Introduction
Definition and Phenotypes
The PCOS is a multifactorial endocrine disorder whose pathophysiology baffles many researchers and clinicians till today. It affects 5-20% of the women of reproductive age group [1]. This syndrome is typically characterised by dysregulated ovulatory cycles and infertility, altered gonadotropin levels, obesity, and bulky multifollicular ovaries on ultrasound. The hallmark features of this complex pathophysiological condition include menstrual dysfunction, hirsutism, infertility, obesity and metabolic syndrome [2,3]. Elevated levels of androgen in PCOS subject population usually leads to subcellular aberrations in theca cells which also brings an imbalance in the levels of serum Anti-Mullerian Hormone (AMH) in comparison to healthy women [4]. Despite being the most common endocrine disorders affecting women, the diagnosis, management, and associated long-term health risks of PCOS remain controversial. In the present literature review, authors have briefly summarised the multifaceted nature of PCOS which still defies proper understanding. Given the importance of uncharacteristic aetiology of PCOS, the review also focuses on the Genome Wide Association Studies (GWAS) and how the scientific community is still in search of novel gene signatures or biomarkers for the diagnosis of PCOS.
The PCOS is a complex disease and this multifactorial syndrome can be grouped into four phenotypes:
a) Phenotype A is characterised with numerous polycystic ovaries, oligo anovulation (self-reported menstrual cycle length of 35 days or <10 menstrual period per year), and hyperandrogenism (high levels of androgens).
b) Phenotype B is characterised with normal appearance of ovaries, oligo anovulation, and hyperandrogenism.
c) Phenotype C characterised with polycystic ovaries with normal routine menses and hyperandrogenism.
d) Phenotype D characterised with polycystic ovaries, oligo anovulation, without hyperandrogenism.
Phenotype A and B are known to be classic PCOS. Women with these phenotypes present with significant menstrual dysfunction, insulin resistance, and increased risk of metabolic syndrome and elevated levels of Antimullerian Hormone (AMH). When compared to other phenotypes, incidence of obesity is higher in classic PCOS [5,6]. Phenotype C also known as the ovulatory PCOS is characterised by elevated insulin, androgens and higher hirsutism scores [7]. Phenotype D is otherwise called non hyper androgenic PCOS because of the normal androgen levels with very low chances of metabolic dysfunction. Usually women with phenotype D has regular menstrual cycles however they have low levels of Triiodothyronine (T3) and Tetraiodothyronine (T4) as well as lower Luteinising Hormone/Follicle Stimulating Hormone (LH/FSH) ratio when compared to the women with classic PCOS [8,9]. It is important to note that all the phenotypes of PCOS can be detected by ultrasound.
Criteria for the Diagnosis of PCOS
Given the multifactorial nature of the disease, there is an uncertainty surrounding the criteria for diagnosis, management of patients, and long term health risks for PCOS subjects. Since the evidences suggest that women with PCOS are at increased risk of infertility, dysfunctional uterine bleeding, metabolic syndrome, type II diabetes, and cardiovascular disease [10,11], it is important to strategise early diagnosis and intervention. There is also growing evidence that women with PCOS are at increased risk of obstructive sleep apnoea, depression, non alcoholic fatty liver disease, and certain cancers [12-14].
The first attempt to define PCOS clinically was initiated by the National Institute of Child Health and Human Development (NICHD) in 1990, which defined PCOS as combined presence of androgen excess and oligo anovulation excluding all other aetiologies of anovulatory infertility. Ultrasonographic evidence was considered to be suggestive but not necessarily diagnostic for PCOS [15]. But this was not accepted by the clinicians from the United Kingdom (UK) and most of Europe because USG evidence of polycystic ovaries had long been considered as definitive evidence of PCOS [16]. Although the NICHD criteria helped in putting forward an important step in establishing a universally acceptable clinical definition for PCOS, but in the years that followed, it became clear that the clinical presentation of PCOS deviated drastically than defined by NICHD and notably women demonstrating biochemical evidence of the syndrome had a consistent morphology of polycystic ovaries [17-19].
After a decade, the European Society for Human Reproduction and Embryology and the American Society for Reproductive Medicine (ESHRE and ASRM or Rotterdam) changed the criteria and included polycystic ovaries as a third diagnostic marker which allowed to redefine PCOS as a syndrome of ovarian dysfunction [20]. The Rotterdam criteria required two of the three criteria for a diagnosis of PCOS which implied that PCOS can even be diagnosed without androgen excess or even irregular menstrual cycles. This made Rotterdam criteria disputable as the above parameters forms the basis of the syndrome.
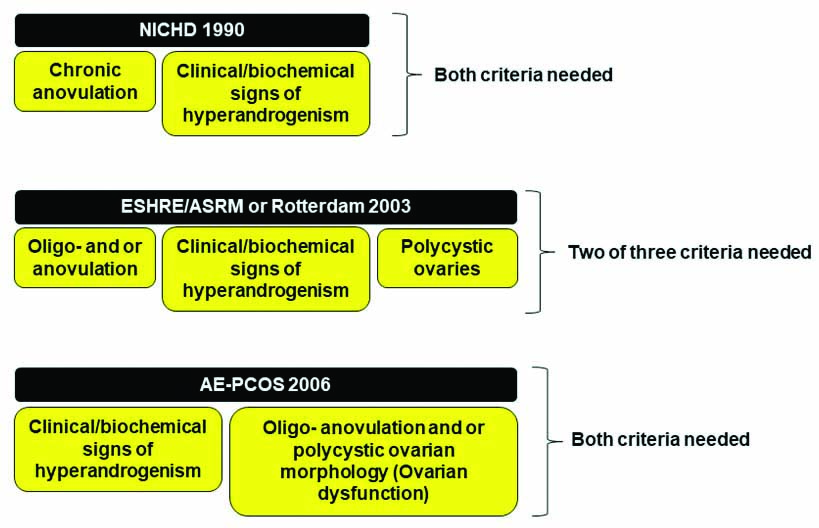
In 2006, a new task force was formed by the Androgen Excess Society (AE-PCOS) to scrutinise the existing data on the phenotypic expression of PCOS. After thorough consideration the society proposed a new set of diagnostic criteria including clinical and or biochemical signs of hyperandrogenism and widely prevalent ovarian dysfunction [21]. The proposed diagnostic criteria and their requisites are summarised in [Table/Fig-1].
