The control of communicable diseases and increase in life expectancy due to modified life styles have resulted in increased incidence of Non Communicable Diseases (NCDs) and, thereby, responsible for more than 70% of deaths and more than 80% of Years Lived with Disability (YLD) [1]. Cardiovascular Diseases (CVD) are a leading cause of death in India involving every class across the social divide and not necessarily those belonging to affluent class as is generally believed [2]. The estimate of age-standardised CVD death rate of 272 per 100,000 population in India is higher than the global average of 235 per 100,000 population [3]. Interestingly, whereas the death rate due to CVD declined by 41% in United States between 1990-2016, in India it rose by 34% from 155.7-209 one death per 100,000 population in the same period and also the CVD is somewhat different from western countries, in India as it shows accelerated course, the early age of onset and the high case fatality rate [3].
In all these years, the prevalence of ischaemic heart disease is increasing and more patients visit the hospital emergency departments with acute coronary events, as a result of which the prognosis is poor in some patients as compared to others [4,5]. It is, therefore assumed that other factors (apart from the patient’s baseline characteristics and traditional risk factors), also play a role in influencing the course of illness in hospital and in immediate postdischarge phase [6].
There has been an ongoing debate on the role of calcium in pathogenesis of vascular diseases but lately, serum calcium levels as an important determinant in acute events was established. Yan SD et al., concluded that lower serum calcium level is a possible indicator of mortality in ACS patients [6]. The extra-skeletal calcium plays a critical role in cardiac contraction, cardiomyocyte apoptosis, electrophysiology of the heart, coagulation pathway and platelet function mediated via the calcium-sensing receptor and in neurotransmitter release, enzyme activity regulation, and blood pressure regulation association [7,8]. Hence, of the present study was to evaluate impact of baseline serum calcium levels in patients with ACS and to determine prognostic significance of baseline serum calcium levels in patients with ACS.
Materials and Methods
This was a single-centre, prospective, observational study conducted in a tertiary care centre, over a period of one year from December 2018 to December 2019 at Acharya Shri Chander College of Medical Sciences, Sidhra, Jammu and Kashmir, India. involving 100 diagnosed cases of ACS vide IEC number ASCOMS/IEC/RP&T/2018/288. A written informed consent was obtained from all patients after explaining to them the nature and purpose of the study. ACS was diagnosed according to the criteria defined by the World Health Organisation (WHO) [9].
Inclusion criteria: Patients with hypocalcaemia and aged 50-80 years and with normal renal functions tests, with no thyroid abnormality and having no history of malignancy were included in the present study.
Exclusion criteria: Patients with renal dysfunction {estimated glomerular filtration rate (eGFR) <60 mL/min)}, parathyroid disease, evidence of infection within last 2 weeks, history of malignancy within last 3 years, major trauma or surgery within 4 weeks before admission, patients on calcium and vitamin D supplements and those with hepatic dysfunction were excluded from the study. After serial 12 lead electrocardiogram monitoring and troponin t-test, all routine biochemical tests, baseline serum calcium and albumin levels were done at the time of admission. All serum calcium levels for each patient were corrected for albumin using following formula:
Corrected calcium (mg/dL)=measured total Ca (mg/dL)+0.8 {4.0-serum albumin (g/dL)}, where 4.0 represents the average albumin level. Patients were divided into three tertile ranges depending upon the corrected calcium levels in mg/dL [10].
hypocalcaemic (<8.1);
normocalcaemic (8.1–10.4);
hypercalcaemic (>10.4).
Patients were followed-up for 90 days through routine Outpatient Department (OPD) examinations and hospital medical records.
Statistical Analysis
Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected then non parametric test was used. Statistical tests were applied as follows-Quantitative variables were compared using ANOVA/Kruskal Wallis Test (when the data sets were not normally distributed) between the three groups. The R (version 3.4.1) software was used for managing the data, generating plots, and performing the statistical analyses. Two-sided p-values <0.05 were considered statistically significant for all estimates.
