Case Report
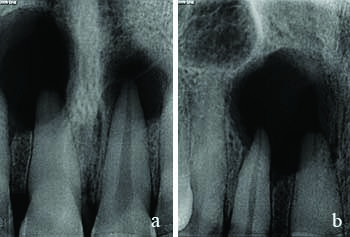
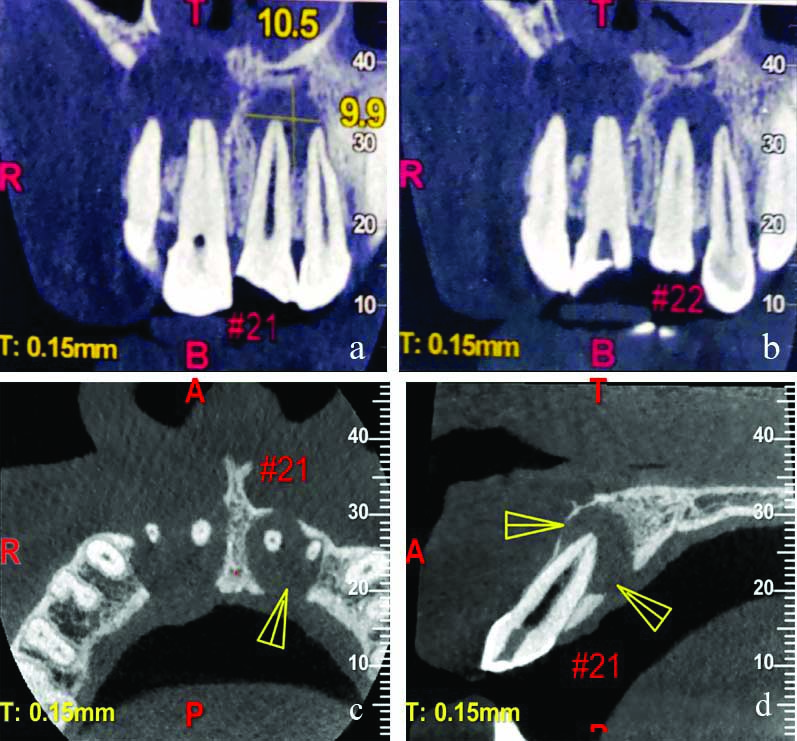
A 30-year-old male patient reported to the Department of Conservative Dentistry and Endodontics with the chief complaint of painless swelling over the palate in the front region since one month and fractured tooth in upper front region. History revealed an incidence of fall from a flight of stairs face down five years back. Due to the absence of any symptoms at the time of fall and aesthetics not being his primary concern he did not seek any dental guidance. The swelling was first noticed about a year ago with a continuing gradual increase in size. He gave no complaints of pain or paresthesia, however, stated that there had been a sudden increase in size and tenderness of the swelling over the past few days. Extra oral examination showed no presence of an extra oral distention of tissue or swelling, also there was no visible or palpable lymphadenopathy. Intra oral examination revealed a well defined tender swelling on right side of anterior palate, crossing over the midline to the left side and an Ellis class III fracture with 21 (maxillary left central incisor) and not associated with pain. Electric pulp testing revealed 11, 12, 21, and 22 (maxillary incisors) to be non vital. Also, the patient complained at times of altered taste in mouth and burning sensation. Intra Oral Periapical Radiograph (IOPA) radiograph revealed well defined round radiolucencies associated with 11, 12 and 21, 22 [Table/Fig-1a,b]. Heat tests and Electric Pulp vitality Tests (EPT) illustrated no response in relation to 11, 12 and 21, 22; whereas 13, 23 (maxillary canines) had a positive vitality response.
Well defined radiolucency in the periapical region of maxillary incisors.
