Surgical Removal of Impacted Mandibular Third Molar (SIM3M) is regarded as one of the most frequently performed minor surgical procedures in oral surgery. SIM3M is classified as a part of clean-contaminated group of surgeries [1]. Various studies have evaluated the sequelae following third molar surgery namely swelling, pain, bleeding, alveolar osteitis, abscesses, dehiscence, paresthesia, haematoma, and trismus [2-5]. Prophylactic antibiotic therapy is defined as the administration of any antimicrobial agent that prevents the development of infection [6]. Some authors prefer routine antibiotic prophylaxis [5,7-10] while others suggest it might be useful only in difficult cases or of no use at all [1,11,12]. According to Lockhart PB et al., they have recommended antibiotic usage for pulpal necrosis and localised acute apical abscess where definitive conservative dental treatment is not available in immunocompetent patients [13].
The aim of prophylactic antibiotic is to have adequate level of antibiotic in the tissue prior to incision, thus reducing chances of postoperative complications. Postoperative antibiotics without preoperative administration are questionable [14]. Some authors suggest postsurgical infection rate is low for routine antibiotic administration after SIM3M [15,16]. Extended or inappropriate antibiotic regimen can lead to acquired drug resistance [17]. Literature reveals that indiscriminate use of antibiotic prophylaxis is not just unscientific but can be harmful leading to adverse effects, advent of multidrug resistance and cross resistant microorganisms [17,18]. This study was carried out with the aim of determining the type of suitable antibiotic regimen for SIM3M. The objective of this study was to compare the effectiveness of single dose preoperative i.v. antibiotic therapy with 5 days postoperative Per Oral (PO) antibiotic therapy in patients undergoing SIM3M. Variables measured in the study were surgical site infection and alveolar osteitis in both groups.
Materials and Methods
This double armed randomised clinical trial with split mouth design was conducted at JSS Dental College and Hospital, Mysuru, Karnataka, India, during the period of August 2020 to April 2021. This study was registered under Clinical Trial Registry of India, CTRI registration number was CTRI/2020/07/026722 and the acknowledgement no is REF/2020/07/035126. The study was approved by Institutional Ethical Committee (JSSDCH IEC research protocol no:10/2018) and a written informed consent was signed by all participants included in the study. The study was conducted in accordance with Helsinki Declaration of 1975, revised in 2000.
Inclusion criteria: Both male and female patients belonging to the age group of 18-45 years with bilaterally impacted mandibular third molars, systemically healthy patients who had not undertaken antibiotics or anti-inflammatory drugs within two weeks before the procedure and patients who were willing to give their consent for their participation were eligible for the study.
Exclusion criteria: Patients presenting with local pathology like cyst/tumour associated with third molar, patients with other systemic illness and immunocompromised patients, patients allergic to amoxicillin, pregnant patients, patients presenting with abscess or cellulitis, non compliance of patient in taking postoperative medication, known allergy to lignocaine and inability to appear for follow-up were excluded.
Sample size calculation: Sample size was calculated using formula

where s is the sample size, z is the standard normal deviate set at 1.96, p is the prevalence rate set at 8% [19] and q is 1-p with a margin of error (d) set at 10% giving a sample size of 28 which was rounded off to 30.
Balanced randomisation between the two groups was used, with blocks of 4. Group A patients were treated with postoperative per oral antibiotics and Group B using preoperative single dose i.v. antibiotics.
