Often cases are referred to the radiologists from the out-patient departments for ruling out any posterior segment pathologies, and even before any operative procedure. The predictive value of B-scan USG has been found to be 100% for diagnosing retinal detachment and Intra-Ocular Foreign Body (IOFB). It was also found to be useful for both surgical and medical management, and also for prognosis [2]. Studies have shown that hidden posterior segment lesions can be detected prior to surgery for cataract [3]. Even determining the integrity of posterior capsule in posterior polar cataract, B-scan USG can be very efficiently used [4]. The use of B-scan USG in diagnosing cases of acute Fundus Obscuring Vitreous Haemorrhage (FOVH) also has got high sensitivity [5]. B-scan USG is also useful in alkali burn eyes, where in such cases it’s diagnostic concordance rate as compared to the intraoperative findings of lens is 100% [6]. It has also been shown that B-scan USG is a reliable investigator-dependent prognostic method along with Bio-Microscopy (BM) to clinically detect if the posterior vitreous cortex is detached [7]. When fundus examination is not possible, USG is known to be a better method for investigation of possible retinal tears [8].
Materials and Methods
The study was hospital based and cross-sectional in nature. It was conducted at a tertiary care centre of Eastern India from June 2007 to June 2009 jointly in the Department of Radiodiagnosis and Department of Ophthalmology. Institute Ethical Clearance was taken before conducting the study (10/IEC dt 06.08.2008), and patient confidentiality was maintained throughout the study. Written informed consent was taken before conducting USG. Patients who presented to the Ophthalmology department with suspected intraocular pathology, or in conditions where fundoscopy could not be carried out such as blunt trauma to the eye, opaque ocular media, etc., were referred to the Radiology department for B-scan ophthalmic USG.
Inclusion criteria: Patients with suspected posterior segment eye disorders (blunt trauma leading to opacity in media, intraocular pathology like retinal detachment, haemorrhage, tumour, retinopathy, etc.,) irrespective of any age and gender were included in the study.
Exclusion criteria: Exclusion criteria included patients who did not consent or agree for follow-up, or who had been operated on the eye for similar conditions in the past, or had been already diagnosed using alternate methods such as fundoscopy, Optical Coherence Tomography (OCT), Magnetic Resonance Imaging (MRI), fluoroscopy, etc., which could possibly bias the selection process and also the interpretation were excluded from the study.
Sample size calculation: Sample size was calculated calculated, assuming a null hypothesis of 0.5 and area under Receiver Operating Curve (RCC) of 0.7, and with an alpha value of 0.05 and power of the study 90%, a minimum of 82 subjects were required.
Study Procedure
Diagnosis by conventional methods such as direct ophthalmoscopy was taken as gold standard/reference test for detecting posterior segment pathology. Cases where direct ophthalmoscopy could not be done due to reasons such as presence of dense cataract, opaque media, etc., were grouped under cases where diagnosis could not be verified (using reference test methods) while tabulating and considering for verification bias correction, but under False Positives (FP) in regular analysis. Cases detected using both reference test and B-mode USG were regarded as True Positives (TP), detected by USG but not by reference test as FP, not detected by USG but detected by reference test as False Negatives (FN) and not detected by both as True Negatives (TN) during regular analysis. However, while correcting for verification bias, there was a separate group where disease verification could not be done, and where B-scan USG was either positive or negative for presence of posterior segment pathology [13].
Accuracy of USG was calculated in comparison with reference test in terms of sensitivity (Sn), specificity (Sp), PPV, NPV and accuracy. Likelihood ratios (LR+ and LR-) were calculated from sensitivity and specificity. Prevalence of the disease (posterior segment disorders) was calculated as proportion of cases diagnosed using reference test (TP+FP) out of the total cases. Pre-test odds were calculated from the derived prevalence. Post-test odds was derived by multiplying pre-test odds with LR, while its probability was finally derived from post-test odds and Fagan’s nomogram [11,12]. This was done for both regular analysis and for correction of verification bias. Adjustment for verification bias was considered during the analysis [13].
