Preorthodontic Management of Gingival Recession using Epithelial Embossed Connective Tissue Graft: A Case Report with Two years Follow-up
PG Resmi1, R Ambili2, M Neethu Prasad3, Leander Deepu4
1 Postgraduate Student, Department of Periodontics, PMS College of Dental Science and Research, Trivandrum, Kerala, India.
2 Professor, Department of Periodontics, PMS College of Dental Science and Research, Trivandrum, Kerala, India.
3 Postgraduate Student, Department of Orthodontics, PMS College of Dental Science and Research, Trivandrum, Kerala, India.
4 Professor, Department of Orthodontics, PMS College of Dental Science and Research, Trivandrum, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. R Ambili, Devikripa, KRA A 143A, Thumbikkonam Lane, Kudappanakunnu, P.O, Trivandrum 43, Kerala, India.
E-mail: ambilirenjith2020@gmail.com
Gingival recession is an aesthetic and functional problem requiring surgical management in most cases. Adequate gingival health is a prerequisite to maintain plaque control during orthodontic treatment. This case report described management of gingival recession before orthodontic treatment using a novel surgical method. Here, authors presented a case of 27-year-old female patient reported to the Department of Periodontics for management of gingival recession in the lower front tooth region. The patient was diagnosed with Miller’s Class II gingival recession on mandibular right central incisor. Vestibular depth and width of attached gingiva was found to be inadequate at the recession site. The case was managed with epithelial embossed connective graft. The recipient site was prepared using envelope technique and internal vestibular deepening was performed before placing the graft. Complete root coverage, adequate vestibular depth and width of attached gingiva were obtained postoperatively. Due to high aesthetic demand of the patient, orthodontic therapy was instituted six months following root coverage and patient could maintain good oral hygiene during orthodontic treatment. Results of surgical treatment were maintained till two years follow-up. Careful selection of surgical technique could enhance thickness and width of attached gingiva and retain vestibular depth at the recipient site. Successful case management enabled the patient to maintain gingival health during orthodontic treatment.
Attached gingiva, Complete root coverage, Plastic surgery, Vestibuloplasty
Case Report
A 27-year-old female patient reported to Department of Periodontics with the chief complaint of receding gums in the lower front tooth region. Probing depth, clinical attachment loss, recession height, recession width and keratinised tissue thickness were measured using Williams periodontal probe. Full mouth bleeding score [1] and full mouth plaque score [2] was calculated. Non surgical periodontal therapy was performed, and patient was re-evaluated after four weeks. Miller’s Class II gingival recession was noticed in relation to mandibular right central incisor [Table/Fig-1a,b]. Patient’s oral hygiene was satisfactory with a Full Mouth Plaque Score (FMPS) score of 8%, Full Mouth Bleeding Score (FMBS) score of 10%. Patient did not have any clinical signs of active periodontal disease or occlusal abnormality. The frenal attachment was mucosal. Tension test was positive which showed an inadequate width of attached gingiva (1 mm). Vestibular depth was measured using manual method and it was again inadequate (2 mm). The patient’s medical history was non contributory with no contraindication for surgery.
Authors performed epithelium embossed connective tissue graft as proposed by Sterrett JD with modification [3]. The procedure was clearly explained, and surgery was carried out after obtaining informed consent from the patient. Local anaesthesia (2% lignocaine with 1:80,000 adrenaline) was administered. A modification was made to the original technique [1]. After giving initial sulcular incisions, a subperiosteal tunnel was made using a tunnelling instrument, maintaining the interdental papilla, and periosteal scoring was carried out internally through the pouch prepared [4]. Tinfoil template was made as per the pouch dimension (10×7 mm) and transferred to the palate from where the donor tissue was obtained.