Accepted diagnostic criteria for PCOS and their requisites.
NICHD: National institute of child health and human development; ESHRE: European society for human reproduction and embryology; ASRM: American society for reproductive medicine
Incidence and Prevalence
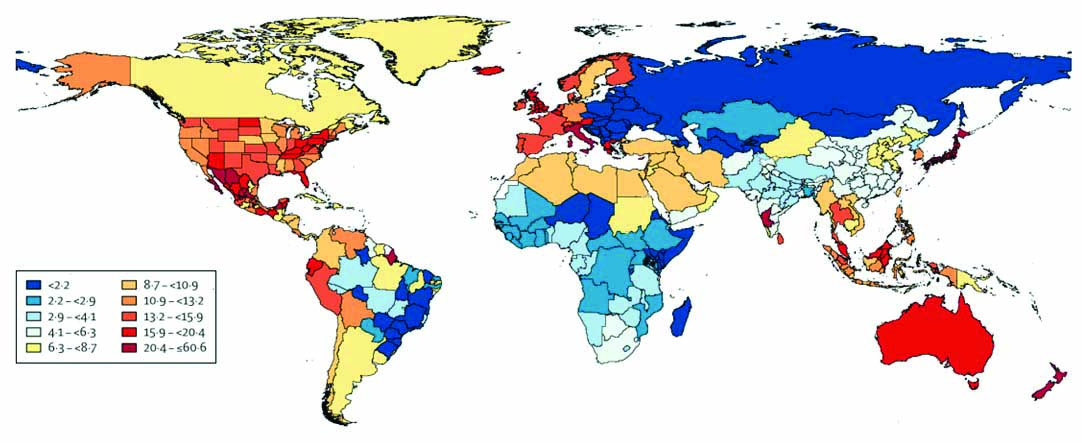
The diagnosis of PCOS is mainly done by the criteria set by one of the three diagnostic criteria: The NICHD or the Rotterdam or the ones set by AE-PCOS society. The estimation of the prevalence of this syndrome depends on which criteria were followed whether individually or combined. The prevalence of PCOS was estimated for the first time in 1998 amongst the different populations of Caucasian and black races, and it was estimated to be around 4% in both the races [22]. In another study, which was done much later in 2017 involving a total of 400 women with age range of 18-45 years it was estimated to be 6.6% in both black and white populations [23] which was well supported by another Spanish study that estimated the prevalence to be 6.8% [24]. In a study conducted at Oxford University and a private medical centre, a 6.8% prevalence of PCOS was estimated [25]. In 2013, a study conducted in Chinese women indicated the prevalence of PCOS as 5.6% [26]. The prevalence of PCOS seems to be significantly higher in the South Asian countries like India and Pakistan. Various studies from India have reported the prevalence of PCOS in the range of 3-35% [27-31] whereas the studies from Pakistan reported a higher prevalence of 40-50% among the woman of reproductive age group [32,33]. The Institute for Health Metrics and Evaluation has provided the latest prevalence rates of PCOS throughout the globe (http://www.healthdata.org/results/gbd_summaries/2019/polycystic-ovarian-syndrome-level-4-cause) and the same has been depicted in [Table/Fig-2].
Age standardised DALY (disability-adjusted life years) of PCOS per 100,000 population worldwide. The color coding chart depicts the percentage of PCOS prevalence in different locations with blue being the lowest and red being the highest.
PCOS and Gestational Complications
During the second and third trimesters of the normal pregnancy, the body induces insulin resistance as a compensatory mechanism designed to restrict maternal glucose uptake thereby ensuring the growing foetus gets enough nutrients [34]. Insulin resistance along with hyperandrogenism forms the metabolic hallmark of PCOS women which increases the risk of pregnancy complications in such women. They are at increased risk of Early Pregnancy Loss (EPL), Gestational Diabetes Mellitus (GDM), Hypertensive Disorders of Pregnancy (HDP), and premature delivery.
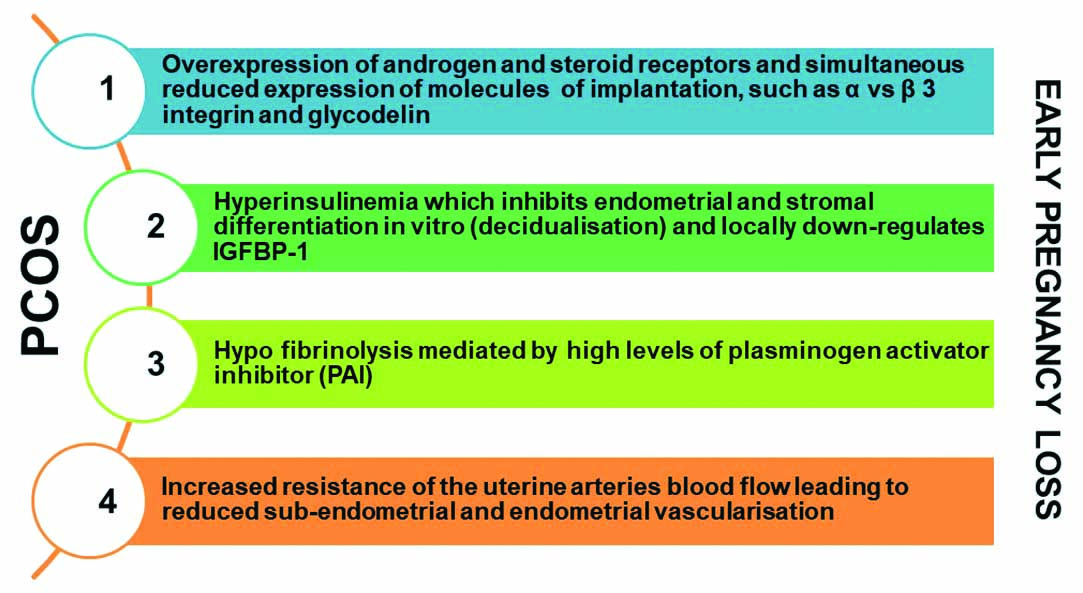
The EPL which is clinically defined as first trimester miscarriage is mostly seen in PCOS women. Two simultaneous studies has showed that 30-50% of PCOS women were prone to PCOS associated EPL when compared with 10-15% of normal women [35,36]. However, it has been difficult to establish the EPL rate associated with PCOS women mainly due to several confounding factors. Also, a study found that the incidence of spontaneous EPL was higher in woman who used ovulation-inducing agents when compared with the naturally ovulating and conceiving population [37]. Several risk factors including elevated LH levels are associated with EPL in women with PCOS [38,39]. When compared to those with normal LH, PCOS women with increased LH levels were at the higher risk of miscarriage with decreased conception rate [40]. In the subsequent studies it was documented that PCOS women who underwent long term pituitary suppression with a Gonadotropin Releasing Hormone (GnRH) agonist had decreased miscarriage rates [41,42]. Various mechanisms underlying the increased risk and pathogenesis of EPL in women with PCOS have been hypothesised and the probable ones are depicted in [Table/Fig-3].
