Clinical and Cardiorespiratory Polygraphy Profile in Children with Obstructive Sleep Apnoea Syndrome: A Cross-sectional Study
Jeyakumar Settu1, Stalin Selvaraj2, Seenivasan Venkatasamy3
1 Assistant Surgeon, Department of Paediatrics, Government Periyar Hospital, Mayiladuthurai, Tamil Nadu, India.
2 Associate Professor, Department of Paediatrics, Government Villupuram Medical College and Hospital, Villupuram, Tamil Nadu, India.
3 Associate Professor, Department of Paediatrics, Government Thiruvannamalai Medical College and Hospital, Thiruvannamalai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Seenivasan Venkatasamy, New No. 52/4, Old No. 11/4, 3rd Floor, Jai Shree Apartment 12th Avenue, Ashok Nagar, Chennai, Tamil Nadu, India.
E-mail: chellamnivas@gmail.com
Introduction
Cardiorespiratory Polygraphy (CRP) is a less costly and simplified alternative to time consuming and laborious over night polysomnography for diagnosis of Obstructive Sleep Apnoea Syndrome (OSAS) in children. The Apnoea Hypopnea Index (AHI) is simple and useful index that can be estimated by using CRP. The magnitude of AHI which reflects severity of OSAS is unknown in the paediatric population.
Aim
To describe the clinical characteristics and to estimate AHI in a population of children with obstructive sleep apnoea and hypopnea syndrome.
Materials and Methods
This cross-sectional observational study was conducted on 1500 children, below 12 years of age, from January 2018 to November 2018. They were screened using Paediatric Sleep Questionnaire (PSQ) in the Outpatient Departments of General Paediatrics and Pulmonology respectively, at the Institute of Child Health and Hospital for Children, Chennai, Tamil Nadu, India. Those children identified to have probable OSAS were made to undergo cardiorespiratory assessment. Children with craniofacial syndromes and congenital heart disease were excluded from the study. Anthropometric parameters, vital signs, and Body Mass Index (BMI) were recorded. AHI and oxyhaemoglobin desaturation index were estimated in CRP. After descriptive analysis, non parametric Mann-Whitney test was used to find out any significant difference in median values of AHI in clinical subgroups. Regression analysis was done between AHI values and BMI.
Results
Total 47 children were subjected to cardiorespiratory polygraphy. There was no statistically significant difference in gender distribution and prevalence of adenoid enlargement (p-value=0.1447 and 0.7705, respectively). It was found that maximum occurrence of OSAS was at the age of 6 years (25.5%). Based on AHI score 44.7% children fell in moderate to severe OSAS category. There was a poor correlation between BMI scores and AHI, though no significant difference was observed (r=-0.266, p-value=0.07087). The difference in median AHI between males and females was not statistically significant (p-value=0.5256), while that between children with/without adenoid enlargement was statistically significant (p-value ≤0.001).
Conclusion
Children with adenoid hypertrophy have higher AHI than children without adenoid hypertrophy. There is lack of evidence for male predominance in the study. Obesity poorly correlated with AHI score.
Adenoid hypertorphy, Apnea hypopnea index, Obesity
Introduction
The prevalence of Obstructive Sleep Apnoea Syndrome (OSAS) in paediatric age group is around 1-4% [1]. OSAS falls in the spectrum of obstructive Sleep Disordered Breathing (SDB). At the lower end of the spectrum lies primary or habitual snoring. Snoring is present in upto 27% of children. A 7 to 12% can be attributed to habitual snoring. The ratio between habitual snoring and OSAS is 4:1 to 6:1. OSAS seems to be more common during the preschool years when the tonsils and adenoids are the largest [2]. Other risk factors for OSAS are male gender, obesity, adenoid hypertrophy, cerebral palsy, neuromuscular disorders, craniofacial anomalies and genetic syndromes [3]. Disordered sleep in OSAS leads to behavioural disturbances, learning difficulties, excessive daytime sleepiness and long term cardiovascular morbidity [4-7].