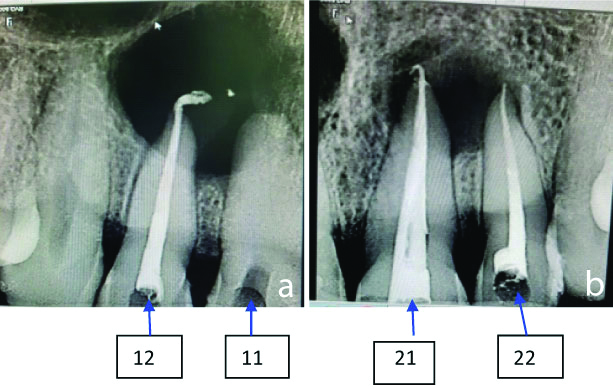
For more accurate understanding of the actual extension of the intra oral lesion, the area of interest was subjected to Cone Beam Computed Tomography (CBCT) examination and the findings were as follows:
Evaluation of maxillary right incisors
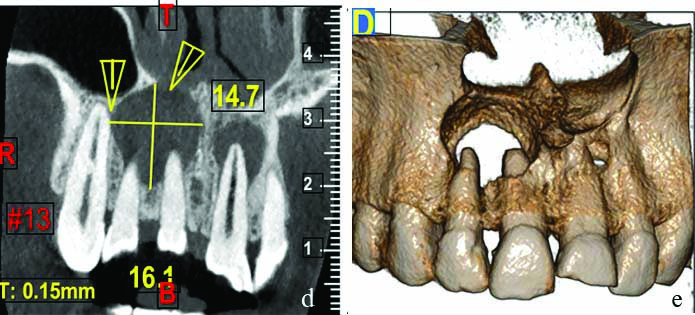
A well-defined partially corticated radiolucency was seen in the periapical region of 11 and 12. Internal structure of the lesion was completely radiolucent. The lesion had caused a breach in the floor of nasal cavity and involvement of inferior conchae was noted. It was in close anatomical proximity to the nasopalatine nerve canal and anterior wall of the maxillary sinus. Epicentre of the lesion was seen with respect to 11 [Table/Fig-2a-b,c,d-e].
Well defined radiolucency in the periapical region of 11 and 12, along with breach in the floor of nasal cavity and involvement of inferior conchae with respect to 11 and 12 can be appreciated.
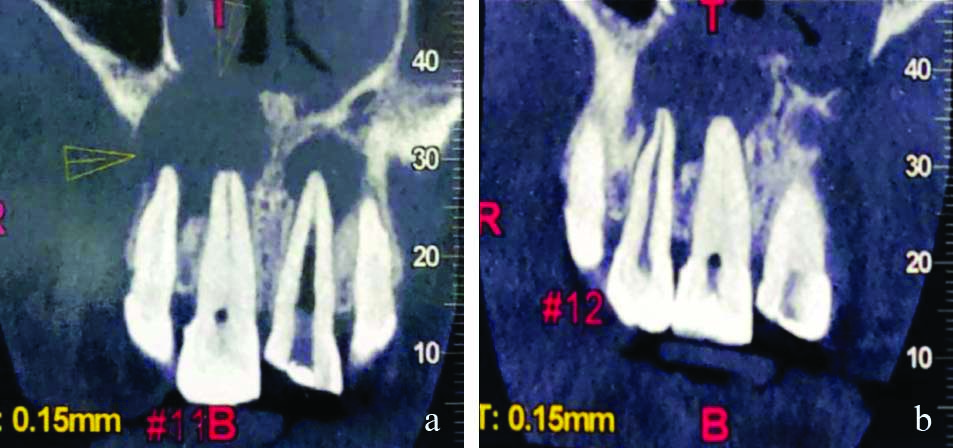
Anterioposterior extent: The lesion anteroposteriorly was seen extending from the buccal cortical plate to the palatal cortical plate till the mesial aspect of 13. Breach in continuity of both buccal and palatal cortex was noted with respect to 11, 12 and 13.