Statistical Analysis
Data were entered in an excel sheet (Microsoft Excel 2010). They were cleaned for any missing values, and imported to Stata 12.1 SE for analysis. Data analysis was done for all the complete case records available. Qualitative data were presented as numbers with percentages, while quantitative data were represented with mean and standard deviation. Data were tabulated for calculating accuracy of B-mode USG. Additional analysis was done considering correction for verification bias.
Results
A total of 84 cases were referred to the radiology department from the ophthalmology for confirmation of presence of a possible posterior segment pathology.
The mean age of the study participants was 37.37±19.49 years (minimum 1 year, maximum 90 years). Maximum number of study participants was between 41-50 years at presentation (30 cases, 35.7%). The number of males among the study participants was 61 (72.6%). The common presenting symptoms among the referred cases were low vision (42 cases, 50.0%) followed by black spots in the visual field (9 cases, 10.7%) and pain around eyes (8 cases, 9.5%) [Table/Fig-1].
Presenting symptoms among study participants (n=84).
| Presenting symptoms | Numbers | % |
|---|
| Low vision | 42 | 50.00 |
| Black spots in visual field | 9 | 10.71 |
| Pain around eyes | 8 | 9.52 |
| Flashes of light | 7 | 8.33 |
| Blurring of vision | 5 | 5.95 |
| Leukocoria | 5 | 5.95 |
| Loss of vision | 3 | 3.57 |
| Bleeding from eyes | 2 | 2.38 |
| Shrunken eyes | 1 | 1.19 |
| No presenting symptoms | 2 | 2.38 |
The most common condition that was found among the study participants was cataract/corneal opacity (45 cases, 54%). Of the 45 cataract cases, three had complete loss of vision, while rest had low vision. Risk factors included raised intraocular pressure (8 cases, 9.5%). Diabetes and hypertension were however also the presenting general risk factors among the study participants in few cases (8.3% and 4.7%, respectively) [Table/Fig-2].
Risk factors of study participants (n=84).
| Risk factors | Numbers | % |
|---|
| No risk factor | 20 | 23.81 |