Paediatric polysomnography is the gold standard in diagnosing OSAS. However, this procedure is complicated, time-consuming, expensive and is not readily available in most hospitals. It is widely accepted that Cardiorespiratory Polygraphy (CRP) is a less costly and simplified alternative to full-night polysomnography for diagnosis of OSAS in children [8,9]. Sleep apnoea is defined as complete loss breathing for 10 seconds or more while sleeping. In similar way, hypopnea is defined as partial loss of breath for 10 seconds or longer. The AHI is simple and useful index that can be estimated by using CRP. It tells the number of mixed, obstructive and central apnoeas and hypopnoeas per hour of total study time. Most sleep centers consider an Apnoea Hypopnea Index (AHI) of ≤1 to be normal, 1 < AHI ≤5 to be mild OSA, 5 < AHI ≤10 to be moderate OSA, and an AHI > 10 as severe OSA [10,11].
The prevalence of OSAS has two age peaks. The first peak with the presence of enlarged adenoid occurs in children from 2 to 8 years of age. A second peak happens at adolescence because of increase in weight [12]. Overweight or obese children have significantly higher prevalence of OSAS when compared to those children having normal weight [13]. In preadolescent children, there is lack of sex differences in occurrence of OSAS and severity of OSAS. There is higher prevalence in boys during adolescent period, as females have higher upper airway space and less severe OSAS [14].
By using the AHI, one can estimate the severity of the OSAS at baseline. One can follow-up the children by reassessing the AHI score. It will help to assess the effectiveness of adenotonsillectomy, Continuous Positive Airway Pressure (CPAP) therapy and weight reduction in bringing down OSAS symptoms. However, the magnitude of AHI, which reflects severity of OSAS, is little known in Southern Indian paediatric population.
The aim of the present study was to describe the clinical profile of children with OSAS and to determine the relationship of AHI to their Body Mass Index (BMI) and distribution of AHI among gender and adenoid status.
Materials and Methods
This cross-sectional observational study was conducted at Outpatient Department of Pulmonology and General Paediatrics at Institute of Child Health and Hospital for Children, Chennai, Tamil Nadu, India, from January 2018 to November 2018. The ethical approval was obtained from Institutional Ethical Committee approval (no:23012018).
Sample size calculation: Expecting 4% prevalence of OSAS in children with 1% margin of error at 95% confidence level, the required sample size was 1500 [15]. Hence, 1500 children under 12 years of age were screened for OSAS.
Paediatric Sleep Questionnaire (PSQ) was utilised to screen children with OSAS [16]. The PSQ scores 22 items that are divided into nocturnal, daytime and cognitive symptoms. The questionnaire contains history related to snoring, restless sleep, night sweating, frequent awakening, enuresis, sleeping posture, daytime sleepiness, morning headache and obesity. A child was thought to have OSAS, if the parents answered positively to 7 or more questions. Thus, on the basis of the questionnaire, 47 children were included in the study and made to undergo cardiorespiratory assessment. Children with craniofacial syndromes and congenital heart disease were excluded from the study.
After obtaining informed consent from parents, detailed history was obtained and clinical examinations were carried out. Anthropometric parameters like weight, height and vital signs like heart rate, respiratory rate and oxygen saturation (SpO2) were recorded. The vital signs like respiratory rate, heart rate and SpO2 were continuously monitored and recorded by Resmed apparatus. BMI was estimated for each child. Adenoid enlargement was confirmed by lateral neck radiographs. Oxygen saturation was monitored and AHI was estimated in CRP (Make: ResMed, Model: Apnoea Link Air).
Statistical Analysis
Data was collected and entered in Gnumeric Worksheet (version: 1.12.46). After doing descriptive analysis, non parametric Mann-Whitney test was done to find out any significant difference in median values of AHI among clinical sub groups of sex and adenoid status. Regression analysis was done between AHI values and BMI. Non parametric tests and regression analysis were done with basic statistical packages in R programming language (The R Foundation for Statistical Computing Version: 3.6.3., Platform: x86_64-pc-linux-gnu (64-bit). Plots were produced in gg plot2 (version: 3.3.3) package in R.
