Recurrent Cutaneous Adenoid Cystic Carcinoma of Forehead
Ashi Vijayaraghavan1, Subhashini Ramamoorthy2, Sylvia Mary Theresa3, Banushree C Srinivasamurthy4, Sankappa P Sinhasan5
1 Postgraduate Student, Department of Pathology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
2 Senior Resident, Department of Pathology, JIPMER, Puducherry, India.
3 Assistant Professor, Department of Pathology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
4 Associate Professor, Department of Pathology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
5 Associate Professor and Head, Department of Pathology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sankappa P Sinhasan, Associate Professor and Head, Department of Pathology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
E-mail: drspsinhasan@gmail.com
Adenoid Cystic Carcinoma (ACC) is a malignant tumour more commonly seen in salivary glands and rarely arises from the skin as adnexal tumour. Cutaneous ACC is a rare malignant adnexal tumour of eccrine origin. It has an indolent course and rarely metastasizes. Hereby, authors report a case of 48-year-old male with complaints of swelling on right forehead present for the past four years. Clinical diagnosis of infected sebaceous cyst was made and excised with simple excision. The swelling reappeared within 15 days of first surgery. The cytological examination of the swelling revealed abundant cellularity with predominantly cohesive clusters of monomorphic population of cells centered around eosinophilic hyaline globules suggestive of ACC. Retrieval of previous biopsy report revealed diagnosis of ACC reaching the margins of excision, the report of which was neither collected by either operating surgeon nor by the patient. Histopathological examination revealed classical cribriform pattern of arrangement of tumour cells with perineural infiltration by tumour cells. Immunohistochemistry further confirmed the diagnosis. The present case report brings out the importance of clearance of surgical margins in malignant tumours, including skin adnexal tumours. It also highlights the importance of histopathological examination of benign looking skin adnexal tumours.
Adnexal tumour, Eosinophilic hyaline globules, Swelling
Case Report