Proposed mechanisms to explain underlying the risk and pathogenesis of Early Pregnancy Loss (EPL) in PCOS women Insulin-like Growth Factor Binding Protein 1 (IGFBP-1).
Literature suggests that 40-50% of the PCOS pregnancies are complicated by GDM [43]. Supporting studies also pointed evidence at obesity, as a confounding factor and hence such women could have increased risk of GDM associated PCOS. Two studies showed Body Mass Index (BMI) more than 25 kg/m2 to be the greatest predictor for GDM [44,45]. Contradictorily, Urman B et al., found that independent of BMI PCOS women are at increased risk of GDM [46]. Similarly, another study observed more cases of GDM and pre-eclampsia in non obese PCOS women supporting the evidence that this risk was mainly due to PCOS rather than obesity [47]. Later on a systematic review and meta-analysis concluded that the higher risk of gestational diabetes in PCOS women was a questionable finding [48]. The heterogenic nature of PCOS and the diversity in methodology among studies seems to be the main reason behind these conflicting results.
HDP, especially pre-eclampsia, is a leading cause of maternal death worldwide and research reports that 8% of the PCOS pregnancies are associated with HDP [49]. HDP includes Pregnancy Induced Hypertension (PIH), usually seen after 20 weeks of gestation, and pre-eclampsia which is PIH with proteinuria. The association between PCOS and HDP is not consistent. A couple of studies showed increased incidence of pre-eclampsia in PCOS women [50,51] whereas others documented similar prevalence of pre-eclampsia between PCOS and non PCOS women [44,52]. A meta-analysis reported in 2011 demonstrated an odds ratio of 4.23 and 4.07 for pre-eclampsia and PIH respectively in PCOS women [53].
Outcome of New-Borns of Mothers with PCOS
Infants born to PCOS mothers can have significantly worse perinatal outcomes when compared to infants born to non PCOS mothers. In 2006, a meta-analysis was conducted which aimed at evaluating pregnancy outcomes and associated neonatal complications in PCOS women. The study reported that the risk of admission to Neonatal Intensive Care Unit (NICU) and possibility of perinatal deaths were significantly higher in infants of PCOS mothers [54]. Evidence suggests that the Apgar score- a method used to summarise the health of new-born against infant mortality is found to be less than 5 in most of the infants born to the PCOS mothers [55]. The same study also showed that there was a risk of increased congenital anomalies in the babies born to women with PCOS.
Genetic Heritability
In all these years of research, clinical and genetic evidences have suggested that PCOS is a complex syndrome of autosomal dominant inheritance [56-58]. The familial aggregation studies and the twin studies aided in establishing the heritable basis of PCOS. The first evidence of the genetic basis of PCOS was reported in 1968 [59]. Early studies in the 1990s reported that, PCOS followed an autosomal dominant mode of inheritance as the results showed siblings of the PCOS probands had increased prevalence of PCOS related traits [60,61]. In concordance many other family studies supported this conjecture, where it was observed the first degree relatives of PCOS probands had a prevalence of PCOS ranging from 51-66%. Interestingly, the studies also reported that oligomenorrhea and hirsutism in PCOS women and male pattern baldness in males of the family could be due to a single gene [60,62]. A large study by Kashar-Miller M and Azziz R found that among the 250 PCOS probands, 75% of them reported at least one family member with either hirsutism alone or PCOS including hirsutism [63]. With 50% of mothers or sisters, 25% of aunts, and 20% of grandmothers having hirsutism or hirsutism with oligomenorrhea, this study established a strong familial aggregation for PCOS and its traits. Subsequent study done by the same research group found that PCOS was prevalent in 35% of the premenopausal mothers and 40% of the sisters of PCOS probands supporting the existing data [64].
Earlier studies conducted in 1995 and 1997 which examined the rate of PCOS in a small group of monozygotic (n=19) and dizygotic (n=15) twin pairs initially suggested that PCOS was not an autosomal dominant disorder. [65,66]. A subsequent large Dutch study published in 2006 with monozygotic (n=1332) and dizygotic (n=1873) twins identified 92 subjects with PCOS using a questionnaire based on the Rotterdam criteria. This study aimed to estimate the heritability of PCOS and if it has any genetic basis. In addition the study also investigated acne, hirsutism and oligomenorrhea as a trivariate model. The data demonstrated that monozygotic twins had higher correlation for PCOS when compared to their counterparts. The results of this study also confirmed the familial trait of PCOS was significantly due to genetic factors which predispose the family members of the probands to a risk of developing PCOS [67].