| History of trauma | 33 | 39.29 |
| History of suspected intraocular pathology | 3 | 3.57 |
| Presence of general risk factors | 11 | 13.09 |
| Diabetes mellitus | 7 | 8.33 |
| Hypertension | 4 | 4.76 |
| Presence of ocular risk factor | 17 | 20.23 |
| Increased intraocular pressure | 8 | 9.52 |
| Posterior synechia | 6 | 7.14 |
| Subluxated lens | 2 | 2.38 |
| Keratic precipitates | 1 | 1.19 |
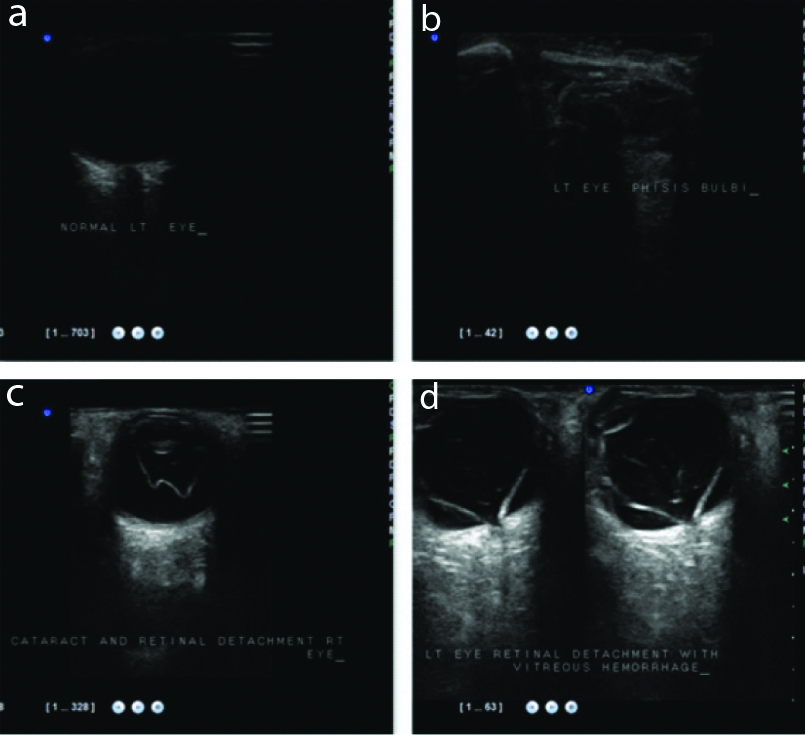
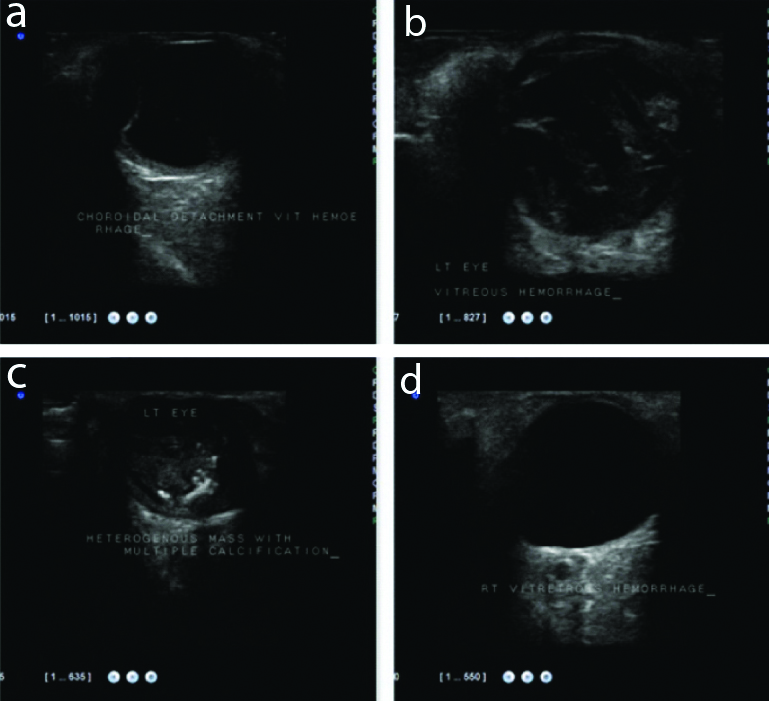
Posterior segment eye disorders could be ruled out to a good extent in cataract cases, trauma cases, suspected intraocular pathology and presence of leukocoria. It was best for confirming diagnosis of a posterior segment disorder in the presence of leukocoria (5 out of 5 cases, 100%) and cataract (7 cases out of 7, 100%), followed by suspected intraocular pathology (2 out of 3 cases, 66.7%). Of all the cases of cataract, posterior segment pathology was suspected in only seven cases. A cross-tabulation of the diagnosis by reference test methods compared to that with ultrasonography is shown in [Table/Fig-3]. Some of the B-scan images of normal eye and posterior segment pathologies is shown in [Table/Fig-4,5].
Cross-tabulation of posterior segment disorder diagnosis by reference test methods and ultrasonography (n=84).
| Diagnosis using B-scan USG | Diagnosis by reference test |
|---|
| CD+VH | N | ND | RD | RM | SL | VH | Total |
|---|
| CD+VH | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| N | 0 | 23 | 37 | 0 | 0 | 0 | 0 | 60 |
| RM | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 5 |
| RD | 0 | 0 | 6 | 1 | 0 | 0 | 0 | 7 |
| SL | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| VH | 0 | 0 | 7 | 0 | 0 | 0 | 3 | 10 |
| Total | 1 | 23 | 50 | 1 | 5 | 1 | 3 | 84 |
CD+VH: Choroidal detachment with vitreous haemorrhage; N: Normal; ND: Not done; RD: Retinal detachment; RM: Retinal mass; SL: Subluxated lens; VH: Vitreous haemorrhage
B-scan ocular ultrasound images in sequence a) Normal, b) Phthisis bulbi, c) Cataract with retinal detachment, d) Retinal detachment with vitreous haemorrhage. (identity hidden).