Interventions
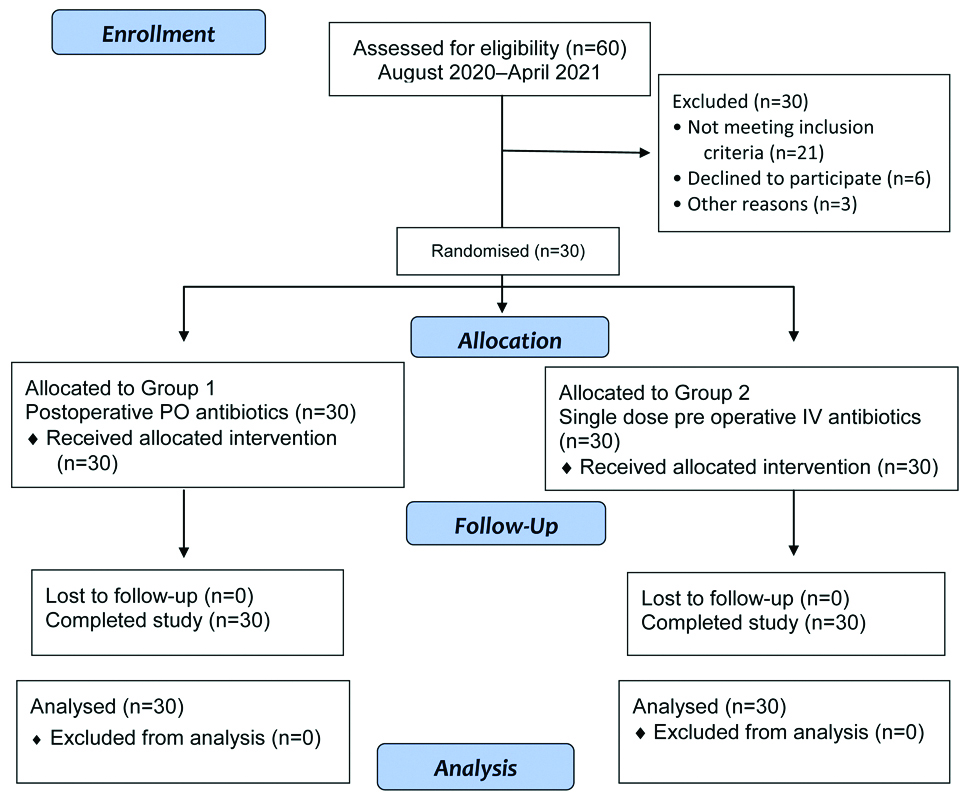
Each subject acted as his/her own control and were randomly allocated into two groups in which the impacted tooth on one side was treated with conventional post-surgical postoperative antibiotics (cap. amoxicillin 500 mg thrice daily for 5 days) representing Group-A and the impacted 3rd molar on the other side was removed after 2 weeks with a single-dose preoperative i.v. antibiotic (inj. amoxicillin 1 gm) 1 hour before the procedure(Group-B) after test dose [Table/Fig-1]. Type of impactions on right and left-sides were recorded [Table/Fig-2]. The impaction kits were sterilised at central sterilisation supply department of our college and sterilisation validation was done by using biological and chemical indicators regularly.
Inj. amoxicillin 500 mg with sterile water.

Type of impactions on right and left-side.
| Tooth | Number | Percentage | Cumulative percentage |
|---|
| Left | V | 5 | 16.7 | 16.7 |
| M | 7 | 23.3 | 40.0 |
| D | 7 | 23.3 | 63.3 |
| H | 11 | 36.7 | 100.0 |
| Total | 30 | 100.0 | |
| Right | V | 6 | 20.0 | 20.0 |
| M | 5 | 16.7 | 36.7 |
| D | 9 | 30.0 | 66.7 |
| H | 10 | 33.3 | 100.0 |
| Total | 30 | 100.0 | |
V: Vertical; M: Mesioangular; D; Distoangular; H: Horizontal
A 2% specify was used as local anaesthesia. Classic inferior alveolar, lingual and long buccal nerve blocks were given. Teeth were surgically removed with or without teeth sectioning. Postoperative instructions given to patients were to bite on the cotton gauze firmly for 10-20 minutes, to avoid spitting for 24 hours, to continue prescribed medications regularly, to apply ice pack extra orally within 24 hours of surgery, to carry out warm saline rinsing after 24 hours of surgery and to refrain from smoking and vigorous oral rinsing. Acetaminophen 500 mg twice daily for 5 days was the analgesic regimen used for all patients in both groups. Patients were evaluated on the 3rd, 7th and 14th postoperative day for outcome variables namely, surgical site infection and alveolar osteitis. These variables were depicted as a binary outcome that is complication present or absent. Same surgeon performed the procedure in all the patients.