Genome Wide Association Studies (GWAS)
A great success has been achieved with the introduction of genotyping platforms and application of the same to many common multigenic diseases. Completion of the Human Genome Project gave access to complete reference genomes and therefore made it easier for the researchers to genotype millions of Single Nucleotide Polymorphisms (SNPs). PCOS is a multifactorial disease and any mutations affecting the ovaries directly or indirectly are associated with PCOS. Research community has always pondered upon identifying candidate genes involved in pathways related to the pathogenesis of PCOS. SNPs have the potential to reveal any small functional changes within a gene and can assist in understanding its differential impact in healthy and diseased individuals.
Till date there had been plenty of studies intending to identify candidate genes for the diagnosis of PCOS and many of them are not successful due to the multigenic architecture of the disease. Limited sample size, uneven control group, phenotypic heterogeneity, lack of exclusion of confounding factors (insulin resistance, obesity) are the root cause for the failed studies. GWAS associates specific loci and traits of a disease in cases and controls to help determine the allele distribution. Chen ZJ et al., in the early 2011 were the first ones to report GWAS in PCOS where they published three susceptibility loci for PCOS (LHCGR, THADA, and DENND1A) identified in a large case-control cohort of Chinese descent including 4,082 patients diagnosed as per the Rotterdam criteria and 6,687 control subjects [68].
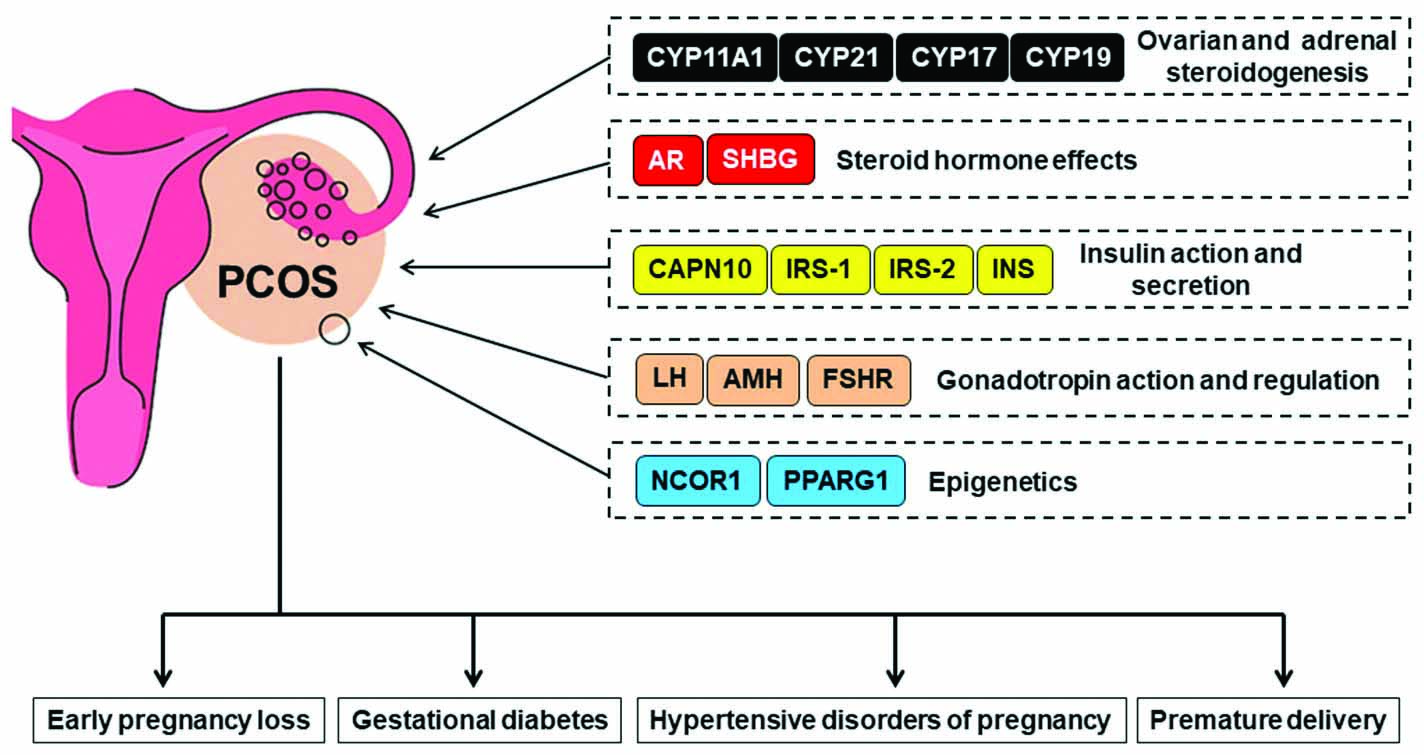
Shortly after a year, in 2012 a second GWAS in Chinese population was published in an expanded cohort of subjects and added eight novel risk loci potentially implicating both LHCGR and FSHR as independent risk genes [69]. A total of 11 PCOS risk genes including Luteinizing Hormone/Choriogonadotropin Receptor (LHCGR), Follicle-Stimulating Hormone Receptor (FSHR), Thyroid Adenoma Associated (THADA), Denn Domain-Containing Protein 1A (DENND1A), Chromosome 9 Open Reading Frame 3 (C9orf3), Yes-associated Protein 1 (YAP1), High Mobility Group AT-Hook 2 (HMGA2), Sulphite oxidase (RAB5B/SUOX), TOX3, Insulin Receptor (INSR) and SUMO1P1 were discovered by the two Chinese GWAS and other smaller studies. Overview of the most common genes are shown in [Table/Fig-4].
Overview of the most common genes whose polymorphism could have a direct impact in the development of PCOS and lead to further complications.