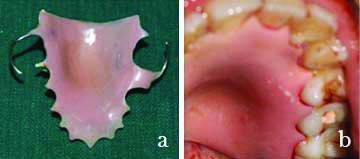
Connective tissue graft was harvested with a portion of epithelium embossed in it corresponding to recession dimension from palatal aspect of upper left premolars by a technique described by Sterrett JD in 2009 [3]. The graft tissue had connective tissue on all the sides, and its centre region was embossed with epithelium which matched the defect morphology [Table/Fig-2a,b]. Donor site was sutured with 5-0 prolene suture and covered with prefabricated acrylic stent [Table/Fig-3a,b]. The donor tissue was positioned over the recipient site in such a way that the connective tissue portion of the graft was secured inside the pouch created and the embossed epithelium was positioned directly over the recession site [Table/Fig-4a,b]. The graft was secured in place using non resorbable 5.0 sutures (Ethicon, prolene Suture) using atraumatic independent stabilising sutures and a periodontal dressing (Coe-PakTM) was placed. The patient was prescribed analgesic (tab. paracetamol 500 mg, three times daily for two days) and was instructed to avoid brushing the surgical area and clean the teeth using a cotton dipped in chlorhexidine mouthwash. In addition, she was asked to rinse with 1:1 diluted 0.2% chlorhexidine for one minute twice daily for 10 days. The periodontal dressing and sutures were removed one week later, and oral hygiene instructions were reinforced. Healing was uneventful and the appearance of recipient and donor site immediately after suture removal is shown in [Table/Fig-5a,b]. The patient was re-evaluated after three months, and thereafter every six months for two years. Appreciable root coverage, adequate vestibular depth, thickness as well as width of attached gingiva were noticed from three months onwards [Table/Fig-6a,b].
Preoperative measurements taken using Williams periodontal probe: a) Depth of recession; b) width of recession.

Donor site preparation: (a) Outline; (b) Tissue obtained (Dimension 10×7 mm).

a) Acrylic stent; b) stent in position.
Recipient site preparation: a) Tunnel preparation; b) Graft placed in position and sutured

Postoperative view after suture removal: a) recipient site; b) donor site.

Postoperative view: a) after 12 months; b) after 24 months.
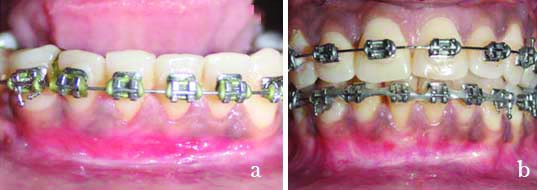
Orthodontic therapy was started six months after the root-coverage procedure. Patient was diagnosed to have Angle’s Class I malocclusion on a Skeletal Class I base with mild spacing in upper and lower arch with moderately proclined lower incisors. Non extraction fixed orthodontic therapy was planned. After initial alignment and levelling the remaining space closure was done followed by finishing and detailing. During orthodontic treatment patient could maintain good oral hygiene as evident by low plaque and bleeding score. Postoperative results were maintained until last re-evaluation [Table/Fig-7]. Root Coverage Esthetic Score (RES) was calculated after two year follow-up and is given in [Table/Fig-8] [5].
Clinical parameters at baseline, 3 months, 6 months, 12 months and 24 months interval at 41 region.
| Clinical parameters (mm) | Baseline | After 3 months | After 6 months | After 12 months | After 24 months |
|---|
| PD | 2 | 1 | 1 | 1 | 1 |
| CAL | 6 | 2 | 2 | 1.5 | 1.5 |
| RH | 4 | 0 | 0 | 0.5 | 0.5 |
| RW | 2 | 0 | 0 | 0.5 | 0.5 |
| KT Thickness | 1 | 3 | 2 | 2 | 2 |
| FMBS | 10% | 12% | 15% | 12% | 8% |
| FMPS | 8% | 11% | 12% | 12% | 10% |
PD: Probing depth; CAL: Clinical attachment loss; RH: Recession height; RW: Recession width; KT: Keratinised tissue; FMPS: Full mouth plaque score; FMBS: Full mouth bleeding score
Root aesthetic score at 24 months postoperatively.