A 48-year-old male presented with history of swelling on right side of forehead since past four years. The swelling was associated with pain. Patient gave history of surgery done for a similar type of swelling at the same site a month back. The swelling had recurred within a month after the surgery. He had not collected the histopathology report and he did not under went any follow-up after the previous surgery. He was referred for Fine Needle Aspiration Cytology (FNAC) from the Surgical Outpatient Department.
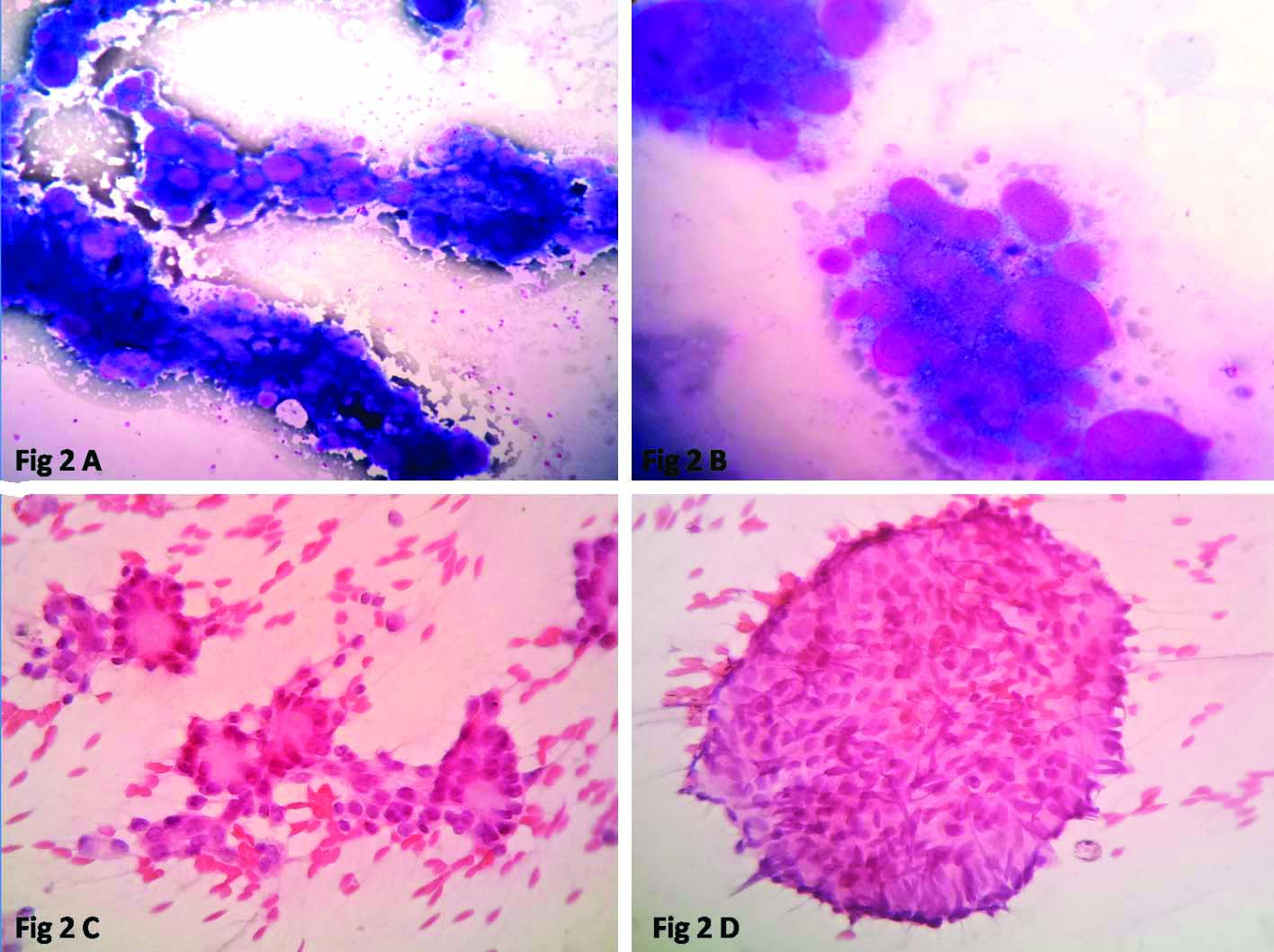
On clinical examination a firm tender nodule was located on the right forehead laterally measuring 3×2 cm [Table/Fig-1]. The overlying skin had a healed scar measuring 1 cm size. The FNAC of the swelling was done and it yielded blood mixed aspirate. Cytology smears showed abundant cellularity with predominantly cohesive clusters of cells [Table/Fig-2a]. The cells were centered around eosinophilic hyaline globules [Table/Fig-2b]. The cells were round with monomorphic population, minimal cytoplasm and tiny nucleoli, arranged in tiny acinar pattern [Table/Fig-2c]. The background showed scattered single cells and large sheets with similar morphology [Table/Fig-2d]. The differential diagnosis considered were Adenoid Cystic Carcinoma (ACC) and adenoid variant of Basal Cell Carcinoma (BCC). The cytological provisional diagnosis was offered as ACC of the skin with advice to do biopsy for further confirmation.
A firm tender nodule was present in the right forehead measuring 3×2 cm.

Cytology smears showing cohesive clusters of cells: a) (Giemsa stain, 4X). Presence of numerous eosinophilic hyaline globules; b) (Giemsa stain, 10X). The tumour cells were round with monomorphic population arranged in tiny acinar pattern; c) (H&E stain, 40X) and in large sheets; d) (H&E stain, 40X).
Meanwhile, with his history of previous surgery, the histopathology biopsy slides and reports were retrived from archives, that revealed swelling on the right forehead of one month duration, 0.5×0.5 cm which was firm and tender, with clinical diagnosis of sebaceous cyst for which simple excision was done. The biopsy report was issued as adenoid cystic carcinoma of skin and advised re-excision of the tumour due to presence of tumour cells at the margin. But unfortunately, postoperatively, neither patient came for the follow-up nor the biopsy report was collected by the surgical team.