Recently, two GWAS data published in European cohorts have significantly increased the number of identified PCOS genes. The first report included a cohort of 984 PCOS subjects diagnosed as per National Institutes of Health (NIH) criteria and 2,964 control subjects. Two novel loci namely, GATA4 and NEIL2 were identified by this study [70]. A subsequent study published in the same year, had a unique and very large cohort. The initial phase consisted of nearly 5,000 self-reported PCOS patients and more than 80,000 control subjects from the online research survey platform (https://www.23andme.com/en-int/research/). The second phase of the study was performed in 2,000 clinically validated cases as per both NIH and Rotterdam criteria. A total of six loci associated with PCOS were identified at genome wide significance. Three of the six were new novel loci (ERBB4, RAD50, and KRR1), two of them were the previously reported loci in Chinese population (THADA and YAP1), and one previously reported in white population (FSHB) [71]. The relationships between SNPs identified by GWAS and the quantitative traits associated with PCOS needs to be further examined to link and better understand the disease biology.
Conclusion(s)
Till date PCOS remains as an endocrine puzzle causing uncharacteristically adverse hormonal disturbances in the affected women leading to metabolic and gynaecological concerns. All aspects of the syndrome starting from the classification to the diagnosis criteria are debatable. Identifying gene signatures for the diagnosis of PCOS has not been successful mainly due to the multigenic architecture of the disease. The identification of candidate genes to assess the risk of developing PCOS is the need of the hour as it helps to improve our understanding of the complex multifactorial syndrome. The recent advances in GWAS of PCOS have done this by providing a list of credible candidate genes. By combining the functional data of the gene signatures and the clinical manifestations of the affected individuals it is possible to understand the aetiology of the PCOS, improve the diagnosis and allow early intervention for treatment.
[1]. Crespo RP, Bachega TA, Mendonça BB, Gomes LG, An update of genetic basis of PCOS pathogenesisArchives of Endocrinology and Metabolism 2018 62:352-61.10.20945/2359-399700000004929972435 [Google Scholar] [CrossRef] [PubMed]
[2]. Dadachanji R, Shaikh N, Mukherjee S, Genetic variants associated with hyperandrogenemia in PCOS pathophysiologyGenetics Research International 2018 2018:762493210.1155/2018/762493229670770 [Google Scholar] [CrossRef] [PubMed]
[3]. Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO, The prevalence and features of the polycystic ovary syndrome in an unselected populationThe Journal of Clinical Endocrinology & Metabolism 2004 89(6):2745-49.10.1210/jc.2003-03204615181052 [Google Scholar] [CrossRef] [PubMed]
[4]. Wiweko B, Maidarti M, Priangga MD, Shafira N, Fernando D, Sumapraja K, Anti-mullerian hormone as a diagnostic and prognostic tool for PCOS patientsJournal of Assisted Reproduction and Genetics 2014 31(10):1311-16.10.1007/s10815-014-0300-625119192 [Google Scholar] [CrossRef] [PubMed]
[5]. Sahmay S, Atakul N, Oncul M, Tuten A, Aydogan B, Seyisoglu H, Serum anti-mullerian hormone levels in the main phenotypes of polycystic ovary syndromeEuropean Journal of Obstetrics & Gynecology and Reproductive Biology 2013 170(1):157-61.10.1016/j.ejogrb.2013.05.01923806449 [Google Scholar] [CrossRef] [PubMed]
[6]. Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R, Criteria, prevalence, and phenotypes of polycystic ovary syndromeFertility and Sterility 2016 106(1):06-15.10.1016/j.fertnstert.2016.05.00327233760 [Google Scholar] [CrossRef] [PubMed]
[7]. Guastella E, Longo RA, Carmina E, Clinical and endocrine characteristics of the main polycystic ovary syndrome phenotypesFertility and Sterility 2010 94(6):2197-201.10.1016/j.fertnstert.2010.02.01420303485 [Google Scholar] [CrossRef] [PubMed]
[8]. Jamil AS, Alalaf SK, Al-Tawil NG, Al-Shawaf T, Comparison of clinical and hormonal characteristics among four phenotypes of polycystic ovary syndrome based on the Rotterdam criteriaArchives of Gynecology and Obstetrics 2016 293(2):447-56.10.1007/s00404-015-3889-526408006 [Google Scholar] [CrossRef] [PubMed]
[9]. Panidis D, Tziomalos K, Papadakis E, Chatzis P, Kandaraki EA, Tsourdi EA, Associations of menstrual cycle irregularities with age, obesity and phenotype in patients with polycystic ovary syndromeHormones 2015 14(3):431-37.10.14310/horm.2002.159326188231 [Google Scholar] [CrossRef] [PubMed]
[10]. Ávila MA, Bruno RV, Barbosa FC, Andrade FC, Silva AC, Nardi AE, Polycystic ovary syndrome: Implications of metabolic dysfunctionRevista do Colégio Brasileiro de Cirurgiões 2014 41:106-10.10.1590/S0100-6991201400020000624918723 [Google Scholar] [CrossRef] [PubMed]
[11]. Sirmans SM, Pate KA, Epidemiology, diagnosis, and management of polycystic ovary syndromeClinical Epidemiology 2014 6:110.2147/CLEP.S3755924379699 [Google Scholar] [CrossRef] [PubMed]