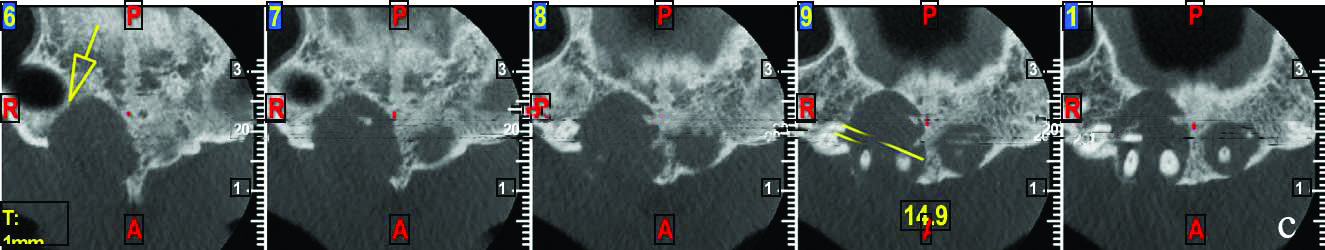
d) SuperoInferior extent: The lesion was seen involving the floor of the nasal cavity extending to the apical two third of roots of 11, 12 and 13. The size of lesion measured in the superoinferior extent was 14.7 mm; e) Mesiodistal extent: Mesiodistally the lesion was seen extending from mesial aspect of 11 to the mesial aspect of 13. The size of lesion measured in the mesiodistal extent was 14.9 mm.
Evaluation of maxillary left incisors
Another well defined, partially corticated radiolucency was seen in the periapical region of 21 and 22. The floor of the nasal cavity was intact. The lesion was in close proximity to the nasopalatine nerve canal. Epicentre of the lesion was seen with respect to 21 [Table/Fig-3a-d].
a) Superior-inferior extent: The lesion was seen extending from below the floor of the nasal cavity to involve apical third of 21 and 22. The lesion measured 10.5 mm in the supero-inferior extent. Mesiodistally: the lesion was seen extending from the mesial aspect of 21 to the mesial aspect of 22. The lesion measured 9.9 mm in the mesio-distal extent; c) and d) Anterioposterior extent: The lesion was seen extending anteroposteriorly from the buccal cortical plate to palatal cortical plate. The lesion measured 9.3 mm in the anteroposterior extent. Breach in the palatal cortex was noted with respect to 22 and severely thinned out buccal cortex was evident for 21 and 22.
Based on the chief complaint, clinical and radiographical examination, pulp vitality test and owing to the size of the lesion appreciated in radiographic picture both orthograde and retrograde management of the lesion was decided. A provisional diagnosis of infected periapical cyst was made. But final diagnosis was to be confirmed on completion of histopathological finding.
The treatment plan was routine endodontic therapy, followed by surgical intervention, the procedure was explained to the patient and an informed consent was obtained for the same. The treatment was scheduled into two phases:
1) Endodontic phase
2) Surgical phase
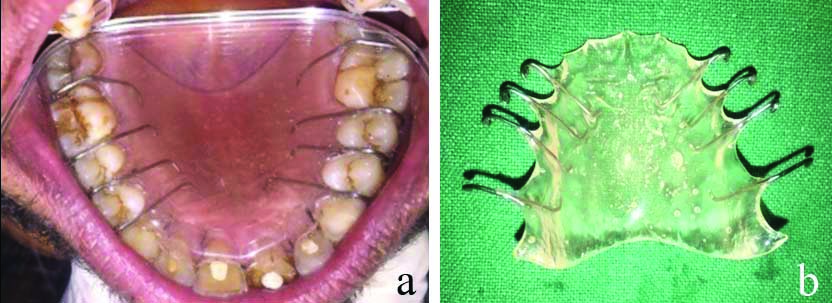
1) Endodontic phase [Table/Fig-4a,b]
Endodontic treatment was done with 12, 21 and 22.