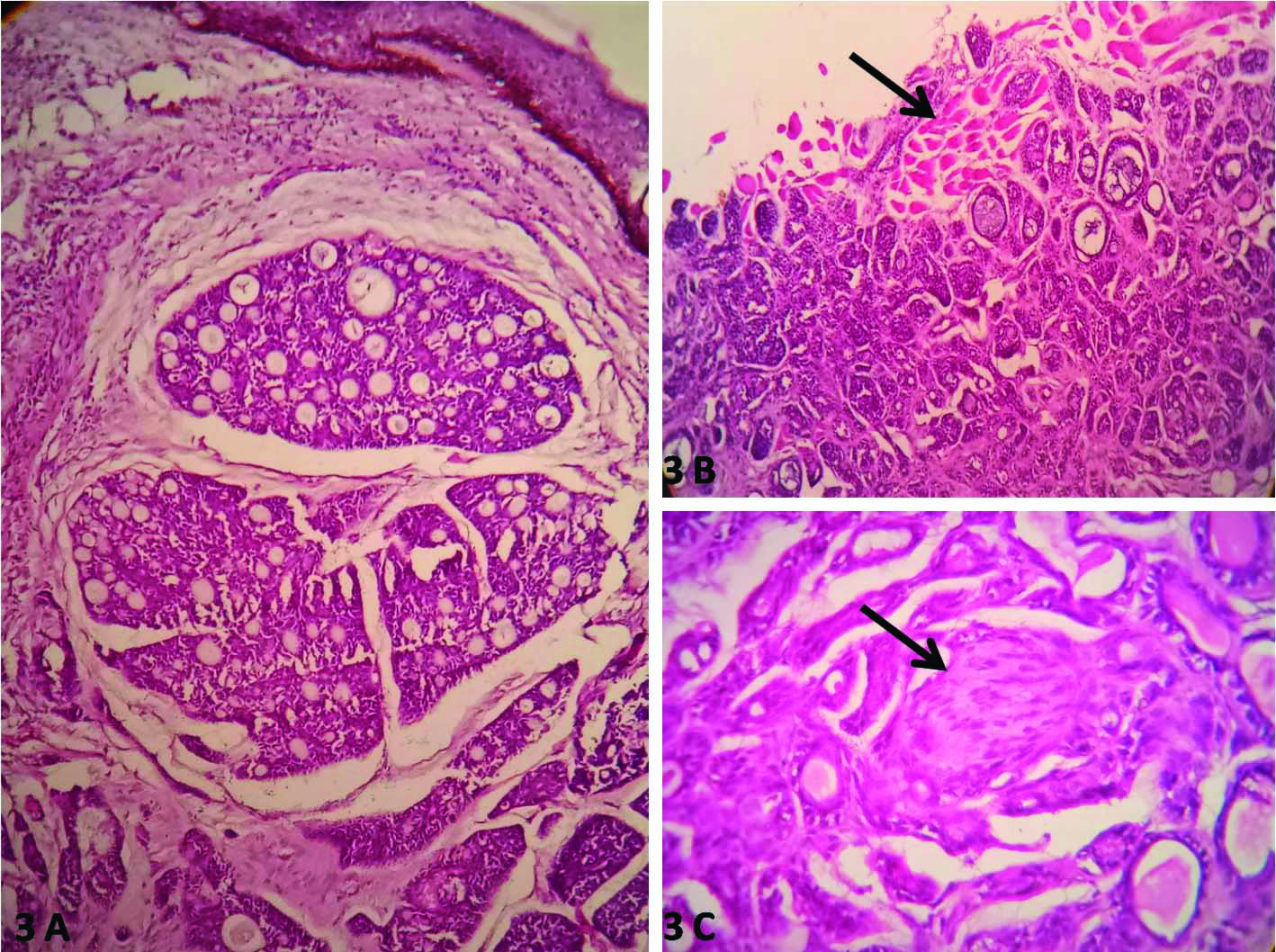
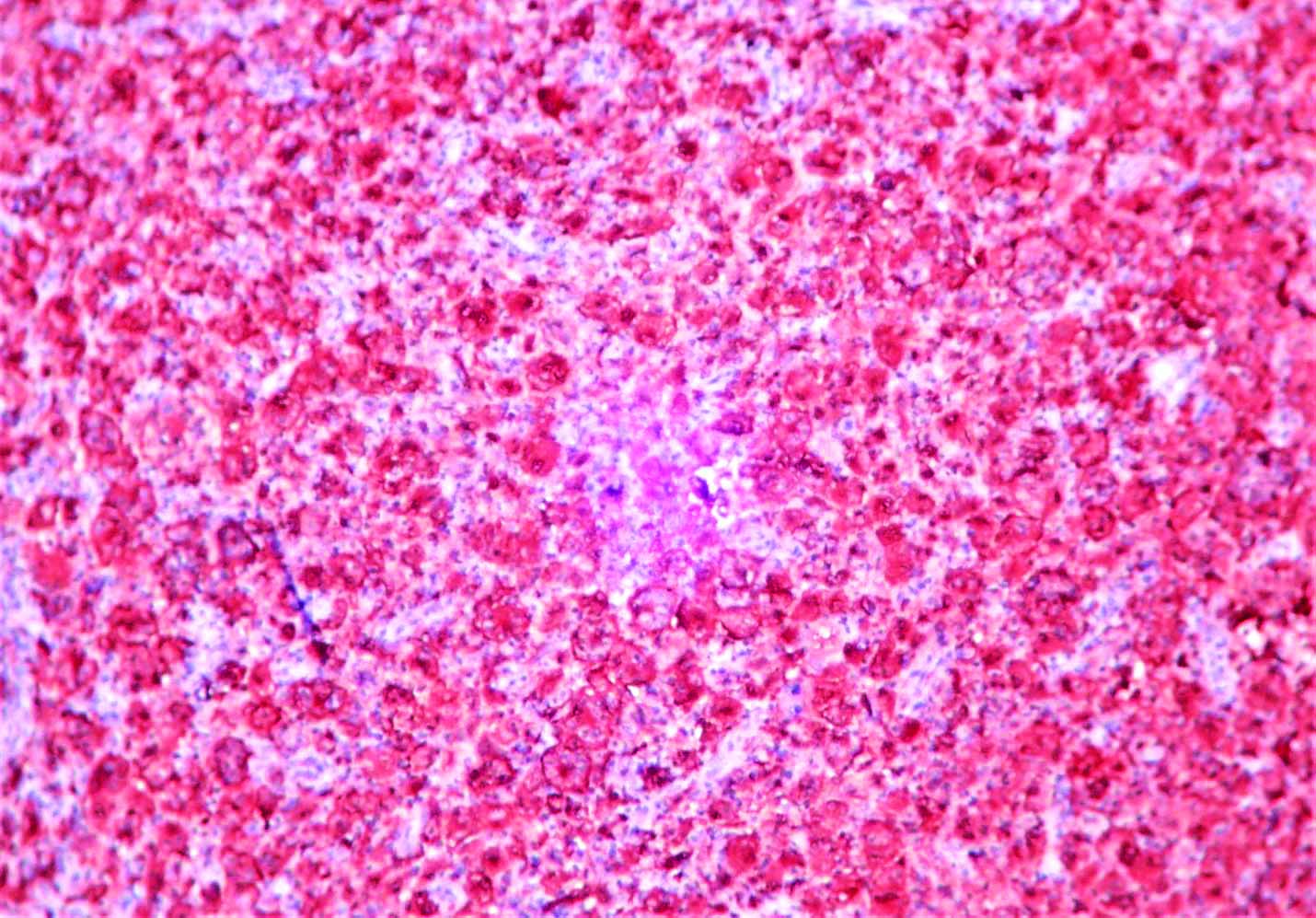
At the present visit, after seeing cytology report, the tumour was excised with wide local excision with rhomboid flap closure. Gross examination of excised specimen showed skin covered soft tissue swelling measuring 2.5×2×1 cm. External surface of skin showed an elevated nodule measuring 1×1 cm and on cut section it was grey white, soft with a tiny ulcer at one end. On histopathological examination, the epidermis was thinned out with an infiltrative lesion in the dermis [Table/Fig-3a]. These tumour cells were seen extending vertically, infiltrating the nerve bundles, subcutaneous fat and horizontally extending upto the lateral margins of resection and infiltrated the skeletal muscle fibers [Table/Fig-3b]. The tumour had basaloid clusters of cells arranged in lace-like pattern, cribriform and glandular pattern. Basophilic mucinous and eosinophilic material was present within the cystic spaces. There was evidence of perineural infiltration [Table/Fig-3c]. Mitosis was two/high power field. Differential diagnosis of cutaneous ACC and adenoid variant of BCC were considered. The BCC was considered as differential diagnosis due to presence of basaloid population of cell clusters and it can exhibit a varied morphology such as adenoid, keratotic, sebaceous, basosquamous, apocrine, eccrine or fibroepithelial. Tumours with a similar histopathological picture are cutaneous ACC and primary cutaneous cribriform apocrine carcinoma. As there was no evidence of peripheral palisading and retraction artefacts and as there was no connection with epidermis diagnosis of adenoid variant of BCC was ruled out. As there was presence of perineural invasion with classical cribriform pattern of arrangement of tumour cells, diagnosis of recurrent primary cutaneous adenoid cystic carcinoma was issued. Immunohistochemistry stain S-100 was carried out and the tumour cells were diffusely positive [Table/Fig-4] for it thereby confirming the diagnosis of cutaneous ACC.
