Intracystic papillary carcinomas of the breast: A re-evaluation using a panel of myoepithelial cell markersAm J Surg Pathol 2006 30:1002-07.10.1097/00000478-200608000-0001116861972 [Google Scholar] [CrossRef] [PubMed]
[16]. Ilhan E, Üreyen O, Şenlikci A, Yağcı A, Yeldan E, Salman T, Intracystic carcinoma of the breast: report of two casesJ Breast Health 2015 11(1):45-47.10.5152/tjbh.2014.200628331690 [Google Scholar] [CrossRef] [PubMed]
[17]. Fayanju OM, Ritter J, Gillanders WE, Therapeutic management of intracystic papillary carcinoma of the breast: The roles of radiation and endocrineAm J Surg 2007 194(4):497-500.10.1016/j.amjsurg.2007.06.01617826064 [Google Scholar] [CrossRef] [PubMed]
[18]. Dhebri AR, Ahmad A, Shah N, Arora PK, Intracystic papillary carcinoma of breast: Report of three cases and review of the literatureBMJ Case Reports 2012 10:113610.1136/bcr-2012-00723723188855 [Google Scholar] [CrossRef] [PubMed]
[19]. Zheng YZ, Hu X, Shao ZM, Clinicopathological characteristics and survival outcomes in invasive papillary carcinoma of the breast: A SEER population-based studySci Rep 2016 6:2403710.1038/srep24037 [Google Scholar] [CrossRef]
[20]. Grabowski J, Salzstein SL, Sadler GR, Blair S, Intracystic papillary carcinoma: A review of 917 casesCancer 2008 113(5):916-20.10.1002/cncr.2372318661510 [Google Scholar] [CrossRef] [PubMed]
[21]. Rakha EA, Gandhi N, Climent F, Encapsulated papillary carcinoma of the breast: An invasive tumor with excellent prognosisAm J Surg Pathol 2011 35:1093-103.10.1097/PAS.0b013e31821b3f6521753694 [Google Scholar] [CrossRef] [PubMed]
[22]. Mugler K, Marshal C, Hardesty L, Intracystic papillary carcinoma of the breast: Differential diagnosis and managementOncology 2007 21:871-76. [Google Scholar]
[23]. Hassan Z, Boulos F, Abbas J, Intracystic papillary carcinoma: Clinical presentation, patterns of practice, and oncological outcomesBreast Cancer Res Treat 2020 182:317-23.10.1007/s10549-020-05680-932462260 [Google Scholar] [CrossRef] [PubMed]
[24]. Fakhreddine MH, Haque W, Ahmed A, Schwartz MR, Farach AM, Paulino AC, Prognostic factors, treatment, and outcomes in early stage, invasive papillary breast cancerAm J Clin Oncol 2018 41(6):532-37.10.1097/COC.000000000000033527819878 [Google Scholar] [CrossRef] [PubMed]