Local anaesthesia (2% lidocaine containing 1:100000 epinephrine) was administered and a root canal access opening of 11, 12, 21 and 22 under rubber dam isolation was done. The canals of 12, 21 and 22 were located. Working length was determined using an apex locator (J.Morita Root ZX II) and also confirmed radiographically. Complete biomechanical preparation was done for 12, 21 and 22 using Universal Protaper rotary shaping files (Dentsply) in a crown-down manner upto size F2 protaper. Standard irrigation protocol was followed during the entire course of biomechanical preparation. The canals were dried using paper points (Dentsply) and a dressing of calcium hydroxide (RC Cal-Prime dental products) medication was given for 21 days to the patient. The patient was recalled after three weeks. During the recall visit calcium hydroxide medicament was removed, canals were irrigated with normal saline and dried using paper points (Dentsply). Obturation was done by lateral condensation technique using corresponding sized gutta-percha 6% (Dentsply) along with AH Plus (Dentsply) as the sealer and the access cavity was sealed with temporary restorative material (Cavit G).
However, while treating 11, the canal could not be negotiated and was calcified which was also confirmed by CBCT, therefore the access cavity was filled with tooth coloured restorative material. (Z-350 Composite Restorative Material).
2) Surgical Phase
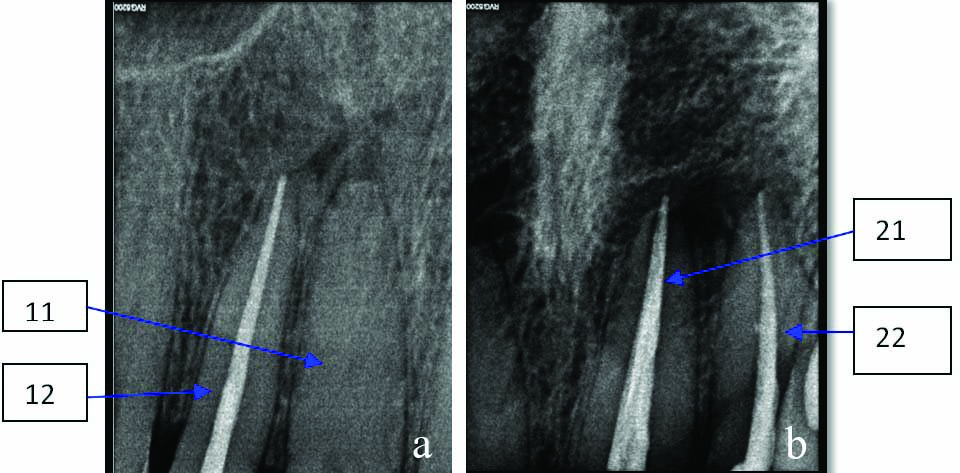
The surgical intervention was carried out under local anaesthesia. An infraorbital block along with palatal infiltration using 2% lidocaine containing 1:100000 epinephrine was given. Crevicular incision was made using a Bard Parker blade (BP) (No. 12) extending from left maxillary premolar to right maxillary premolar on the labial aspect. A full thickness mucoperiosteal flap was raised [Table/Fig-5] and reflection of the flap was carried out to expose healthy bony margins apical to the defects in 11, 12, 21 and 22 regions. Two separate bony defects were identified. Sharp dissection was carried out using BP blade (No.15) as the cystic lining had merged with the periosteum on both the labial and palatal aspect with respect to 11 and 12. Cystic lining was curetted out using a double ended Molt’s curette (Premier dental, USA) and irrigated using normal saline. Also, complete enucleation of the cystic lesion with respect to 21 and 22 was carried out [Table/Fig-6]. Apicoectomy was performed for 11, 12, 21, and 22. Flap closure was done using 3-0 silk sutures (Ethicon) [Table/Fig-7]. The enucleated cystic lesion specimen was fixed in 10% formalin and send for further histopathological examination. Hawley’s retainer was given to support the palatal mucoperiosteum [Table/Fig-8a,b]. The patient was asked to follow a soft diet for seven days and was prescribed a course of antibiotics. Amoxicillin in combination with clavulanic acid (Augmentin Duo 625 mg) was prescribed twice a day for five days and an Non steroidal Anti-inflammatory Drugs (NSAIDs) with serratiopeptidase combination (Tab. Enzoflam) was given twice a day for five days. Also an antacid pantaprazole (Tab. Pan 40 mg) was given twice a day. Betadine rinses for oral hygiene maintenance along with other postoperative instructions were explained to the patient.