B-scan ocular ultrasound images in sequence a) Choroidal detachment with Vitreous haemorrhage, b) Left eye Vitreous hemorrhage, c) Retiniblasoma, d) Right eye Vitreous haemorrhage. (identity hidden).
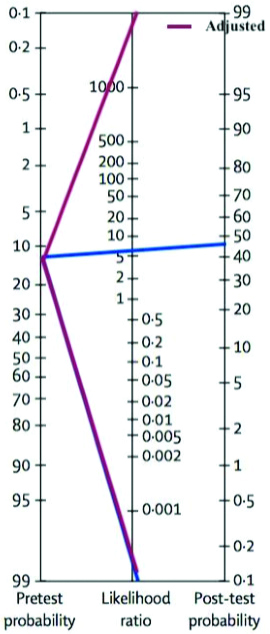
The accuracy of diagnosis using B-scan USG for posterior segment disorders in comparison with reference test, was calculated with and without verification bias correction [Table/Fig-6a,b]. Prevalence of posterior segment disorder (using reference test method) was found to be 13.1%. Sensitivity of B-scan USG was found to be 100%, as was also the NPV [Table/Fig-7]. Adjusted positive LR was found to be ∞ (5.84 without adjustment), which increased the post-test probability to 6.6% (also confirmed using Fagan’s nomogram) [Table/Fig-8].
Accuracy of diagnosis using B-scan USG for posterior segment disorders (n=84).
| a) Without verification bias correction |
|---|
| B-scan USG | Reference test (Indirect ophthalmoscopy) | Total |
|---|
| Disease present | Disease absent |
|---|
| Test positive | 11 (TP) | 13 (FP) | 24 |
| Test negative | 0 (FN) | 60 (TN) | 60 |
| Total | 11 | 73 | 84 |
| b) Considering verification bias correction |
| B-scan USG | Reference test (Indirect ophthalmoscopy) | Total |
| Disease present | Disease absent | Disease verification could not be done |
| Test positive | 11 (s1) | 0 (r1) | 13 (u1) | 24 (n1) |
| Test negative | 0 (s0) | 23 (r0) | 37 (u0) | 60 (n0) |
| Total | 11 | 23 | 50 | 84 |
TP: True positive; FP: False positive; FN: False negative; TN: True negative
Calculations involved in diagnostic accuracy of B-scan USG among study participants (n=84).
| Refer to table 6 (a) and 4 (b) for regular accuracy analysis and adjustment for verification bias respectivelySensitivity (Sn)=TP/(TP+FN)×100=11/11×100=100%Specificity (Sp)=TN/(TN+FP)×100=60/73×100=82.9%LR+=Sn/(1-Sp)×100=1/(1-0.829)×100=5.84LR-=(1-Sn)/Sp×100=(1-1)/0.829×100=0Adjusted Sensitivity (Sn)=(s1n1/(s1+r1))/((s1n1/(s1+r1))+(s0n0/(s0+r0)))×100=100%Adjusted Specificity (Sp)=(r0n0/(s0+r0))/((r0n0/(s0+r0))+(r1n1/(s1+r1)))×100=100%Adjusted LR+=Sn/(1-Sp)×100=∞Adjusted LR-=(1-Sn)/Sp×100=0PPV=TP/(TP+FP)×100=11/24×100=45.33%NPV=TN/(TN+FN)×100=60/60×100=100%Accuracy=(TP+TN)/(TP+TN+FP+FN)×100=71/84×100=84.52%Adjusted accuracy=(s1+r0)/(s1+r1+s0+r0)×100=100%Prevalence=(TP+FN)/(TP+TN+FP+FN)×100=11/84×100=13.1%Pre-test odds=Prevalance/(1-prevalance)=0.13/(1-0.13)=0.15Post-test odds+=Pre-test odds×LR^+=0.15×5.84=0.876Adjusted post-test odds+=Pre-test odds×Adjusted LR+=∞Post-test probability+=(Post-test odds)/(Post-test odds+1)=0.876/(0.876+1)=46.6Adjusted post-test probability+=(Post-test odds+)/(Post-test odds+1)=∞Post-test odds-=Pretest odds×LR^-=0.15×0=0Adjusted post-test odds-=Pre-test odds×Adjusted LR-=0Post-test probability-=(Post-test odds)/(Post-test odds+1)=0/(0+1)=0Adjusted post-test probability-=(Post-test odds)/(Post-test odds+1)=0 |
Fagan’s nomogram to detect post-test probability (LR+=5.84, LR-=0, Adjusted LR+=∞, Adjusted LR=0).