| RES Parameters* | RES score |
|---|
| Gingival Margin (GM) | 6 |
| Marginal Tissue Contour (MTC) | 1 |
| Soft Tissue Texture (STT) | 1 |
| Gingival Colour (GC) | 1 |
| Mucogingival Junction (MGJ) | 1 |
*Scoring criteria-GM: 0- No coverage; 3: Partial coverage; 6: Complete root coverage, MTC: 0- Irregular margin does not follow; CEJ: 1- Proper contour; STT: 0- Scar/keloid formation; 1- Absence of scar; GC: 0- Colour of tissue varies; 1- Colour similar, MGJ: 0- MGJ not aligned with MGJ of adjacent teeth; 1- MGJ aligned
Discussion
Denuded root surfaces cause aesthetic concerns and predispose to caries and hypersensitivity. They are often accompanied with inadequate attached gingiva and vestibular depth which make plaque control difficult. Orthodontic treatment can worsen the oral hygiene maintenance in such situations. Many surgical techniques are described for root coverage and to increase the width of attached gingiva [6-8]. Subepithelial connective tissue graft with coronally advanced flap is considered as the gold standard technique for root coverage [9]. But coronal advancement requires adequate amount of attached gingiva as well as sufficient vestibular depth [10]. When there is deficiency of attached gingiva and vestibular depth, free gingival graft is the technique of choice. But it creates an open wound at the donor site increasing postoperative discomfort and unaesthetic appearance at the recipient site due to colour mismatch [11]. Innovative surgical techniques must be designed as an alternative solution. The present case report describes successful management of gingival recession in a patient before orthodontic treatment using a combination of free gingival and connective tissue graft which is superior to the existing techniques in sites with inadequate attached gingiva and vestibular depth.
Epithelial embossed connective tissue graft possesses advantages of both subepithelial connective tissue graft and free gingival graft. Major portion of the graft was placed into the pouch over the periosteum which provided dual blood supply. Subepithelial connective tissue graft around the area of recession helped to increase the thickness and width of attached gingiva. The embossed epithelium protected the underlying connective tissue and promoted healing by primary intention [4]. Moreover, previous studies have demonstrated an increase in width of attached gingiva where connective tissue graft was not accompanied by coronally advanced flap [9,12]. Since a very small portion of the donor tissue was devoid of epithelium, healing at donor site was uneventful. Colour match was also optimal compared to free gingival graft.
There were few case reports of epithelial embossed connective tissue graft in the literature [3,13-15]. The technique was originally described by Sterrett JD for maxillary canine recession with short term follow-up without providing data on amount of root coverage or attachment gain [3]. Even though the article describes another case of mandibular premolar recession, its postoperative results are not provided. Rath A et al., described root coverage of labial recession of maxillary canine and palatal recession of maxillary molar which were followed-up for 1 year [13,14]. Complete root coverage was obtained for maxillary canine whereas 93.6% root coverage and 7.5 mm gain in attachment level was reported for palatal recession. Ramakrishnan T et al., described management of maxillary canine recession and obtained complete root coverage after six months follow-up [15].
Conclusion(s)
To the best of authors knowledge, this was the first case report of epithelial embossed connective tissue graft for management of lower anterior recession which is a frequent site of gingival recession. The successful management of the case enabled the patient to maintain good oral hygiene during orthodontic treatment. Customised case management is extremely essential for the best possible outcome. Histological evaluation of the regenerated area has to be carried out in future studies. Comparative studies with partially de-epithelialised connective tissue also can be carried out especially in terms of donor site morbidity.