Results
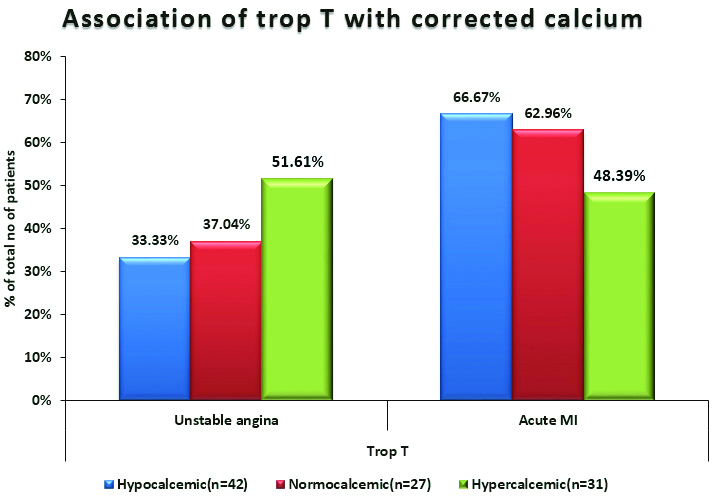
In the present study, mean age of the population was 73.29±8.11 years. Out of a total of 100 patients, 40 patients were of unstable angina and 60 were of Acute MI (AMI). It was observed that 64% of the patients in hypocalcaemia tertile (n=14) were males in unstable angina group and overwhelming 78.57% in AMI. On admission, troponin T levels were positive in 66.67% patients of AMI with low baseline serum calcium levels and 33.33% in patients with unstable angina [Table/Fig-1].
Association of troponin T with corrected calcium.
The highest BMI was found to be 27.38 kg/m2 in hypocalcaemic group with mean age of 73.29 years among AMI patients [Table/Fig-2]. Mean systolic and diastolic blood pressure found to be lower in hypocalcaemic patients in both unstable angina and AMI [Table/Fig-3]. Hypocalcaemic patients requiring emergency revascularisation in unstable angina patients and AMI were 35.71% and 21.43%, respectively. Normocalcaemic patients requiring emergency revascularisation in unstable angina patients and AMI were 70% and 76.47%, respectively. Hypercalcaemic patients requiring emergency revascularisation in unstable angina patients and AMI were 75% and 73.33%, respectively [Table/Fig-4].
Association of baseline characteristics with corrected calcium in unstable angina and AMI.
| Baseline characteristics | Corrected calcium (mg/dL) in unstable angina | Corrected calcium (mg/dL) in AMI |
|---|
| Hypocalcaemic (n=14) | Normocalcaemic (n=10) | Hypercalcaemic (n=16) | Hypocalcaemic (n=28) | Normocalcaemic (n=17) | Hypercalcaemic (n=15) |
|---|
| Age in years |
| Mean (SD) | 72.21 (7.53) | 63.3 (7.66) | 54.62 (7.9) | 73.29 (8.11) | 54.71 (5.88) | 56.6 (9.5) |
| Median (IQR) | 73 (66-78) | 63 (58-70) | 54 (49-61) | 75 (68- 78.500) | 55 (49.750-57.250) | 56 (49.250-61.500) |
| p-value | <0.0001 | <0.0001 |
| Gender |
| Female | 5 (35.71%) | 9 (90.00%) | 7 (43.75%) | 6 (21.43%) | 8 (47.06%) | 8 (53.33%) |
| Male | 9 (64.29%) | 1 (10.00%) | 9 (56.25%) | 22 (78.57%) | 9 (52.94%) | 7 (46.67%) |
| p-value | 0.021 | 0.068 |
| Body mass index (BMI) (kg/m2) |
| Mean (SD) | 26.19 (3.3) | 25.55 (3.18) | 26.84 (3.62) | 27.38 (4.04) | 24.52 (2.26) | 25.98 (2.9) |
| Median (IQR) | 26.01 (24.090-29.720) | 24.93 (24.090-26.400) | 26.06 (23.915-30.450) | 27.19 (23.225-30.800) | 24.22 (23-24.875) | 25.03 (24.977-27.578) |
| p-value | 0.642 | 0.026 |
p-value <0.05 was considered statistically significant
Association of haemodynamic parameters with corrected calcium in unstable angina and AMI.