Discussion
Eye is situated in the anterior part of the orbit embedded in fat with the Tenon’s capsule separating it from the orbital wall. Posterior segment of the eye, which constitutes the major portion (5/6th of the eye) is composed of vitreous cavity, retina, choroid, sclera, episclera, and occasionally subluxated lens.
Cystic composition and even superficial location makes the eye an ideal organ for USG examination with unique acoustic advantages being offered by its USG imaging. The anechoic vitreous acts as a natural contrast for USG purposes. USG becomes the most practical method of obtaining images of the posterior segment when light conducting media are opaque. It is most commonly employed prior to vitrectomy also. Ophthalmic USG may be of A-type or B-type. A-scan can be used for biometric calculation, while B-scan for quantifying the reflectivity of lesions in the eye and orbit. A 20 MHz probe is used for lens and vitreous while 50 MHz probe for anterior segment (also known as USG BM). Routine ocular scanning is done with B-scan using 7.5 MHz or above frequency transducers [1,14].
Ophthalmic USG offers multiple advantages over Computerised Tomographic (CT) scan and MRI. It produces real time images of the eye and orbit with a very high resolution (0.1 to 0.01 mm). Multiple cross-sectional and radial cuts can be rapidly obtained at the bedside or even in an operating room, as it is portable. It is less expensive and without radiation hazards. It can categorise and predict the location of pathology in the posterior chamber of eye very well [15].
Ophthalmic USG uses high frequency sound waves (>20 KHz) transmitted and received through a probe, which then gets converted into electric signals which are read on a monitor. The higher the frequency of USG, the shorter is the wavelength. There is a direct relationship between wavelength and depth of the tissue penetrance (the shorter the wavelength, the more shallow is the penetrance). A shorter wavelength also gives a high resolution image. Ophthalmic USG use around 10 MHz and thus produce detailed resolution images of the posterior segment of the eye. Sound travels faster in solid than in liquid mediums and eye is composed of both, an important aspect to be considered while dealing with the eye. Sound travelling from one medium to the other gets reflected back at the interface on to the probe, and this reflection is directly proportional to the density difference between the media. In B-scan USG, these echoes are represented as multiple dots forming an image on the screen. The stronger the echo, the brighter is the dot [14].
Keeping the probe perpendicular to the area of interest gives a greater reflection on to the probe, and an inclined angle loses this intensity and clarity. Denser medium also end up with greater absorption, and thus compromising the resolution of the image. Presence of a dense cataract thus hampers the image resolution as compared to a normal crystalline lens, as also is a calcification mass. This may lead to no signal posterior to the medium, which is termed as shadowing. Pulse-echo system enables to compensate for this by amplifying the display through adjustment of the gain [14].
Andreoli MT et al., retrospectively reviewed ten years’ data (2000-2010) of 965 open globe injuries in Massachusetts where B-scan ultrasonography was used and found that the predictive value of B-scan USG was 100% for diagnosing retinal detachment and IOFB. Other diagnoses such as retinal detachment, disorganised posterior contents, haemorrhagic Choroidal Detachment (CD), etc. were also found to have worse visual acuity at final follow-up. They concluded that B-scan USG can offer both diagnostic and prognostic information. It was also found to be useful for both surgical and medical management [2]. The PPV found in this study was low, however NPV was 100%, may be as present study was not meant specifically for diagnosing retinal detachment and IOFB.
In a study by Qureshi MA and Laghari K for pre-surgical planning of cataract patients done among 750 cataract cases, they concluded that if B-scan USG is used as a diagnostic tool, the hidden posterior segment lesions can be detected prior to surgery. This if done routinely in preoperative cases of cataract could help in surgical planning. If 2D B-scan is not helpful, then a 3D USG can be opted for [3]. Even for determining the integrity of posterior capsule in posterior polar cataract, this can be very efficiently used as shown by Guo Y et al., [4]. Imaging techniques employed in present study could also perceive similar findings, excepting that present study was not done exclusively among cataract cases.