Two primary outcome variables assessed in this study were surgical site infection and alveolar osteitis.
Surgical site infection (SSI): The diagnosis of SSI was made if there was visual evidence of parameters like erythema, oedema, presence of Purulent Discharge (PD) in the extraction site. Oedema [1,11,20-26], erythema [1,25] and presence of PD [1,23,25-28] were the parameters assessed for diagnosing SSI following SIM3M. Presence of PD alone or PD in combination with other parameters was considered as an indicator of SSI. Increase in pain from 3rd-10th postoperative days, persistence or increase in swelling during 4th-10th postoperative days and PD from the surgical site postoperatively were noted.
Alveolar Osteitis (AO): The diagnosis of AO was made if there was a new onset or increasing pain more than 36 hours after the procedure and by examination, there was a loss of the blood clot in the surgical site as evidenced by exposed bone [8]. Pain more than 36 hours [5,8,9], LOBC [1,8,9,25,29] and EEB [1,8,29,30] are the most commonly assessed parameters in literature. All elements needed to be present to make the diagnosis of AO.
Statistical Analysis
All the statistical methods were carried out through the Statistical Package for the Social Sciences (SPSS) for Windows (version 20.0). The descriptive procedure displays univariate summary statistics for several variables in a single table and calculates standardised values (z scores). Variables can be ordered by the size of their means (in ascending or descending order), alphabetically, or by the order in which the researcher specifies. The outcome variables namely alveolar osteitis and surgical site infection was assessed using Chi-square test. All statistical analyses were carried out at 5% level of significance and p-value of <0.05 was considered as statistically significant.
Results
The baseline demographic characteristics of the 30 patients who participated in the study have been included in the flow diagram [Table/Fig-3]. No patients dropped out from the study and were followed-up for a period of two weeks.
CONSORT flow diagram.
PO: Per oral; IV: Intravenous
Amongst 30 patients selected for this study, 14 (46.7%) were females and 16 (53.3%) were males with a mean age of 25.17±5.74 years [Table/Fig-4].
Frequency distribution of demographic data.
| Variables | Number | Percentage | Mean age (years) | Standard deviation |
|---|
| Gender | Male | 16 | 53.3 | 25.17 | 5.74 |
| Female | 14 | 46.7 |
| Total | 30 | 100.0 |
Primary outcome variables assessed in this study are surgical site infection and alveolar osteitis. No subject showed SSI among both the groups.
In this study, 23 subjects (76.7%) in group A had oedema on the 3rd postoperative day, 3 subjects (10%) on the 7th postoperative day and no patients on the 14th postoperative day. Whereas in group B, 21 subjects (70%) had oedema on 3rd postoperative day, 1 patient (3.3%) on 7th postoperative day and no patients on 14th postoperative day which was not significant [Table/Fig-5]. The combined statistical analysis of all the 3 sessions namely 3rd, 7th and 14th postoperative days revealed a Chi-square value of 50.733 for group A and 50.655 for group B with a degree of freedom of 2, p-value of 0.001 was arrived, which is statistically significant [Table/Fig-6].