| Haemodynamic parameters | Corrected calcium (mg/dL) in unstable angina | Corrected calcium (mg/dL) in AMI |
|---|
| Hypocalcaemic (n=14) | Normocalcaemic (n=10) | Hypercalcaemic (n=16) | Hypocalcaemic (n=28) | Normocalcaemic (n=17) | Hypercalcaemic (n=15) |
|---|
| Systolic blood pressure (mmHg) |
| Mean (SD) | 112.14 (21.11) | 131.8 (24.54) | 134.88 (13.29) | 107.29 (14.27) | 134.59 (16.03) | 136.8 (19.17) |
| Median (IQR) | 108 (94-130) | 132 (110-150) | 139 (126 - 143) | 109 (94-120) | 130 (128.500-148) | 130 (123.500-140) |
| p-value | 0.007 | <0.0001 |
| Diastolic blood pressure (mmHg) |
| Mean (SD) | 72.86 (11) | 77.4 (14.7) | 85.88 (7.5) | 69.21 (10.67) | 89.65 (13.46) | 86.27 (6.54) |
| Median (IQR) | 72 (70-82) | 79 (62-82) | 88 (81-92) | 69 (60-80) | 90 (82-100) | 84 (82-89) |
| p-value | 0.004 | <0.0001 |
| Heart rate (bpm) (at the time of admission) |
| Mean (SD) | 85.43 (14.32) | 77.4 (9.14) | 89 (10.48) | 87.29 (9.77) | 74.71 (10.44) | 84.8 (8.61) |
| Median (IQR) | 84 (72-98) | 76 (74-86) | 92 (84-98) | 89 (82-94) | 72 (67.50-80.50) | 86 (78-91.50) |
| p-value | 0.059 | 0.0003 |
p-value <0.05 was considered statistically significant
Association of emergency revascularisation with corrected calcium in unstable angina and AMI.
| Emergency revascularisation | Corrected calcium (mg/dL) in unstable angina | Corrected calcium (mg/dL) in AMI |
|---|
| Hypocalcaemic (n=14) | Normocalcaemic (n=10) | Hypercalcaemic (n=16) | Hypocalcaemic (n=28) | Normocalcaemic (n=17) | Hypercalcaemic (n=15) |
|---|
| No | 9 (64.29%) | 3 (30%) | 4 (25%) | 22 (78.57%) | 4 (23.53%) | 4 (26.67%) |
| Yes | 5 (35.71%) | 7 (70%) | 12 (75%) | 6 (21.43%) | 13 (76.47%) | 11 (73.33%) |
| p-value | 0.069 | 0.0002 |
p-value <0.05 was considered statistically significant
Median LVEF of hypocalcaemic, normocalcaemic and hypercalcaemic in unstable angina was 29%, 45% and 55% and in AMI was 30%, 48% and 55%, respectively. Thus, inference can be made that LVEF is significantly lower in hypocalcaemic patients as compared to hypercalcaemic patients [Table/Fig-5].
Association of complications with corrected calcium in unstable angina and AMI.
| Complications | Corrected calcium (mg/dL) in unstable angina | Corrected calcium (mg/dL) in AMI |
|---|
| Hypocalcaemic (n=14) | Normocalcaemic (n=10) | Hypercalcaemic (n=16) | Hypocalcaemic (n=28) | Normocalcaemic (n=17) | Hypercalcaemic (n=15) |
|---|
| LVEF (%) |
| Mean (SD) | 33.43 (15.53) | 47.5 (12.08) | 52.75 (10.02) | 33.43 (14.74) | 49.65 (10.45) | 53.8 (8.2) |
| Median (IQR) | 29 (20-48) | 45 (40-60) | 55 (45-60) | 30 (20-45) | 48 (40-60) | 55 (49.750-60) |
| p-value | 0.006 | 0.0001 |
| Acute pulmonary oedema |
| Yes | 7 (50%) | 3 (30%) | 3 (18.75%) | 15 (53.57%) | 4 (23.53%) | 2 (13.33%) |
| p-value | 0.186 | 0.016 |
| Arrhythmias |
| Yes | 7 (50%) | 1 (10%) | 3 (18.75%) | 11 (39.29%) | 5 (29.41%) | 4 (26.67%) |
| p-value | 0.058* | 0.649* |
| Recurrence of chest pain |
| Yes | 6 (42.86%) | 3 (30%) | 3 (18.75%) | 15 (53.57%) | 7 (41.18%) | 3 (20%) |
| p-value | 0.356 | 0.104 |
p-value <0.05 was considered statistically significant
Acute pulmonary oedema was present more in hypocalcaemic patients with unstable angina and AMI as compared to that of normocalcaemic and hypercalcaemic patients [Table/Fig-5]. Recurrence of chest pain was higher in hypocalcaemic patients with unstable angina and AMI as compared to that of normocalcaemic and hypercalcaemic patients, respectively [Table/Fig-5].