[12]. Lin TY, Lin PY, Su TP, Li CT, Lin WC, Chang WH, Risk of developing obstructive sleep apnea among women with polycystic ovarian syndrome: A nationwide longitudinal follow-up studySleep Medicine 2017 36:165-69.10.1016/j.sleep.2016.12.02928599952 [Google Scholar] [CrossRef] [PubMed]
[13]. Deeks AA, Gibson-Helm ME, Teede HJ, Anxiety and depression in polycystic ovary syndrome: A comprehensive investigationFertility and Sterility 2010 93(7):2421-23.10.1016/j.fertnstert.2009.09.01820117778 [Google Scholar] [CrossRef] [PubMed]
[14]. Dumesic DA, Lobo RA, Cancer risk and PCOSSteroids 2013 78(8):782-85.10.1016/j.steroids.2013.04.00423624028 [Google Scholar] [CrossRef] [PubMed]
[15]. Lujan ME, Chizen DR, Pierson RA, Diagnostic criteria for polycystic ovary syndrome: Pitfalls and controversiesJournal of Obstetrics and Gynaecology Canada 2008 30(8):671-79.10.1016/S1701-2163(16)32915-2 [Google Scholar] [CrossRef]
[16]. Balen AH, Laven JS, Tan SL, Dewailly D, Ultrasound assessment of the polycystic ovary: International consensus definitionsHuman Reproduction Update 2003 9(6):505-14.10.1093/humupd/dmg04414714587 [Google Scholar] [CrossRef] [PubMed]
[17]. Michelmore K, Ong K, Mason S, Bennett S, Perry L, Vessey M, Clinical features in women with polycystic ovaries: Relationships to insulin sensitivity, insulin gene VNTR and birth weightClinical Endocrinology 2001 55(4):439-46.10.1046/j.1365-2265.2001.01375.x11678825 [Google Scholar] [CrossRef] [PubMed]
[18]. Carmina E, Lobo RA, Polycystic ovaries in hirsute women with normal mensesThe American Journal of Medicine 2001 111(8):602-06.10.1016/S0002-9343(01)00979-2 [Google Scholar] [CrossRef]
[19]. Cresswell J, Fraser RB, Bruce C, Egger P, Phillips D, Barker DJ, Relationship between polycystic ovaries, body mass index and insulin resistanceActa obstetriciaetgynecologica Scandinavica 2003 82(1):61-64.10.1034/j.1600-0412.2003.820111.x12580842 [Google Scholar] [CrossRef] [PubMed]
[20]. Azziz R, Diagnostic criteria for polycystic ovary syndrome: A reappraisalFertil Steril 2005 83(5):1343-46.10.1016/j.fertnstert.2005.01.08515866567 [Google Scholar] [CrossRef] [PubMed]
[21]. Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: An androgen excess society guidelineThe Journal of Clinical Endocrinology & Metabolism 2006 91(11):4237-45.10.1210/jc.2006-017816940456 [Google Scholar] [CrossRef] [PubMed]
[22]. Knochenhauer ES, Key TJ, Kahsar-Miller M, Waggoner W, Boots LR, Azziz R, Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern United States: A prospective studyThe Journal of Clinical Endocrinology & Metabolism 1998 83(9):3078-82.10.1210/jc.83.9.3078 [Google Scholar] [CrossRef]
[23]. Chan JL, Kar S, Vanky E, Morin-Papunen L, Piltonen T, Puurunen J, Racial and ethnic differences in the prevalence of metabolic syndrome and its components of metabolic syndrome in women with polycystic ovary syndrome: A regional cross-sectional studyAmerican Journal of Obstetrics and Gynecology 2017 217(2):189-e1.10.1016/j.ajog.2017.04.00728400308 [Google Scholar] [CrossRef] [PubMed]
[24]. Asunción M, Calvo RM, San Millán JL, Sancho J, Avila S, Escobar-Morreale HF, A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from SpainJ Clin Endocrinol Metab 2000 85(7):2434-38.10.1210/jcem.85.7.668210902790 [Google Scholar] [CrossRef] [PubMed]
[25]. Michelmore KF, Balen AH, Dunger DB, Vessey MP, Polycystic ovaries and associated clinical and biochemical features in young womenClinical Endocrinology 1999 51(6):779-86.10.1046/j.1365-2265.1999.00886.x10619984 [Google Scholar] [CrossRef] [PubMed]
[26]. Li R, Zhang Q, Yang D, Li S, Lu S, Wu X, Prevalence of polycystic ovary syndrome in women in China: A large community-based studyHuman Reproduction 2013 28(9):2562-69.10.1093/humrep/det26223814096 [Google Scholar] [CrossRef] [PubMed]
[27]. Gill H, Tiwari P, Dabadghao P, Prevalence of polycystic ovary syndrome in young women from North India: A Community-based studyIndian Journal of Endocrinology and Metabolism 2012 16(Suppl 2):S389 [Google Scholar]
[28]. Bharathi RV, Swetha S, Neerajaa J, Madhavica JV, Janani DM, Rekha SN, An epidemiological survey: Effect of predisposing factors for PCOS in Indian urban and rural populationMiddle East Fertility Society Journal 2017 22(4):313-16.10.1016/j.mefs.2017.05.007 [Google Scholar] [CrossRef]
[29]. Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R, Prevalence of polycystic ovarian syndrome in Indian adolescentsJournal of Pediatric and Adolescent Gynecology 2011 24(4):223-27.10.1016/j.jpag.2011.03.00221600812 [Google Scholar] [CrossRef] [PubMed]
[30]. Ramanand SJ, Ghongane BB, Ramanand JB, Patwardhan MH, Ghanghas RR, Jain SS, Clinical characteristics of polycystic ovary syndrome in Indian womenIndian Journal of Endocrinology and Metabolism 2013 17(1):13810.4103/2230-8210.10785823776867 [Google Scholar] [CrossRef] [PubMed]