In a study done by Sandinha MT et al., on 58 patients to assess the accuracy of B-scan USG for acute FOVH they found that B-scan U/S scan was highly sensitive in identifying the pathology in acute FOVH and for new retinal tears (100%) [5]. Sensitivity found in present study was also very high (100%), similar to the findings by Sandinha MT et al., [5].
In another comparative study done by Yang Q-H et al., on alkali burn eyes, 56 cases were evaluated using both USG bio microscopy and immersion 20 MHz B-scan USG, and compared with intraoperative findings. Compared with the intraoperative findings, the diagnostic concordance rate of B-scan appearance of lens was 100% (56/56), which was significantly higher than when done by an Ultrasound Biomicroscopy (UBM) 57.14% (32/56) (p <0.01) [6]. Thus, B-scan USG is as good as other imaging techniques for diagnosing pathologies related to lens. This was however not an objective in present study and not captured.
In a study conducted by Mohamed IE et al., on 100 diabetic patients presenting with diabetic retinopathy using B-scan USG, it was seen that Vitreous Haemorrhage (VH) amounting to 42 cases (66.6%), was the most important cause of low vision in patients presenting with poorly or moderately regulated HbA1c. Other reasons like Asteroid Hyalosis (AH), Partial or Total Retinal Detachment (PRD/TRD), Posterior Vitreous Detachment (PVD), and CD were also found. They concluded that the non invasive procedure of ophthalmic B-mode USG can be used with minimum discomfort for Diabetic Retinopathy (DR) complications linked with the visual outcome of a diabetic case [16]. VH was also the commonest finding in present study, though there was poor representation of diabetes cases compared to the total sample.
In another study by Shazlee MK et al., in 2013-14 on the diagnostic accuracy of B-scan USG among ocular trauma cases using 10 MHz linear probe, a total of 61 patients with 63 ocular injuries were assessed, and it was seen that the overall sensitivity was 91.5%, with a specificity of 98.87%, a PPV of 87.62% and NPV was 99%. They concluded that B-scan USG is a sensitive, non invasive way to diagnose intra-ocular damage rapidly [17]. Sensitivity, specificity and NPVs was also similar in our study. However, positive predictive in our study was low as compared to the study conducted by Shazlee MK et al., [17].
In a study conducted by Neetam SBS et al., to assess the usefulness of high frequency real time USG to detect and characterise posterior chamber and extraocular pathologies, a total of 138 cases were studied. It was seen that the most common pathology in posterior segment in non traumatic eyes was retinal detachment while that in traumatic eyes was VH [18]. This finding was similar to present study as the most common findings.
In another study conducted by Kumar J et al., in 2017-18 on role of B-scan USG in evaluating posterior segment pathology of eye, it was seen that the most common indication for B-scan USG among 180 subjects was opaque media due to opacity of lens (52.5%). Majority of them (52.2%) did not show any posterior segment pathology using B-scan USG. The two most common pathology seen were retinal detachment and VH among those having posterior segment pathology [19]. Similarly in a cross-sectional study conducted among 136 patients eyes by Ansari AA et al., most common pathologies found were retinal detachment and VH [20]. Similar were the findings in the current study with retinal mass/detachment and VH being the most common among the posterior ocular pathologies.
In a comparative study of B-scan USG and optical coherence computerised tomography done by Kicova N et al., the posterior vitreous cortex was examined in 30 eyes among 30 patients presenting with macular pucker or macular hole, a day prior to a scheduled vitrectomy. It was seen that B-scan USG was the most reliable investigator-dependent prognostic method along with BM to clinically detect if the posterior vitreous cortex is detached [7]. Prognosis was not considered to be evaluated in present study, though preoperative assessment was a part of present study and routinely followed.