Crevicular incision continuous in nature was placed on labial aspect extending from left maxillary premolar to right maxillary premolar to reflect full thickness mucoperiosteal flap that exposed a wide labial bone defect.

Cyst lining was excavated along with its content followed by thorough curettage and irrigation.

Flap closure was done using 3-0 silk suture.

After enucleation of cyst, patient had been given a Hawley’s Retainer.
After a week, the patient was recalled for the removal of sutures. Patient was kept under follow-up for one year. On a one-year follow-up radiographically the periapical lesion that presented as a well circumscribed radiolucency had reduced in size drastically and a trabaecular pattern suggestive of osteogenesis could be appreciated [Table/Fig-9a,b]. Clinically, there was no swelling with a presentation of healthy palatal mucosa.
Histopathological report [Table/Fig-10a-e]
The connective tissue was dense and fibrous, composed of collagen fibre bundles interspersed with fibroblast. Abundant neurovascular bundles were seen scattered throughout the stroma under 40X magnification (a) and 100X magnification (b) respectively. Chronic inflammatory cell infiltrate, chiefly lymphocytes and a few plasma cells were also evident; c) Abundant capillaries and engorged blood vessels are noted (40X Magnification) (H&E staining); d) Connective tissue devoid of epithelium (40X Magnification) (H&E staining); e) Bony tissue with osteocytic lacunae was present throughout the connective tissue stroma (100x Magnification) (H&E staining).
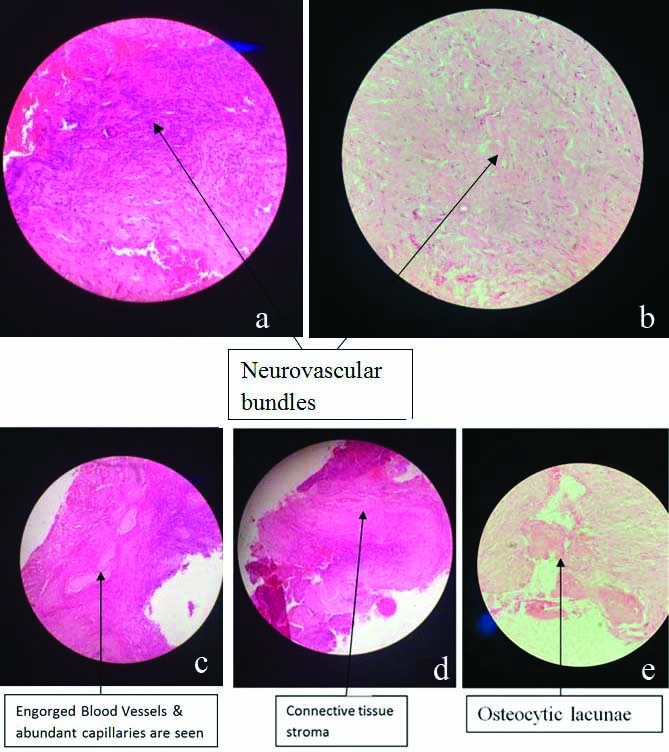
On histopathological evaluation, the specimen was devoid of epithelium. The connective tissue was dense and fibrous, composed of collagen fibre bundles interspersed with fibroblast. Abundant neurovascular bundles were seen scattered throughout the stroma. Chronic inflammatory cell infiltrate, chiefly lymphocytes and a few plasma cells were evident. Also, numerous capillaries and engorged blood vessels with extravasated Red Blood Corpuscles (RBC’S) were noted.
Bony tissue with osteocytic lacunae was present throughout the connective tissue stroma. Deeper connective tissue showed longitudinal section of muscles at some areas. The overall picture was found to be suggestive of Nasopalatine Duct Cyst (NPDC).