[31]. Joshi B, Mukherjee S, Patil A, Purandare A, Chauhan S, Vaidya R, A cross-sectional study of polycystic ovarian syndrome among adolescent and young girls in Mumbai, IndiaIndian Journal of Endocrinology and Metabolism 2014 18(3):31710.4103/2230-8210.13116224944925 [Google Scholar] [CrossRef] [PubMed]
[32]. Akram M, Roohi N, Endocrine correlates of polycystic ovary syndrome in Pakistani womenJ Coll Physicians Surg Pak 2015 25(1):22-26. [Google Scholar]
[33]. Khan MJ, Ullah A, Basit S, Genetic basis of polycystic ovary syndrome (PCOS): Current perspectivesThe Application of Clinical Genetics 2019 12:24910.2147/TACG.S20034131920361 [Google Scholar] [CrossRef] [PubMed]
[34]. Barbour LA, McCurdy CE, Hernandez TL, Kirwan JP, Catalano PM, Friedman JE, Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetesDiabetes Care 2007 30(Supplement 2):S112-19.10.2337/dc07-s20217596458 [Google Scholar] [CrossRef] [PubMed]
[35]. Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE, Effects of metformin on early pregnancy loss in the polycystic ovary syndromeThe Journal of Clinical Endocrinology & Metabolism 2002 87(2):524-29.10.1210/jcem.87.2.820711836280 [Google Scholar] [CrossRef] [PubMed]
[36]. Al-Biate MA, Effect of metformin on early pregnancy loss in women with polycystic ovary syndromeTaiwanese Journal of Obstetrics and Gynecology 2015 54(3):266-69.10.1016/j.tjog.2013.06.02026166338 [Google Scholar] [CrossRef] [PubMed]
[37]. Palomba S, de Wilde MA, Falbo A, Koster MP, La Sala GB, Fauser BC, Pregnancy complications in women with polycystic ovary syndromeHum Reprod Update 2015 21(5):575-92.10.1093/humupd/dmv02926117684 [Google Scholar] [CrossRef] [PubMed]
[38]. Glueck CJ, Wang P, Fontaine RN, Sieve-Smith L, Tracy T, Moore SK, Plasminogen activator inhibitor activity: An independent risk factor for the high miscarriage rate during pregnancy in women with polycystic ovary syndromeMetabolism 1999 48(12):1589-95.10.1016/S0026-0495(99)90250-0 [Google Scholar] [CrossRef]
[39]. Liddell HS, Sowden K, Farquhar CM, Recurrent miscarriage: Screening for polycystic ovaries and subsequent pregnancy outcomeAustralian and New Zealand Journal of Obstetrics and Gynaecology 1997 37(4):402-06.10.1111/j.1479-828X.1997.tb02447.x9429701 [Google Scholar] [CrossRef] [PubMed]
[40]. Regan LE, Owen EJ, Jacobs HS, Hypersecretion of luteinising hormone, infertility, and miscarriageThe Lancet 1990 336(8724):1141-44.10.1016/0140-6736(90)92765-A [Google Scholar] [CrossRef]
[41]. Homburg R, Levy T, Berkovitz D, Farchi J, Feldberg D, Ashkenazi J, Gonadotropin-releasing hormone agonist reduces the miscarriage rate for pregnancies achieved in women with polycystic ovarian syndromeFertility and Sterility 1993 59(3):527-31.10.1016/S0015-0282(16)55794-X [Google Scholar] [CrossRef]
[42]. Balen AH, Tan SL, MacDougall J, Jacobs HS, Miscarriage rates following in-vitro fertilization are increased in women with polycystic ovaries and reduced by pituitary desensitization with buserelinHuman Reproduction 1993 8(6):959-64.10.1093/oxfordjournals.humrep.a1381748345091 [Google Scholar] [CrossRef] [PubMed]
[43]. Veltman-Verhulst SM, Van Haeften TW, Eijkemans MJ, De Valk HW, Fauser BC, Goverde AJ, Sex hormone-binding globulin concentrations before conception as a predictor for gestational diabetes in women with polycystic ovary syndromeHuman Reproduction 2010 25(12):3123-28.10.1093/humrep/deq272 [Google Scholar] [CrossRef]
[44]. Mikola M, Hiilesmaa V, Halttunen M, Suhonen L, Tiitinen A, Obstetric outcome in women with polycystic ovarian syndromeHuman Reproduction 2001 16(2):226-29.10.1093/humrep/16.2.22611157811 [Google Scholar] [CrossRef] [PubMed]
[45]. Turhan NÖ, Seckin NC, Aybar F, Inegöl I, Assessment of glucose tolerance and pregnancy outcome of polycystic ovary patientsInternational Journal of Gynecology & Obstetrics 2003 81(2):163-68.10.1016/S0020-7292(03)00003-1 [Google Scholar] [CrossRef]
[46]. Urman B, Sarac E, Dogan L, Gurgan T, Pregnancy in infertile PCOD patients. complications and outcomeThe Journal of Reproductive Medicine 1997 42(8):501-05. [Google Scholar]
[47]. Li GH, Fan L, Zhang L, Liu XW, Sun CJ, Zhang WY, Clinical characteristics and perinatal outcomes of non overweight/obese pregnant women with polycystic ovary syndromeZhonghuayixuezazhi 2011 91(39):2753-56. [Google Scholar]
[48]. Toulis KA, Goulis DG, Kolibianakis EM, Venetis CA, Tarlatzis BC, Papadimas I, Risk of gestational diabetes mellitus in women with polycystic ovary syndrome: A systematic review and a meta-analysisFertility and Sterility 2009 92(2):667-77.10.1016/j.fertnstert.2008.06.04518710713 [Google Scholar] [CrossRef] [PubMed]
[49]. Roberts JM, Pearson G, Cutler J, Lindheimer M, Summary of the NHLBI working group on research on hypertension during pregnancyHypertension 2003 41(3):437-45.10.1161/01.HYP.0000054981.03589.E912623940 [Google Scholar] [CrossRef] [PubMed]
[50]. Diamant YZ, Rimon E, Evron S, High incidence of pre-eclamptic toxemia in patients with polycystic ovarian diseaseEuropean Journal of Obstetrics & Gynecology and Reproductive Biology 1982 14(3):199-204.10.1016/0028-2243(82)90097-1 [Google Scholar] [CrossRef]