Evaluation of outcome variables and their parameters during each session, Only present cases have been considered.
| Parameters | Group | | Sessions |
|---|
| Day 3 | Day 7 | Day 14 |
|---|
| Surgical site infection | A | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| B | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| p-value (Chi-square test) | | | Nil | Nil | Nil |
| Oedema | A | Frequency | 23 | 3 | 0 |
| Percent | 76.7% | 10% | 0% |
| B | Frequency | 21 | 1 | 0 |
| Percent | 70% | 3.3% | 0% |
| p-value (Chi-square test) | | | 0.559 | 0.301 | Nil |
| Erythema | A | Frequency | 25 | 3 | 0 |
| Percent | 83.3% | 10% | 0% |
| B | Frequency | 19 | 2 | 0 |
| Percent | 63.3% | 6.7% | 0% |
| p-value (Chi-square test) | | | 0.80 | 0.640 | Nil |
| Purulent discharge | A | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| B | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| p-value (Chi-square test) | | | Nil | Nil | Nil |
| Alveolar osteitis | A | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| B | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| p-value (Chi-square test) | | | Nil | Nil | Nil |
| Pain more than 36 hours | A | Frequency | 18 | 2 | 0 |
| Percent | 60.0% | 6.7% | 0% |
| B | Frequency | 15 | 0 | 0 |
| Percent | 50% | 0% | 0% |
| p-value (Chi-square test) | | | 0.436 | 0.150 | Nil |
| Loss of blood clot | A | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| B | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| p-value (Chi-square test) | | | Nil | Nil | Nil |
| Evidence of exposed bone | A | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| B | Frequency | 0 | 0 | 0 |
| Percent | 0% | 0% | 0% |
| p-value (Chi-square test) | | | Nil | Nil | Nil |
Group A- Postoperative group, Group B- Preoperative group
Cumulative p-values of 3rd, 7th and 14th postoperative day sessions.
| Parameter | Groups | Chi-square value | Total Chi-square value | Degree of freedom | p-value |
|---|
| Oedema | A | 50.733 | 100.909 | 2 | 0.001 |
| B | 50.655 |
| Erythema | A | 57.961 | 97.641 | 2 | 0.001 |
| B | 40.621 |
| Pain more than 36 hours | A | 37.543 | 72.851 | 2 | 0.001 |
| B | 36.000 |
Group A- Postoperative group, Group B- Preoperative group
Twenty five subjects (83.3%) in group A and 19 subjects (63.3%) in group B had erythema on the 3rd postoperative day, 3 subjects (10%) in group A and 2 (6.7%) in group B on the 7th postoperative day and no patient had erythema on the 14th postoperative day in both groups [Table/Fig-5] which was not statistically significant. The combined statistical analysis of all the 3 sessions namely 3rd, 7th and 14th postoperative days revealed a Chi-square value of 57.961 for group A and 40.621 for group B with degree of freedom of 2 giving a p-value of 0.001 which is statistically significant [Table/Fig-6].
No subject had the incidence of Purulent Discharge (PD) among both groups.
In this study, no subject experienced AO among both groups A and B. Pain greater than 36 hours was noted in 18 subjects (60%) in group A and 15 subjects (50%) in group B on the 3rd postoperative day, 2 subjects (6.7%) in group A and no patients (0%) in group B on the 7th postoperative day and no patient experienced pain greater than 36 hours on the 14th postoperative day which was not statistically significant [Table/Fig-5]. The combined statistical analysis of all the 3 sessions namely 3rd, 7th and 14th postoperative days revealed a chi-square value of 37.543 for group A and 36.000 for group B with a degree of freedom of 2 revealing a p-value of 0.001 which is statistically significant [Table/Fig-6].
In this study, no subject experienced LOBC or EEB among of both groups. There was no statistically significant difference between the 2 antibiotic regimens employed when the variable of SSI and AO were evaluated on the 3rd, 7th and 14th postoperative days [Table/Fig-5].
Discussion
Surgical wounds maybe classified into clean, clean contaminated, contaminated and dirty wounds by the National Research Council [31]. SIM3M is classified as part of the clean-contaminated group of surgeries [1]. The reasons for SIM3M involves existing pathology or pain due to pericoronitis, periodontitis, periapical abscess, cysts or neoplasms, resorption of adjacent roots, and inflammation of the opposing soft tissue, prosthetic and orthodontic reasons [32].