Discussion
The NPDC is one of the most common developmental, non neoplastic, non odontogenic cysts of the oral cavity, occurring in about 1% of population. Nasopalatine Duct Cyst (NPDC) is unique in that it develops in only single location which is midline of the palate [1].
The aetiology of these lesions is not clear; in addition to the hypothesis of spontaneous proliferation from embryonic tissue remains, other possible aetiologies have been proposed–including trauma, poorly fitting dentures, the existence of local infection, or the influence of genetic and racial factors and mucous retention within associated salivary gland [2,3]. The NPDC can form within the incisive canal which is located in the palatine bone and behind the alveolar process of the maxillary central incisors or in the soft tissue of the palate that overlies the foramen, called the cyst of the incisive papilla [4]. In the reported case there was history of trauma, therefore it is a probability that the cyst developed as a result of trauma.
The NPDCs have previously been reported to occur centrally or unilaterally [5]. It is rare for an NPDC to present bilaterally making our case unique and clinically significant. In a study conducted by Shear M et al., out of 404 NPDC cases only one patient developed cysts in both Stensons canal [6].
These lesions have shown a predilection of presenting between the fourth and sixth decades of life, though some cases of NPDC have been found in paediatric patients up to 8 years of age [4].
Common clinical presentation is the presence of a fluctuant swelling in the anterior part of the palate, pain in a few case and intermittent discharge of straw coloured fluid (mucoid in nature) exudates imparting a salty taste to the mouth. Sometimes due to compression of the nasopalatine nerve, patient may experience burning sensation and numbness. Displacement of teeth is a rare finding [7]. Similarly the patient presented with a well defined tender swelling in the midline of the anterior palate and also experienced a burning sensation and bad taste in the mouth.
Radiographically, it appears as a round, ovoid or heart shaped radiolucency between the roots of central incisors [8]. In some cases, a prominent incisive canal can present as a radiolucent area and imitate NPDC. When considering the size of a lesion if it exceeds 6mm in size it should be suspected to be potentially pathogenic in nature and warrant further investigation [4,7,9,10]. Lesions that are aymptomatic and are less that 6 mm in size are considered as enlarged incisor ducts of a non pathological nature [9].
A 3D radiographic exploration is essential for diagnosing NPDC. In addition to conventional 2 dimensional IOPA, other advanced radiographic techniques are recommended such as panoramic X-rays, occlusal radiographs and CBCT [11].
The main advantages of CBCT imaging are, that it offers real size data base sheet and a 3D reconstruction (supero-inferior, anterio-posteriorly and mesiodistal dimensions of the lesion), which are based on a single scan of low radiation dose [11]. In the present case, CBCT helped us to diagnose the erosion of the nasal floor at the superior extent and erosion of the bony vault of the palate at inferior extent of the lesion. Also, 11 showed a calcified canal therefore root canal treatment was not attempted.
The differential diagnosis should be established with odontogenic cyst {e.g., lateral radicular cyst, lateral periodontal cyst, odontogenic keratocyst (OKC)}, odontogenic tumour (e.g., ameloblastoma, odontogenic myxoma) and non odontogenic tumours (e.g., central giant cell tumour, brown tumour of hyperparathyroidism, central haemangioma) [4]. Due to similar signs and symptoms, the NPDC may be misdiagnosed as a periapical cyst. Incisor teeth that are in close proximity or associated with the cystic cavity are always checked for vitality. NPDC present with teeth that are vital and show intact lamina dura, whereas non vital teeth with loss of continuity of lamina dura could be suggestive of a radicular cyst [5]. In the present case report the lesion involved the apical third of the roots and since the vitality test was negative, that led to an initial misdiagnosis as a periapical cyst.
In our case, 11, 12, 21, 22 showed a negative response to vitality test; whereas 13, 23 which also were approximating the cyst showed a positive vitality response. Hence, endodontic treatment was planned for only pulpless teeth.