[51]. Radon PA, McMahon MJ, Meyer WR, Impaired glucose tolerance in pregnant women with polycystic ovary syndromeObstetrics & Gynecology 1999 94(2):194-97.10.1097/00006250-199908000-0000710432126 [Google Scholar] [CrossRef] [PubMed]
[52]. Haakova L, Cibula D, Rezabek K, Hill M, Fanta M, Zivny J, Pregnancy outcome in women with PCOS and in controls matched by age and weightHuman Reproduction 2003 18(7):1438-41.10.1093/humrep/deg28912832369 [Google Scholar] [CrossRef] [PubMed]
[53]. Kjerulff LE, Sanchez-Ramos L, Duffy D, Pregnancy outcomes in women with polycystic ovary syndrome: A meta-analysisAmerican Journal of Obstetrics and Gynecology 2011 204(6):558-e1.10.1016/j.ajog.2011.03.02121752757 [Google Scholar] [CrossRef] [PubMed]
[54]. Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS, A meta-analysis of pregnancy outcomes in women with polycystic ovary syndromeHuman Reproduction Update 2006 12(6):673-83.10.1093/humupd/dml03616891296 [Google Scholar] [CrossRef] [PubMed]
[55]. Doherty DA, Newnham JP, Bower C, Hart R, Implications of polycystic ovary syndrome for pregnancy and for the health of offspringObstetrics & Gynecology 2015 125(6):1397-406.10.1097/AOG.000000000000085226000511 [Google Scholar] [CrossRef] [PubMed]
[56]. Wilroy Jr RS, Givens JR, Wiser WL, Coleman SA, Andersen RN, Summitt RL, Hyperthecosis: An inheritable form of polycystic ovarian diseaseBirth Defects Original Article Series 1975 11(4):81-85. [Google Scholar]
[57]. Franks S, Polycystic ovary syndromeNew England Journal of Medicine 1995 333(13):853-61.10.1056/NEJM1995092833313077651477 [Google Scholar] [CrossRef] [PubMed]
[58]. Jahanfar S, Eden JA, Genetic and non genetic theories on the etiology of polycystic ovary syndromeGynecological Endocrinology 1996 10(5):357-64.10.3109/095135996090128238915666 [Google Scholar] [CrossRef] [PubMed]
[59]. Cooper HE, Spellacy WN, Prem KA, Cohen WD, Hereditary factors in the Stein-Leventhal syndromeAmerican Journal of Obstetrics and Gynecology 1968 100(3):371-87.10.1016/S0002-9378(15)33704-2 [Google Scholar] [CrossRef]
[60]. Carey AH, Chan KL, Short F, White D, Williamson R, Franks S, Evidence for a single gene effect causing polycystic ovaries and male pattern baldnessClinical Endocrinology 1993 38(6):653-58.10.1111/j.1365-2265.1993.tb02150.x8334753 [Google Scholar] [CrossRef] [PubMed]
[61]. Hague WM, Adams J, Reeders ST, Peto TE, Jacobs HS, Familial polycystic ovaries: A genetic disease?Clinical Endocrinology 1988 29(6):593-605.10.1111/j.1365-2265.1988.tb03707.x3076848 [Google Scholar] [CrossRef] [PubMed]
[62]. Govind A, Obhrai MS, Clayton RN, Polycystic ovaries are inherited as an autosomal dominant trait: Analysis of 29 polycystic ovary syndrome and 10 control familiesThe Journal of Clinical Endocrinology & Metabolism 1999 84(1):38-43.10.1210/jcem.84.1.53829920059 [Google Scholar] [CrossRef] [PubMed]
[63]. Kashar-Miller M, Azziz R, Heritability and the risk of developing androgen excessThe Journal of Steroid Biochemistry and Molecular Biology 1999 69(1-6):261-68.10.1016/S0960-0760(99)00043-6 [Google Scholar] [CrossRef]
[64]. Kahsar-Miller MD, Nixon C, Boots LR, Go RC, Azziz R, Prevalence of Polycystic Ovary Syndrome (PCOS) in first-degree relatives of patients with PCOSFertility and Sterility 2001 75(1):53-58.10.1016/S0015-0282(00)01662-9 [Google Scholar] [CrossRef]
[65]. Jahanfar S, Eden JA, Warren P, Seppälä M, Nguyen TV, A twin study of polycystic ovary syndromeFertility and Sterility 1995 63(3):478-86.10.1016/S0015-0282(16)57412-3 [Google Scholar] [CrossRef]
[66]. Jahanfar S, Eden JA, Nguyen T, Wang XL, Wilcken DE, A twin study of polycystic ovary syndrome and lipidsGynecological Endocrinology 1997 11(2):111-17.10.3109/095135997091525219174852 [Google Scholar] [CrossRef] [PubMed]
[67]. Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI, Heritability of polycystic ovary syndrome in a Dutch twin-family studyThe Journal of Clinical Endocrinology & Metabolism 2006 91(6):2100-04.10.1210/jc.2005-149416219714 [Google Scholar] [CrossRef] [PubMed]
[68]. Chen ZJ, Zhao H, He L, Shi Y, Qin Y, Shi Y, Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16. 3, 2p21 and 9q33. 3Nature genetics 2011 43(1):55-59.10.1038/ng.73221151128 [Google Scholar] [CrossRef] [PubMed]
[69]. Shi Y, Zhao H, Shi Y, Cao Y, Yang D, Li Z, Genome-wide association study identifies eight new risk loci for polycystic ovary syndromeNature Genetics 2012 44(9):1020-25.10.1038/ng.238422885925 [Google Scholar] [CrossRef] [PubMed]
[70]. Hayes MG, Urbanek M, Ehrmann DA, Armstrong LL, Lee JY, Sisk R, Genome-wide association of polycystic ovary syndrome implicates alterations in gonadotropin secretion in European ancestry populationsNature Communications 2015 6(1):01-03.10.1038/ncomms850226284813 [Google Scholar] [CrossRef] [PubMed]
[71]. Day FR, Hinds DA, Tung JY, Stolk L, Styrkarsdottir U, Saxena R, Causal mechanisms and balancing selection inferred from genetic associations with polycystic ovary syndromeNature Communications 2015 6(1):01-07.10.1038/ncomms946426416764 [Google Scholar] [CrossRef] [PubMed]