Oral infections are caused by a plethora of microorganisms where anaerobes outnumber aerobes by 2:1 [33]. The bacteria responsible for causing oral infections are predominantly.
Aerobic Gram positive cocci (Streptococcus viridans gp.).
Anaerobic Gram negative cocci (peptococci and peptostreptococci).
Anaerobic Gram negative rods (Prevotella melaninogenicus and Fusobacterium nucleatum).
It has been proven that pure anaerobic strains when introduced into an environment does not cause infection as they require aerobic microorganisms to grow [34,35]. This has led to the foundation of antibiotic prophylaxis that is effectiveness against aerobes is sufficient and total effectiveness against anaerobic organisms may not be necessary [36].
Oral surgeries are carried out in an environment where large number of bacteria exists, predisposing to postoperative infection. This along with evidence on improved health related quality of life with i.v. antibiotics [10] could be the benefits of antibiotic use in minor oral surgery.
Bacterial resistance to antibiotics has been a perceived reality nearly since the beginning of antibiotic era, yet just within the past twenty years has the emergence of dangerous, resistant microorganisms occurred with a disturbing regularity [17]. This antibiotic resistance along with decreased antibiotic advent will eventually lead to a post-antibiotic era [37].
Prophylactic antibiotic therapy is defined as ‘the administration of any antimicrobial agent that prevents the development of infection [5]. For effective prophylaxis, the antibiotic agent employed must have adequate bone penetration, should be widely distributed in the body fluids and should be active against microorganisms [38]. For any infection, the antibiotic considered should possess bactericidal activity, spectrum should be as narrow as possible to prevent incidence of resistant micro organisms and should be the least toxic agent available with adequate potency [15].
In transoral procedures, penicillin is the drug of choice for prophylaxis as it is bactericidal, non toxic and effective against the infectious oral microflora [39]. In our study, amoxicillin was used in both injectable and oral preparations as an antibiotic. Various antibiotic regimes have been followed in minor oral surgery such as:
1) Antibiotic therapy immediately after surgery and maintenance for several days [1,5,9,11,27,40].
2) Prophylactic antibiotic administration before surgery as a single dose or multiple doses several days preoperatively [3,8,40-45].
3) Administration of the antibiotic preoperatively and maintained after surgery [12,15,41,42,46].
Some studies also have suggested that routine use of antibiotic prophylaxis for third molar surgery is unnecessary [1,11,13]. There are evidence that both supports [3,7,20,47-50] and questions [11,18,41,50] the benefits of routine prophylactic antibiotic therapy in reducing risk of postoperative complications like infection [4]. Infectious complications may be due to the position and anatomy of the third molar [51], trauma and surgical time needed, or to the surgeon’s experience [52].
According to Rothaug J et al., binary answering format has proven to be a reliable alternative method to numerical rating scales in a study of 430 patients from 3 different surgical disciplines which included oral and maxillofacial surgery [53]. On measurement of pain interference, the binary method achieved equal test-retest reliability, an equal validity, and a slightly lower internal consistency.
Hence, the primary outcome variables of SSI and AO were assessed in this study based on parameters depicted as binary answers (present/absent).