Days of hospitalisation were higher in hypocalcaemic patients with unstable angina and AMI as compared to that of normocalcaemic and hypercalcaemic patients [Table/Fig-6].
Association of outcome with corrected calcium in unstable angina and AMI.
| Outcome | Corrected calcium (mg/dL) in unstable angina | Corrected calcium (mg/dL) in AMI |
|---|
| Hypocalcaemic (n=14) | Normocalcaemic (n=10) | Hypercalcaemic (n=16) | Hypocalcaemic (n=28) | Normocalcaemic (n=17) | Hypercalcaemic (n=15) |
|---|
| Days of hospitalisation |
| Mean (SD) | 8.64 (2.21) | 5.1 (0.99) | 5.06 (0.68) | 8.82 (2.26) | 5.53 (0.94) | 5.47 (0.83) |
| Median (IQR) | 8.5 (7-10) | 5.5 (4-6) | 5 (5-5.500) | 9.5 (7 - 10.500) | 6 (5-6) | 6 (5-6) |
| p-value | <0.0001 | <0.0001 |
| Mortality within 7 days of admission |
| Yes | 5 (35.71%) | 1 (10%) | 2 (12.50%) | 10 (35.71%) | 2 (11.76%) | 1 (6.67%) |
| p-value | 0.187 | 0.044 |
| Readmission rate |
| Yes | 6 (42.86%) | 2 (20%) | 1 (6.25%) | 13 (46.43%) | 2 (11.76%) | 2 (13.33%) |
| p-value | 0.055 | 0.014 |
| Mortality within 90 days |
| Yes | 6 (42.86%) | 2 (20%) | 1 (6.25%) | 11 (39.29%) | 2 (11.76%) | 2 (13.33%) |
| p-value | 0.055 | 0.057 |
p-value <0.05 was considered statistically significant
Mortality within 90 days of follow-up was higher in hypocalcaemic patients (42.86%) as compared to normocalcaemic (20%) and hypercalcaemic (6.25%) patients with unstable angina and also higher for hypocalcaemic patients with AMI [Table/Fig-6].
Discussion
The present study conducted to determine prognostic significance of baseline serum calcium levels in patients with ACS. Findings revealed that the serum calcium level is an independent predictor of the cause midterm mortality risk in ACS patients. Serum calcium levels are an independent risk factor for in-hospital mortality in acute myocardial infarction [5,6]. The low serum calcium levels may influence the cardiac electrophysiology by reducing the calcium influx through the L-type calcium channel, leading to reduced plateau depolarisation and a shortened cardiac action potential. The hypocalcaemia also causes QT prolongation and has postulated to facilitate the development of cardiomyopathy and heart failure, both ultimately leading to poorer outcomes [7,10]. It has also been hypothesised that an increasing level of intracellular calcium in platelet results in increased consumption of calcium, resulting in hypocalcaemia, the assumption being that low calcium level might partially reflect worsened vascular condition in patients of ACS leading to poor outcome [7,10]. Hypertension, hyperlipidemia, diabetes, smoking, age, and sex are generally are some confounding factors for CVD [11,12,13].