Results
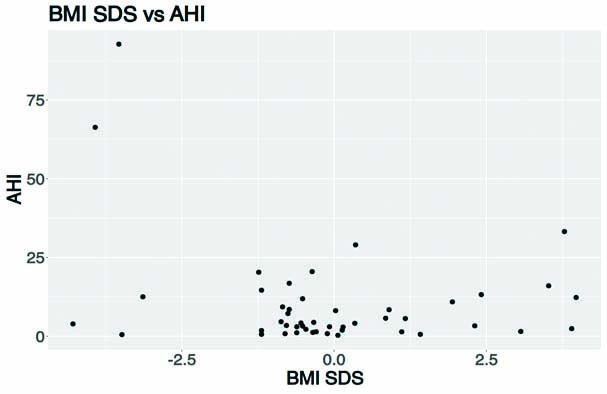
Of the total 1500 children screened by parental questionnaire, 47 (3.1%) children scored 7 and above. On analysis of the subjects, it was found that there was male predominance among the study population (61.7%). On clinical examination, 22 (46.8%) children were found to have adenoid enlargement. When compared with children having no adenoid enlargement, the difference was found to be statistically insignificant (p-value=0.7705) [Table/Fig-1]. It was found that maximum occurrence of OSAS was at the age of 6 years (25.5%) (n=12). More than 50% of children fell in the mild and normal categories OSA based on their AHI score [Table/Fig-2]. There was a poor correlation between BMI SD scores and AHI without any significant association(r=-0.266, p-value=0.07087) [Table/Fig-3].
Distribution of sex, adenoid status, age and BMI among children with Obstructive Sleep Apnoea Syndrome.
| Parameter | Frequency | p-value |
|---|
| Sex* |
| Male | 29 (61.7%) | 0.1447 |
| Female | 18 (38.3%) |
| Adenoid enlargement* |
| Present | 22 (46.8%) | 0.7705 |
| No adenoid enlargement | 25 (53.2%) |
| Age |
| 2-4 years | 7 (14.9%) | 0.0001 |
| 5-7 years | 23 (48.9%) |
| 8-10 years | 11 (23.4%) |
| 11-12 years | 6 (12.8%) |
| Body mass index (kg/m2) |
| Mean | 16.95 | - |
| SD | 5.25 |
| Min | 11 |
| Max | 42.7 |
*-sample proportions test with continuity correction
Scaling severity of Obstructive Sleep Apnoea (OSA) based on Apnea Hypopnea Index (AHI) scoring.
| Category | AHI score | n (%) |
|---|
| Normal | ≤1 | 6 (12.8%) |
| Mild | >1 to ≤5 | 20 (42.6%) |
| Moderate | >5 to ≤10 | 7 (14.9%) |
| Severe | >10 | 14 (29.8%) |
Plotting AHI score against Body Mass Index Standard Deviation Scores.
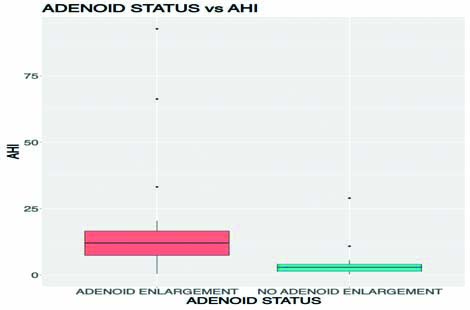
As the distribution of AHI was right skewed, non parametric Mann-Whitney test was applied in sub groups. The difference in median AHI between males and females was not statistically significant (p-value=0.5256). The difference in median AHI values between children with adenoid enlargement and children without adenoid enlargement was statistically significant (p-value <0.001) [Table/Fig-4,5].