Majority of the NPDCs cases (71.8%) have squamous, columnar, cuboidal or some combination of these epithelial types; whereas 9.8% cases showed presence of respiratory epithelium [8]. Histopathological examination of this case revealed a cavity devoid of epithelium and surrounded by connective tissue wall. The cyst wall contains a chronic inflammatory reaction consisting of lymphocytes and few plasma cells. The presence of neurovascular bundles and adipose tissue also confirm diagnosis of NPDC [4,8].
While deciding the most pertinent treatment protocol to be followed when treating a NPDC lesion, a multitude of probabilities could be considered. NPDC is generally treated by surgical excision. Marsupialisation is indicated for treatment of very large cysts [12-14]. Enucleation of the NPDC followed by consequent coverage of the defect, a conservative approach for certain cases and or chemical ablation can also be considered [15]. Failure to remove the cyst can lead to acute infection, followed by perforation of the bone and development of a fistulous tract [16]. Paresthesia on the anterior palate has been observed in less than 10% of the NPDCs treated by surgical excision, as components of the long sphenopalatine nerve may also be removed [17]. In the majority of the cases, the prognosis is good and complete bone regeneration occurs in a high percentage of cases [18]. The treatment of choice in the present case was surgical excision but care was exercised while performing the surgery because neurovascular bundles are a delicate and highly vascularised structure giving rise to profuse bleeding if inadvertently sectioned during surgery. Electrocoagulation might be required in such cases [19].
The NPDC has shown a predilection in giving rise to squamous cell carcinomas which commonly occur in the anterior part of the maxilla. Squamous cell carcinomas are said to originate from the metaplasia of epithelial cells lining a cystic cavity or from the epithelial remnants that participate in odontogenesis [19]. As NPDC shows a high recurrence rate close to 30% a regular follow-up and or any signs of carcinoma development should be noted and acted on immediately [2].
Therefore, cystic lesions of the maxillae require comprehensive study and precise treatment and histological diagnosis, since some of them may be aggressive and incorrect diagnosis and treatment can give rise to recurrences.
Conclusion(s)
Nasopalatine Duct Cyst (NPDC) are the most common type of non odontogenic cyst that present as radiolucencies occurring in the anterior part of the maxilla. This case report attempts to emphasise the need for a comprehensive clinical and radiographic examination of a lesion to identify the pathology like NPDC that can be easily be misdiagnosed as a periapical cyst. NPDC require prompt treatment protocol as they show a high recurrence rate and show a tendency of developing into a squamous cell carcinoma that can be life threatening. In our case, a provisional diagnosis of periapical cyst was proposed and teeth were treated based on their vitality along with surgical management of the cyst was carried out. The final diagnosis of the lesion being an NPDC was determined only after the full histopathological analysis of the pathology was conducted.