Histopathology showing thinned out epidermis with an infiltrative lesion in the dermis; a) (H&E stain, 4X). The tumour had basaloid clusters of cells arranged in cribriform and glandular pattern with perineural infiltration; b) (H&E stain, 4X); c) (H&E stain, 40X) and infiltrating surrounding skeletal muscle fibers.
Immunohistochemistry (IHC) stain showing diffuse positivity for tumour cells (S-100 stain, 4X).
In view of presence of tumour cells in one of the surgical margin, patient was referred to tertiary cancer Institute for further treatment.
Discussion
The ACC is a malignant tumour common in the salivary glands. Other rare sites of occurrence are the breast, lungs, skin and cervix. The ACC arising from the skin was first reported in 1975 by Boggio R [1]. It is an adnexal tumour probably of eccrine origin. The scalp has been reported as the most common site [2,3]. Though similar in morphology to salivary gland tumours cutaneous ACC has a different behaviour and prognosis proving it to be different at molecular level. From a retrospective study of adenoid cystic carcinoma, Sharma P et al., reported only one case of cutaneous ACC of the 30 cases of ACC which shows its uncommon incidence [4]. The average age of cases reported is 55-59 years and female predominance [4]. The patient in the present case was a male with similar age group incidence. Common sites of occurrence are the scalp (32-41%), followed by chest and abdomen [5]. Clinically, it presents as a tender nodule due to the perineural invasion as happened in the present case. Metastasis of ACC is rare [2,6]. Cutaneous ACC usually has an indolent course in contrast to ACC of the salivary gland which has an aggressive course [2,6]. Similarly the patient had a slow progressive course with four years history of swelling, but swelling had recurred within one month of surgery due to incomplete excision. However, cutaneous ACC can cause multiple recurrences as seen in the present patient due to widespread infiltration into the fat or muscle and around nerves. Previous studies have noted recurrence in 44% of cases following wide local excision [7-9]. Mohs micrographic surgery has been reported the best method to prevent local recurrences by Xu YG et al., [7]. In the present case the surgical margins were involved by tumour and perineural invasion was also seen and these factors have led to immediate recurrence of the tumour within a month period of time. However, there was no evidence of distant metastasis. Few authors have used intraoperative frozen sections to get tumour free margins [7-9].
Histologically, the main differential diagnosis to be considered is the adenoid variant of BCC. Xu YG et al., reported a similar case in a female with chest nodule mistaken for BCC and presented later with recurrent nodule in the scar site [7]. Absence of epidermal connection and presence of perineural invasion favours diagnosis of ACC. Adenoid variant of BCC also can show gland formations, cribriform pattern and cystic spaces with mucinous material mimicking ACC.
Immunohistochemistry helps in differentiating ACC from adenoid BCC, as EMA, CEA, and S100 to be positive in ACC but not in adenoid BCC [2,4,10]. In the present case was tumour cells were positive for S-100, thereby confirming the diagnosis. Other tumours to be differentiated includes mucinous carcinoma of skin, cutaneous cribriform apocrine carcinoma [2,4,10].
At molecular level, MYB-NFIB gene fusion has been reported in ACC of salivary glands but Prieto-Granada CN et al., reported MYB aberrations in three cases of cutaneous ACC using fluorescent probes and none of the cases showed NFIB rearrangement [11]. This might suggest though morphologically similar the genetic variations account for the difference in the clinical behaviour.
The gold standard treatment for adenoid cystic carcinoma is often consisting of wide surgical excision with at least 2 cm tumour free margins to exclude local recurrences caused by perineural extensions. Cutaneous ACC has low potential for distant metastasis while locally being infiltrative with frequent perineural invasion [12]. The role of Mohs surgery in preventing local recurrence and role of postoperative radiation therapy has not been well established in cutaneous ACC due to the rarity of the tumour and the small number of available case reports [13].