Distribution of AHI among Sex and Adenoid Status.
| Parameters | Mean AHI | Median AHI | IQR | p-value |
|---|
| Sex* |
| Male | 10.86 | 5.70 | 1.90-12.50 | 0.5256 |
| Female | 9.26 | 3.35 | 1.73-66.30 |
| Adenoid enlargement* |
| Present | 17.49 | 12.10 | 7.43-92.70 | <0.001 |
| Absent | 3.87 | 2.90 | 1.40-4.10 |
*Mann-Whitney test; p-value <0.05 considered significant
Box Plots of AHI Scores in children with adenoid enlargement and without adenoid enlargement.
Discussion
The diagnosis of OSAS requires a high degree of suspicion in paediatric population and it should be included in routine history taking. However, if left untreated it has lasting impact on the growth and development of the child. If history is taken with care, we can bring more and more children for evaluation and treatment. There are many simple questionnaires which help to identify children with problems that may be indicative of OSAS. By using PSQ, this study found that 3.1% children attending the Outpatient Department suffered from OSAS. Total 47 children were chosen to undertake the cardiorespiratory profile after administration of the questionnaire.
Inoshita A et al., in Japan conducted a study to find age-stratified sex differences in polysomnographic findings and pharyngeal morphology among children with obstructive sleep apnoea [14]. They found sex differences in adolescent patients with OSAS and lack of such differences in preadolescent children with OSAS. In addition, they found that adolescent girls have less severe OSA and better sleep efficiency compared with adolescent boys with OSA. In spain, Fuentes-Pradera MA et al., conducted a cross-sectional study in 226 adolescents of both sexes aged 11-19 years with overnight polysomnography and observed that postpubertal adolescents showed sex differences in clinical and polygraphic parameters related to sleep disordered breathing that were not observed at earlier pubertal stages [17]. These findings support the influence of sex hormones on sex differences in sleep disordered breathing that seem to become apparent at the time of sexual maturation [18]. In the present study male preponderance was not statistically significant (p-value=0.1447). Moreover, the median difference of 2.35 in AHI between male children and female children was not statistically significant (p-value=0.5256).
Total 48.9% of children fell in 5-7 years of age. Probably because this is the age when the adenoid is the maximum in size. The median difference in AHI between children with adenoid enlargement and children without adenoid enlargement was statistically significant (p-value <0.001). There are studies which have found increased association between adenotonsillar hypertrophy and OSAS. A retrospective study conducted at Taiwan by Kang KT et al., observed a positive influence of adenotonsillar hypertrophy on OSA and also observed that the influence of adenoid size on OSAS decreases in adolescence [19]. A study conducted by Ye J et al., at Guangdong province of China also proved the significance of early adenotonsillectomy in children suffering from OSAS [2]. Don DM et al., reviewed overnight polysomnography records of 363 children aged 1-18 years at children Hospital Los Angeles. They observed those children less than three years of age also had an increased frequency of central apnoea than their older counterparts. They advocate that all children less than three years of age with obstructive sleep apnoea continue to be treated as a high-risk population for a period even after adenotonsillectomy [20].
The study conducted by Andersen IG et al., in Denmark in adolescent age group showed relationship between the BMI and incidence of OSAS [13]. In their study, children with overweight/obesity had a significantly higher prevalence of OSA compared with a normal-weight group. Increased BMI SD scores was associated with increased AHI. In the present study the BMI SD scores of 47 children poorly correlated with AHI (r=-0.266, p-value=0.07087). No child beyond 12 years of age was included in the study. Authors presume that in younger children adiposity plays little role when compared to adenoid enlargement.
The overall mean value of AHI is approximately 10.4, this can be easily understood by the population selected by a questionnaire which filters out normal children. Going by AHI, 12.8% children were normal without OSAS. It was found that 42.6% of the children had an AHI which indicated mild OSAS, 14 children had severe OSAS and rest of the children had moderate OSAS as indicated by AHI. Severe cases were referred for adenotonsillectomy, and mild to moderate cases were subjected to steroidal nasal spray.