[1]. Robertson H, Palacios E, Nasopalatine duct cystEar Nose Throat J 2004 83(5):31310.1177/014556130408300505 [Google Scholar] [CrossRef]
[2]. Yih WY, Krump JL, Odontogenic keratocyst in the nasopalatine duct associated with mural cartilaginous metaplasiaJ Oral Maxillofac Surg 2005 63(9):1382-84.10.1016/j.joms.2005.05.30516122607 [Google Scholar] [CrossRef] [PubMed]
[3]. Allard RH, Van der Kwast WA, Van der Waal I, Nasopalatine duct cyst. Review of the literature and report of 22 casesInt J Oral Surg 1981 10(6):447-61.10.1016/S0300-9785(81)80081-6 [Google Scholar] [CrossRef]
[4]. Shylaja S, Balaji K, Krishna A, Nasopalatine duct cyst: Report of a case with review of literatureIndian J Otolaryngol Head Neck Surg 2013 65(4):385-88.10.1007/s12070-011-0242-624427606 [Google Scholar] [CrossRef] [PubMed]
[5]. Cicciù M, Grossi GB, Borgonovo A, Santoro G, Pallotti F, Maiorana C, Rare bilateral nasopalatine duct cysts: A case reportOpen Dent J 2010 4:08-12.10.2174/187421060100401000820386720 [Google Scholar] [CrossRef] [PubMed]
[6]. Shear M, Speight PM, Cysts of the Oral and Maxillofacial Regions 2007 4th editionOxford, UKBlackwell Munksgaard10.1002/9780470759769 [Google Scholar] [CrossRef]
[7]. Elliott KA, Franzese CB, Pitman KT, Diagnosis and surgical management of nasopalatine duct cystsLaryngoscope 2004 114(8):1336-40.10.1097/00005537-200408000-0000415280704 [Google Scholar] [CrossRef] [PubMed]
[8]. Francoli JS, Marques NA, Aytis LB, Escoda CG, Nasopalatine duct: report of 22 cases and review of literatureMed Oral Patol Oral Cir Bucal 2008 13(7):438-43. [Google Scholar]
[9]. Vasconcelos R, De Aguiar MF, Castro W, De Araújo VC, Mesquita R, Retrospective analysis of 31 cases of nasopalatine duct cystOraL Dis 1999 5(4):325-28.10.1111/j.1601-0825.1999.tb00098.x10561722 [Google Scholar] [CrossRef] [PubMed]
[10]. Swanson KS, Kaugars GE, Gunsolley JC, Nasopalatine duct cyst: An analysis of 334 casesJ Oral Maxillofac Surg 1991 49:268-71.10.1016/0278-2391(91)90217-A [Google Scholar] [CrossRef]
[11]. Prabhusankar K, Yuvaraj A, Prakash CA, Parthiban J, Praveen B, CBCT cyst lesions diagnosis imaging mandible maxillaJ Clin Diagn Res. JCDR 2014 8(4):ZD03-05.10.7860/JCDR/2014/7547.422824959518 [Google Scholar] [CrossRef] [PubMed]
[12]. Saunders LA, Wisniewski H, Soumeral S, Extensive incisive canal cystOral Surg Oral Med Oral Pathol 1968 26:284-90.10.1016/0030-4220(68)90396-4 [Google Scholar] [CrossRef]
[13]. Schiff BS, Kringstein G, Stoopack JC, An extremely large and facially distorting nasopalatine duct cystOral Surg Oral Med Oral Pathol 1969 27:590-94.10.1016/0030-4220(69)90088-7 [Google Scholar] [CrossRef]
[14]. Tainter JF, Fahid A, Case report: Median palatine cystDent Surg 1977 53:33-36. [Google Scholar]
[15]. Werder P, Bassetti R, Kuttenberger J, Surgical treatment option of the patent nasopalatine duct: A case reportJ Surg Case Rep 2016 2016(5):rjw09010.1093/jscr/rjw09027197612 [Google Scholar] [CrossRef] [PubMed]
[16]. Schott TR, Correll RW, Wescott WB, Well-defined radiolucent area involving the anterior maxillaJ Am Dent Assoc 1985 110:86-88.10.14219/jada.archive.1985.03103855924 [Google Scholar] [CrossRef] [PubMed]
[17]. Bodin I, Isacsson G, Julin P, Cysts of the nasopalatine ductInt J Oral Maxillofac Surg 1986 15:696-99.10.1016/S0300-9785(86)80110-7 [Google Scholar] [CrossRef]
[18]. Hedin M, Klamfeldt A, Persson G, Surgical treatment of nasopalatine duct cysts: A follow-up studyInt J Oral Surg 1978 7:427-33.10.1016/S0300-9785(78)80033-7 [Google Scholar] [CrossRef]
[19]. Takagi R, Ohashi Y, Suzuki M, Squamous cell carcinoma in the maxilla probably originating from Nasopalatine duct cyst: Report of caseJ Oral Maxillofac Surg 1996 54(1):112-15.10.1016/S0278-2391(96)90318-3 [Google Scholar] [CrossRef]