When fundus examination was not possible, USG is known to be a better method for investigation of possible retinal tears. In a study done by Streho M et al., it was further found that B-scan USG is able to detect superior retinal tears predominantly than in other quadrants (71% cases among the 101 eyes of 100 patients studied) [8].
Case studies published have also shown that USG B-scan is an indispensable tool for the diagnosis of ocular cysticercosis, locating masses/growths/tumours even in complete cataract cases, diagnosis of microvascular changes associated with optic disc drusen, etc., [21-23]. Similar posterior segment eye disorders were found to be present even in the current study.
In a study among 102 Sudanese adult patients with cataract done by Gareeballah A et al., sonographic findings showed PVD in 19.2%, VH of 0.98%, and complicated PVD in 1.96%. They also concluded that abnormalities of posterior segment should be evaluated by USG before surgery, especially cataract surgery [24]. Present study also inferred similar conclusions.
A sensitivity of 100% as found in the study indicates that all cases of posterior segment pathologies would be detected using B-scan USG, and almost none would be left undetected, thus making this a useful screening tool even in rural health care set-up. This has also been recommended by several authors [1,25]. The adjusted specificity of 100% indicates that it is also a suitable method for confirmation of diagnosis.
The LRs are one of the best ways to know the diagnostic accuracy [9]. It is the likelihood of a given test result in patient with a disease compared to the likelihood in a patient without the disease. The LR is used to assess and select a diagnostic test or sequence of tests. As compared to sensitivity and specificity, they are more or less stable with changes in prevalence of the disorder, and they can be used to calculate post-test probability of a disease using the test [10]. In present study we had a very high adjusted LR+ (LR+=∞) and a very low LR- (LR-=0), which qualitatively are said to be excellent for prediction of positive and negative test results. The prevalence of diagnosing a posterior segment pathology at the tertiary care centre was found to be 13.1%, which means using reference test technique posterior segment pathology would be detected in 13 cases out of 100 presenting referral cases from ophthalmology department. However, using B-scan USG the post-test probability increased to 46.6%, i.e., the detection of posterior segment pathology would increase to 46 or more out of 100 such cases referred from the ophthalmology department. This finding has never been presented in any study till date, to the best of the knowledge of the authors.
The classical method for diagnosis of accuracy has got deviations in two forms- the first situation where there is no reference test (e.g., a situation where a new test is developed for a newly developed test or there was no reference test that could be fixed till date or people could not opt for this test due to some medical reasons) and the second where the reference test is not a perfect reference test (due to presence of misclassification error) [26]. The study has thus considered this situation, and made adjustment accordingly during analysis [13,27].
The study recommends using B-scan USG as a faster, easier and accurate method to screen subjects with suspected posterior segment pathology and also for screening during follow-up in diseases with possible ophthalmoscopic complications (like Diabetes, Hypertension, etc.,). The frequency of follow-up for screening these subjects is scope for future research. The study also recommends employing B-scan USG at rural health centres by trained and qualified personnel for screening potential posterior segment eye diseases in its catchment population.
Limitation(s)
Adjustment had to be made for cases that could not be diagnosed using reference test (due to conditions in anterior chamber of eye), but could be diagnosed using the new test, to avoid verification bias. This could have been done at the planning stage through inclusion/exclusion criteria allowing only subjects whose verification could be done using both methods. Adjustments were done during analysis using bias correction methods [13].
Conclusion(s)
Prevalence of PSD was 13.1% for cases referred to radiology department. The most common PSD found was retinal mass. Absence of posterior segment disorder using B-scan USG is very helpful in ruling out disease entirely as it has a 100% sensitivity, specificity and NPV. Post-test probability was infinite after adjustment. Adjusted accuracy was 100%. Using B-scan ultrasonography for preoperative assessment and confirmation of diagnosis increases the probability of detecting presence or absence of posterior segment pathology. It also has a very high sensitivity and hence has a scope to be used even in rural health centres for screening.
CD+VH: Choroidal detachment with vitreous haemorrhage; N: Normal; ND: Not done; RD: Retinal detachment; RM: Retinal mass; SL: Subluxated lens; VH: Vitreous haemorrhage
TP: True positive; FP: False positive; FN: False negative; TN: True negative