Limitation(s)
The population selected was small in size and that also contained high risk children selected by questionnaire without any proper control population. AHI index was calculated by Cardiorespiratory Polygraphy in our study. Authors were unable to compare our cardiorespiratory profile findings with that of an overnight polysomnogram to give conclusive evidence regarding the accuracy of cardiorespiratory profile. The lack of a dedicated Polysomnography laboratory with adequate number of technicians who are trained in handling children and infants with provisions to lodge the children and their attenders is an important limitation of the present study. A large population based study with polysomnography as a gold standard and appropriately matched controls may reveal the effectiveness of Cardiorespiratory Polygraphy in diagnosing cases of OSAS in children.
Conclusion(s)
The prevalence rate of OSAS in our paediatric Outpatient Department is 3.1%. There are tools such as PSQ that can be employed as a screening tool to find out the cases of paediatric OSAS. CRP is a cheaper and effective modality to find out AHI. Children with adenoid hypertrophy have higher AHI than children without adenoid hypertrophy. There was a lack of evidence for male predominance in the present study and obesity poorly correlated with AHI score.
*-sample proportions test with continuity correction
*Mann-Whitney test; p-value <0.05 considered significant
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 26, 2021
Manual Googling: Sep 04, 2021
iThenticate Software: Sep 20, 2021 (16%)
[1]. Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, American Academy of Pediatrics. Diagnosis and management of childhood obstructive sleep apnea syndromePediatrics 2012 130(3):576-84.Epub 2012 Aug 2710.1542/peds.2012-167122926173 [Google Scholar] [CrossRef] [PubMed]
[2]. Ye J, Liu H, Zhang GH, Li P, Yang QT, Liu X, Li Y, Outcome of adenotonsillectomy for obstructive sleep apnea syndrome in childrenAnn Otol Rhinol Laryngol 2010 119(8):506-13.10.1177/00034894101190080220860275 [Google Scholar] [CrossRef] [PubMed]
[3]. Shine NP, Coates HL, Lannigan FJ, Obstructive sleep apnea, morbid obesity, and adenotonsillar surgery: A review of the literatureInt J Pediatr Otorhinolaryngol 2005 69:1475-82.10.1016/j.ijporl.2005.08.00816171876 [Google Scholar] [CrossRef] [PubMed]
[4]. Blechner M, Williamson AA, Consequences of Obstructive Sleep Apnea in ChildrenCurr Probl Pediatr Adolesc Health Care 2016 46(1):19-26.10.1016/j.cppeds.2015.10.00726631839 [Google Scholar] [CrossRef] [PubMed]
[5]. Fava C, Montagnana M, Favaloro EJ, Guidi GC, Lippi G, Obstructive sleep apnea syndrome and cardiovascular diseasesSemin Thromb Hemost 2011 37(3):280-97.Epub 2011 Mar 3110.1055/s-0031-127309221455862 [Google Scholar] [CrossRef] [PubMed]
[6]. Tseng PH, Lee PL, Hsu WC, Ma Y, Lee YC, Chiu HM, A Higher Proportion of Metabolic Syndrome in Chinese subjects with sleep-disordered breathing: A case-control study based on electrocardiogram-derived sleep analysisPLoS One 2017 12:e016939410.1371/journal.pone.016939428081171 [Google Scholar] [CrossRef] [PubMed]
[7]. Farrell PC, Richards G, Recognition and treatment of sleep-disordered breathing: An important component of chronic disease managementJ Transl Med 2017 15:11410.1186/s12967-017-1211-y28545542 [Google Scholar] [CrossRef] [PubMed]