Conclusion(s)
Author reported this case due to its rare incidence, morphological overlapping features with adenoid BCC, and highlight the importance of histopathological examination of benign looking skin adnexal tumours. Newer surgical methods are required to prevent recurrences. The ACC though morphologically look alike may be molecularly different at different sites which definitely need further studies. Prognosis and outcome of cutaneous ACC and adenoid BCC greatly differ hence correct histological diagnosis is very vital in the management of these cases.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 28, 2021
Manual Googling: Aug 27, 2021
iThenticate Software: Sep 18, 2021 (9%)
[1]. Boggio R, Adenoid cystic carcinoma of scalpArch Dermatol 1975 111:793-94. [Google Scholar]
[2]. Raychaudhuri S, Santosh KV, Satish Babu HV, Primary cutaneous adenoid cystic carcinoma of the chest wall: A rare entityJ Can Res Ther 2012 8:633-35.10.4103/0973-1482.10658323361287 [Google Scholar] [CrossRef] [PubMed]
[3]. Khan AJ, Digiovanna MP, Ross DA, Adenoid cystic carcinoma: A retrospective clinical reviewInt J of Cancer 2001 96:149-58.10.1002/ijc.101311410883 [Google Scholar] [CrossRef] [PubMed]
[4]. Sharma P, Jha V, Mandal AK, Clinicopathological correlation of adenoid cystic carcinoma: A notorious masquerade and clinical paradoxIndian J Med Paediatr Oncol 2018 39:276-81.10.4103/ijmpo.ijmpo_141_16 [Google Scholar] [CrossRef]
[5]. Naylor E, Sarkar P, Perlis CS, Giri D, Gnepp DR, Bostom LR, Primary cutaneous adenoid cystic carcinomaJ Am Acad Dermatol 2008 58(4):636-41.10.1016/j.jaad.2007.12.00518342709 [Google Scholar] [CrossRef] [PubMed]
[6]. Cacchi C, Persechino S, Fidanza L, Bartolazzi S, A primary cutaneous adenoid cystic carcinoma in a young woman. Differential diagnosis and clinical implicationsRare Tumours 2011 3:03-09.10.4081/rt.2011.e321464876 [Google Scholar] [CrossRef] [PubMed]
[7]. Xu YG, Hinshaw M, Longley BJ, Ilyas H, Snow SN, Cutaneous adenoid cystic carcinoma with perineural invasion treated by Mohs micrographic surgery– A case report with literature reviewJ Oncol 2010 10:01-06.10.1155/2010/46904920379385 [Google Scholar] [CrossRef] [PubMed]
[8]. Aleksandar LK, Recurrent adenoid cystic carcinoma of the scalp treated with Mohs micrographic surgeryDermatol Surg 2003 29:647-49.10.1046/j.1524-4725.2003.29155.x12786711 [Google Scholar] [CrossRef] [PubMed]
[9]. Fueston JC, Gloster HM, Diya FM, Primary cutaneous adenoid cystic carcinoma: A case report and literature reviewCutis 2006 77:157-60. [Google Scholar]
[10]. Alkan BI, Bozdogan O, Karadeniz M, BozdoLan N, Two different cell populations is an important clue for diagnosis of primary cutaneous adenoid cystic carcinoma: Immunohistochemical studyCase Rep in Path 2017 10:01-06.10.1155/2017/794936128243477 [Google Scholar] [CrossRef] [PubMed]
[11]. Prieto-Granada CN, Zhang L, Antonescu C, Henneberry J, Messina J, Primary Cutaneous Adenoid Cystic Carcinoma with MYB aberrations, report of three cases and comprehensive review of the literatureJ Cutan Pathol 2017 44(2):201-09.10.1111/cup.1285627859477 [Google Scholar] [CrossRef] [PubMed]
[12]. Ferreira S, Fernandes IC, Coelho A, Selores M, Primary Cutaneous Adenoid Cystic Carcinoma of the abdomen: A rare entityDermatol Online J 2020 26(8):16-19.10.5070/D3268049896 [Google Scholar] [CrossRef]
[13]. Iro S, Raiteb M, Maadane A, Elmrini S, Slimani F, Cutaneous adenoid cystic carcinoma of lower eyelid: Case report of a rare malignant entityAnn Med Surg 2021 67:10246710.1016/j.amsu.2021.10246734168870 [Google Scholar] [CrossRef] [PubMed]