On admission, troponin T levels were positive in 66.67% patients of AMI with low baseline serum calcium levels and 33.33% in patients with unstable angina [Table/Fig-1]. Hypocalcaemia was documented in 49% cases in a study conducted by Patil S et al., [14]. Significant association was seen between age and corrected calcium in unstable angina patients and AMI patients as also by other authors, indicating that patients in lower quartiles of calcium are older [9,15]. In the present study, mortality within 90 days of follow-up was higher in hypocalcaemia group but overall, the distribution was comparable. Study conducted by Akirov A et al., and also reported similar findings [16]. In the present study, significant association was seen between gender and corrected calcium in unstable angina but not in AMI. Sathyamurthy I et al., and Gomez Alvarez Z et al., reported that males constituted 92% and 76% of their patients with hypocalcaemia, respectively [17,18]. The significant association was seen between BMI and corrected calcium in AMI but not in in unstable angina, in the present study. Meiling J et al., found that hypocalcaemia was predominant in obese individuals with high BMI who were also dyslipidemic [19].
Significant association was also seen between blood pressure and corrected calcium in AMI. However, in a similar study, Meiling J et al., reported no such difference. (p>0.05) [19]. Significant association was seen between heart rate at admission and corrected calcium in AMI (p<0.05) Meiling J et al., also found higher baseline heart rates more in patients with hypocalcaemia, but that was statistically not significant. Thus, blood pressure and heart rates are not shown to significantly associated with corrected calcium levels.
Again, significant association was seen between emergency revascularisation and corrected calcium in AMI but not in unstable angina. The larger percentage of hypocalcaemic subjects were not stable haemodynamically to undergo emergency revascularisation and less percentage is also associated with worse outcome as in some patients’ revascularisation could improve myocardial salvage. In unstable angina and AMI, the LVEF was significantly lower in patients with hypocalcaemia, similar to that seen by Meiling J et al., but not by Lu X et al., [19,20]. The complication of acute pulmonary oedema was significantly more in those with hypocalcaemia in AMI but not in unstable angina. Gomez Polo J et al., and Obradovic S et al., also reported similar findings [21,22].
In both, unstable angina and in AMI incidence of arrhythmias didn’t differ significantly in patients within three tertiles in the present study. In comparison, Gomez Alvarez Z et al., and Gomez Polo JC et al., reported more patients of sustained ventricular arrhythmias and atrioventricular block and Yarmohammadi H et al., found sudden cardiac arrest more common in patients with hypocalcaemia [18,21,23]. The recurrence of chest pain was comparable in both unstable angina and AMI with no significant association with calcium levels.
Kumar S and Saxena P, found higher risk for several in-hospital complications in their study [24]. Days of hospitalisation were significantly longer in hypocalcaemic patients as compared to normocalcaemic and hypercalcaemic patients in both unstable angina and AMI. The findings are in contrast to those reported by Lu X et al., [20]. There is very limited research which describe the association between serum calcium levels and mortality at the end of first 7 days; which was higher in hypocalcaemic patients with AMI but overall, the distribution was comparable in unstable angina. The readmission rate in AMI was significantly more in hypocalcaemic group but not in unstable angina. Obradovic S et al., reported similar correlation [22].
The present study didn’t find significant association between mortality within 90 days of follow-up and corrected calcium in unstable angina and in AMI. However, Gomez Alvarez Z et al., Lu X et al., Sauter TC et al., and Miura S et al., found in-hospital mortality significantly higher in hypocalcaemics (12.7%) as compared to normocalcaemics (6.5%) and hypercalcaemics subjects (2.9%) [18,20,25,26].
Limitation(s)
The study evaluated serum calcium only at the time of admission, but serum calcium levels may vary over time. Although, numerous relevant points were considered some potential confounders (e.g., vitamin D, bone metabolites, and thyroid hormones) were not considered. Present study revealed that serum calcium can be used as an available biomarker in the midterm risk stratification of patients with ACS. Further studies can be done to clarify the underlying mechanisms and to determine how therapy affecting serum calcium levels can improve the prognosis.
Conclusion(s)
In order to identify patients with potential outcomes early, the measurement of total serum calcium is an easy and economical strategy as soon as the initial management of the patient is started. This is especially important in a country like India with limited healthcare facilities and resource as there is need for appropriate triage and clinical resource utilisation including decisions regarding transfer to tertiary centres and for early hospital discharge in low-risk patients.
p-value <0.05 was considered statistically significant
p-value <0.05 was considered statistically significant
p-value <0.05 was considered statistically significant
p-value <0.05 was considered statistically significant
p-value <0.05 was considered statistically significant