[8]. Alonso Alvarez ML, Terán Santos J, Cordero Guevara JA, Navazo Egüia AI, Ordax Carbajo E, Masa Jiménez JF, Fiabilidad de la poligrafía respiratoria para el diagnóstico del síndrome de apneas-hipopneas durante el sueño en niños [Reliability of respiratory polygraphy for the diagnosis of sleep apnea-hypopnea syndrome in children]Arch Bronconeumol 2008 44(6):318-23.Spanish10.1157/13123089 [Google Scholar] [CrossRef]
[9]. Tan HL, Gozal D, Ramirez HM, Bandla HP, Kheirandish-Gozal L, Overnight polysomnography versus respiratory polygraphy in the diagnosis of pediatric obstructive sleep apneaSleep 2014 37(2):255-60.10.5665/sleep.339224497654 [Google Scholar] [CrossRef] [PubMed]
[10]. Ruehland WR, Rochford PD, O’Donoghue FJ, Pierce RJ, Singh P, Thornton AT, The New AASM Criteria for Scoring Hypopneas: Impact on the Apnea Hypopnea IndexSleep 2009 32(2):150-57.10.1093/sleep/32.2.15019238801 [Google Scholar] [CrossRef] [PubMed]
[11]. Dehlink E, Tan HL, Update on paediatric obstructive sleep apnoeaJ Thorac Dis 2016 8(2):224-35.Doi: 10.3978/j.issn.2072-1439.2015.12.04 [Google Scholar]
[12]. Chang SJ, Chae KY, Obstructive sleep apnea syndrome in children: Epidemiology, pathophysiology, diagnosis and sequelaeKorean J Pediatr 2010 53(10):863-71.10.3345/kjp.2010.53.10.86321189956 [Google Scholar] [CrossRef] [PubMed]
[13]. Andersen IG, Holm JC, Homøe P, Obstructive sleep apnea in children and adolescents with and without obesityEur Arch Otorhinolaryngol 2019 276(3):871-78.10.1007/s00405-019-05290-230689039 [Google Scholar] [CrossRef] [PubMed]
[14]. Inoshita A, Kasai T, Matsuoka R, Sata N, Shiroshita N, Kawana F, Age-stratified sex differences in polysomnographic findings and pharyngeal morphology among children with obstructive sleep apneaJ Thorac Dis 2018 10(12):6702-10.10.21037/jtd.2018.11.0930746215 [Google Scholar] [CrossRef] [PubMed]
[15]. Lumeng JC, Chervin RD, Epidemiology of pediatric obstructive sleep apneaProc Am Thorac Soc 2008 5(2):242-52.10.1513/pats.200708-135MG18250218 [Google Scholar] [CrossRef] [PubMed]
[16]. Chervin RD, Hedger K, Dillon JE, Pituch KJ, Pediatric sleep questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioural problemsSleep Med 2000 1(1):21-32.10.1016/S1389-9457(99)00009-X [Google Scholar] [CrossRef]
[17]. Fuentes-Pradera MA, Sánchez-Armengol Á, Capote-Gil F, Quintana-Gallego E, Carmona-Bernal C, Polo J, Effects of sex on sleep-disordered breathing in adolescentsEuropean Respiratory Journal 2004 23:250-54.10.1183/09031936.03.0002200314979499 [Google Scholar] [CrossRef] [PubMed]
[18]. Pickett CK, Regensteiner JG, Woodard WD, Hagerman DD, Weil JV, Moore LG, Progestin and estrogen reduce sleep-disordered breathing in postmenopausal womenJ Appl Physiol (1985) 1989 66(4):1656-61.10.1152/jappl.1989.66.4.16562543656 [Google Scholar] [CrossRef] [PubMed]
[19]. Kang KT, Chou CH, Weng WC, Lee PL, Hsu WC, Associations between adenotonsillar hypertrophy, age, and obesity in children with obstructive sleep apneaPLoS One 2013 8(10):e7866610.1371/journal.pone.007866624205291 [Google Scholar] [CrossRef] [PubMed]
[20]. Don DM, Geller KA, Koempel JA, Ward SD, Age specific differences in pediatric obstructive sleep apneaInt J Pediatr Otorhinolaryngol 2009 73(7):1025-28.10.1016/j.ijporl.2009.04.00319410303 [Google Scholar] [CrossRef] [PubMed]