Surgical Site Infection (SSI): According to Halpern LR and Dodson TB, they found that 8.5% cases developed SSI when subjected the preoperative I.v. placebo than those subjects who received prophylactic I.v. penicillin (p-value of 0.03) which was statistically significant [8]. Similar findings by Monaco G et al., suggested that 2 gm amoxicillin prescribed PO 1 hour before the procedure showed a statistically significant reduction of SSI when compared to patients who were prescribed no antibiotics [20]. Sane VD et al., in his clinical study showed that only 1 patient (2%) developed postoperative SSI when single dose antibiotic was given preoperatively and concluded that antibiotics when administered 1 hour preoperatively is beneficial in reducing SSI [14]. In the present study, we had no case of SSI in both groups. López-Cedrún JL et al., compared the occurrence of SSI among patients who underwent SIM3M under preoperative antibiotic therapy, postoperative antibiotic therapy and placebo and found five patients in placebo group developed SSI (p-value=0.01) [40]. However, these differences were statistically insignificant. Reiland MD et al., found that 2.6% subjects developed SSI when subjected to postoperative PO antibiotic therapy and 3.3% in patients who received perioperative I.v. antibiotics (p-value=0.26) [54]. They concluded that there was no significant association between antibiotic regimen employed and SSI, and when antibiotics are considered perioperative I.v. antibiotics are preferred over postoperative PO antibiotics. Ren YF and Malmstrom HS in their meta-analysis of published trials found that SSI occurred with a frequency of 4% when systemic antibiotics were administered and 6.1% in placebo group after SIM3M and concluded that systemic antibiotics are effective in reducing the incidence of SSI [7]. Mehrabi M et al., in their study found 10% of SSI in SIM3M, which is a clean and contaminated wound, 20-40% SSI for contaminated and dirty wounds. They recommended antibiotic prophylaxis for clean contaminated, contaminated and dirty wounds [55]. According to Olusanya AA et al., a single dose of prophylactic peroral antibiotic is sufficient for most cases of third molar surgery while additional days of antibiotics should be used when more than usual degree of trauma is inflicted in the process of removal [56].
Alveolar Osteitis (AO): Alveolar osteitis or dry socket is the most frequently reported complication following removal of impacted mandibular third molars involving 25% to 30% of the patients [56]. More than infectious sequelae AO is considered as an inflammatory response of bone to a traumatic stimuli and the aetiology is associated strongly with socket blood clot fibrinolysis and bacterial contamination [57].
Xue P et al., showed the occurrence of 4 cases (2%) of AO in patients who received single dose preoperative antibiotics with continued postoperative PO antibiotics and 6 cases (3%) in placebo group confirming that there is no statistically significant result in incidence of AO between the 2 groups [2]. According to Halpern LR and Dodson TB, they found that no patient developed AO when subjected the preoperative I.v. placebo when compared to patients receiving prophylactic I.v. penicillin [8]. Ramos E et al., in a systemic review stated that preventive use of antibiotics significantly reduce the risk of AO in patients undergoing SIM3M [52]. Kaczmarzyk T et al., in their study reported AO in 1 (3.23%) patient in the single-dose preoperative antibiotic group, 2 (7.14%) patients in the single dose preoperative with 5-day postoperative antibiotic group and 4 (14.81%) patients in the placebo group [12]. The differences were statistically insignificant (p-value=0.26), proving that there is no significant difference in occurrence of AO among patients in 3 groups. Royhoudhary A et al., in his study demonstrated a statistically significant difference in development of AO in patients treated with placebo compared to patients in the postoperative antibiotic group after SIM3M [28]. They observed 14.58% of AO in the placebo group when compared to antibiotic group with a p-value of 0.012. Reiland MD et al., in their study, found that 6.4% subjects developed SSI when subjected to postoperative PO antibiotic therapy and 5.5% in patients who received perioperative I.v. antibiotics (p-value=0.65) [54]. Incidence of AO was 0% in our study in both the groups. Comparison of outcomes of present study with similar studies are compared [Table/Fig-7] [24,26,54,56].