PD: Probing depth; CAL: Clinical attachment loss; RH: Recession height; RW: Recession width; KT: Keratinised tissue; FMPS: Full mouth plaque score; FMBS: Full mouth bleeding score
*Scoring criteria-GM: 0- No coverage; 3: Partial coverage; 6: Complete root coverage, MTC: 0- Irregular margin does not follow; CEJ: 1- Proper contour; STT: 0- Scar/keloid formation; 1- Absence of scar; GC: 0- Colour of tissue varies; 1- Colour similar, MGJ: 0- MGJ not aligned with MGJ of adjacent teeth; 1- MGJ aligned
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 28, 2021
Manual Googling: Sep 02, 2021
iThenticate Software: Sep 20, 2021 (14%)
[1]. Muhlemann HR, Gingival sulcus bleeding-a leading symptom in initial gingivitisHelv Odontol Acta 1971 15:107-13. [Google Scholar]
[2]. O’Leary TJ, Drake RB, Naylor JE, The plaque control recordJ Periodontol 1972 43(1):3810.1902/jop.1972.43.1.384500182 [Google Scholar] [CrossRef] [PubMed]
[3]. Sterrett JD, The management of large mucogingival defects with an “epithelial embossed” connective tissue graftInt J Periodontics Restorative Dent 2008 28(6):577-83. [Google Scholar]
[4]. Raetzke PB, Covering localized areas of root exposure employing the “envelope” techniqueJ Periodontol 1985 56(7):397-402.10.1902/jop.1985.56.7.3973894614 [Google Scholar] [CrossRef] [PubMed]
[5]. Cairo F, Nieri M, Cattabriga M, Cortellini P, De Paoli S, De Sanctis M, Root coverage aesthetic score after treatment of gingival recession: An interrater agreement multicenter studyJ Periodontol 2010 81(12):1752-58.10.1902/jop.2010.10027820629546 [Google Scholar] [CrossRef] [PubMed]
[6]. Sullivan HC, Free autogenous gingival graftsIII. Utilization of grafts in the treatment of gingival recession. Periodontics 1968 6:152-60. [Google Scholar]
[7]. Grupe HE, Warren Jr RF, Repair of gingival defects by a sliding flap operationJ Periodontol 1956 27(2):92-95.10.1902/jop.1956.27.2.92 [Google Scholar] [CrossRef]
[8]. Bouchard P, Etienne D, Ouhayoun JP, Nilvéus R, Subepithelial connective tissue grafts in the treatment of gingival recessions. A comparative study of 2 proceduresJ Periodontol 1994 65(10):929-36.10.1902/jop.1994.65.10.9297823274 [Google Scholar] [CrossRef] [PubMed]
[9]. Dhanpal PC, Yiu CK, King NM, Tay FR, Hiraishi N, Effect of temperature on water sorption and solubility of dental adhesive resinsJ Dent 2009 37(2):122-32.10.1016/j.jdent.2008.10.00419062151 [Google Scholar] [CrossRef] [PubMed]
[10]. Lang NP, Löe H, The relationship between the width of Keratinised gingiva and gingival healthJ periodontol 1972 43(10):623-27.10.1902/jop.1972.43.10.6234507712 [Google Scholar] [CrossRef] [PubMed]
[11]. Wyrębek B, Górski B, Górska R, Patient morbidity at the palatal donor site depending on gingival graft dimensionDent Med Probl 2018 55(2):153-59.10.17219/dmp/9140630152618 [Google Scholar] [CrossRef] [PubMed]
[12]. Cordioli G, Mortarino C, Chierico A, Grusovin MG, Majzoub Z, Comparison of 2 techniques of subepithelial connective tissue graft in the treatment of gingival recessionsJ Periodontol 2001 72(11):1470-76.10.1902/jop.2001.72.11.147011759857 [Google Scholar] [CrossRef] [PubMed]
[13]. Rath A, Fernandes B, Priyadarshini HR, Varma S, Pavuluri AK, Root coverage of palatal recession using epithelial embossed connective tissue: A case reportJ Int Acad Periodontol 2017 19(1):10-14. [Google Scholar]
[14]. Rath A, Fernandes BA, Sidhu P, Ramamurthy P, Root coverage of a wide anterior mucogingival defect with epithelial embossed connective tissue graft and its evaluation using root coverage esthetic scoresJ Indian Soc Periodontol 2017 21(3):24510.4103/jisp.jisp_221_1729440795 [Google Scholar] [CrossRef] [PubMed]
[15]. Ramakrishnan T, Kaur M, Aggarwal K, Root coverage using epithelial embossed connective tissue graftIndian J Dent Res 2011 22(5):72610.4103/0970-9290.9346622406723 [Google Scholar] [CrossRef] [PubMed]