Comparison of similar studies [24,26,54,56].
| Author’s name and year | Place of study | No. of subjects | Intervention | Parameters assessed | Conclusion |
|---|
| Olojede OA et al., [24] 2014 | Nigeria | 62 | Group I (n=31) had administration of 1 gram of oral metronidazole and 1 gram of amoxicillin capsules 30 minutes preoperative and Group II (n=31) had 500 milligrams of amoxicillin capsule 8 hourly and 400 milligrams of metronidazole tablets administered postoperatively for 5 days. | Pain, facial swelling and mouth opening assessment were done postoperatively and on days 1st, 3rd and 7th. | Administration of preoperative or postoperative antibiotics showed no marked differences in the degree of postoperative sequaele that occur after impacted mandibular third molar extractions. |
| Olusanya AA et al., [56] 2011 | Nigeria | 79 | Patients in preoperative group were given oral bolus of 2 gm amoxycillin capsules and 1 gm metronidazole tablets one hour before extraction, while those in the postoperative group were given a five-day regimen oral 500 mg amoxycillin capsules thrice daily and 400 mg metronidazole tablets thrice daily. | The occurrence of postoperative pain, swelling, trismus, SSI and AO were compared between the groups. | Single bolus antibiotic prophylaxis should be adequate for most cases of third molar surgery as the degree of postoperative pain, swelling and trismus was similar in both groups. However, a five-day postoperative antibiotic regimen is advised in patient with risk factors for AO. |
| Reiland MD et al., [54] 2017 | Rochester,Minnesota | 1895 | Group A subjects were treated with postoperative PO antibiotics alone (5-day course of amoxicillin) and the subjects treated in group B were treated with perioperative i.v. antibiotics (amoxicillin). | Primary outcome variables assessed were alveolar osteitis and surgical sit infection. | The use of a postoperative PO antibiotic regimen versus perioperative i.v. antibiotic regimen does not significantly alter the incidence of AO or SSI following elective third molar removal. if the surgeon chooses to use antibiotics in the setting of third molar surgery, perioperative i.v. antibiotics are preferable over postoperative PO antibiotics. |
| Sane VD et al., [26] 2014 | Maharashtra, India | 50 | In the first group postoperative antibiotic treatment was administered with Tab Augmentin 625 mg. The second group received no antibiotic medication and served as the control group. | Evaluation for pyrexia, purulent discharge from surgical site, persistent pain and/or swelling and lymphadenopathy was done on 1st, 3rd, 7th and 10th postoperative day. | No case of infection was seen in either of the two groups and suggests that antibiotics should be used reasonably and only if the surgeon feels the need to do so. From the results obtained in this study, the authors do not recommend the routine and indiscriminate use of antibiotics for surgical removal of asymptomatic impacted mandibular third molar. |
| Present study2021 | Mysore,India | 30 | Each subject acted as his/her own control in which the impacted tooth on one side was treated with conventional postsurgical PO antibiotics (cap. amoxicillin 500 mg thrice daily for 5 days) representing Group-A and the impacted 3rd molar on the other side was removed after 2 weeks with a single-dose preoperative i.v. antibiotic (Inj. amoxicillin 1 gm) 1 hour before the procedure (Group-B). | Primary outcome variables assessed were alveolar osteitis and surgical site infection. | Inj. amoxicillin 1 gm administered 1 hour preoperatively and cap. amoxicillin 500 mg administered postsurgically for 5 days had no statistically significant difference, hence suggesting that 1 gm Inj. amoxicillin administered 1 hour prior to surgery is a beneficial and cost effective alternative in lower third molar surgery. |
Limitation(s)
The control group was not included in this study owing to poor patient compliance.
Conclusion(s)
In the present study, alveolar osteitis and surgical site infection was not evident in both groups. Inj. amoxicillin 1 gm administered 1 hour preoperatively and cap. amoxicillin 500 mg administered postsurgically for 5 days following SIM3M had no statistically significant difference, hence suggesting that 1gm Inj. amoxicillin administered 1 hour prior to surgery is beneficial. Other factors like asepsis and sterilisation, atraumatic surgery, patient compliance with postoperative instructions will also play a major role in the development of postsurgical complications. Future research in newer antibiotic development along with antibiotic stewardship programs will help in overcoming development of antibiotic resistance.
Group A- Postoperative group, Group B- Preoperative group
Group A- Postoperative group, Group B- Preoperative group