Case Report
A 42-year-old male patient, reported to the Department of Oral Medicine and Radiology, with a chief complaint of dull and continuous pain in the upper right back tooth region while eating since five days.
Intraoral examination revealed tenderness on percussion in relation to 16, 17 and 18. Gingiva was oedematous and pink in colour with melanin pigmentation. Generalised gingival recession from cementoenamel junction to cervical third of the root was evident. There was no swelling reported in the associated area and the teeth did not exhibit any mobility [Table/Fig-1a]. The patient gave a history of extraction in relation to 22, 24 and 47 three years ago, and subsequently a fixed prosthesis extending from 21 to 25 was provided. The patient also had a habit of smoking 8-10 bidis per day, for 15-20 years. There was no significant medical history. Based on the patient’s history and clinical examination, a provisional diagnosis of chronic apical periodontitis in relation to 16, 17 and 18 was made.
a) Intraoral photograph with no sign of swelling; b) Orthopantomogram (OPG) revealed a unilocular well-defined radiolucency with a radiopaque sclerotic border in the right maxillary anterior region, involving the apices of 11, 12, 13 and 14; c) Cone Beam Computed Tomography image in axial plane: An oval shaped, unilocular homogenously hypodense region extending from the periapical portion of 11 to 21 palatally, measuring 9×7.05×8.85 mm in size; d) Medium Field of View CBCT scan of maxillary arch revealing a unilocular homogenously hypodense region extending from mesial aspect of 11 to 15; e) Cone Beam Computed Tomography image in axial plane: A large ellipsoidal shaped, unilocular homogenously hypodense region extending from mesial aspect of 11 to 15, measuring 21.73×13.29×15.56 mm in size.
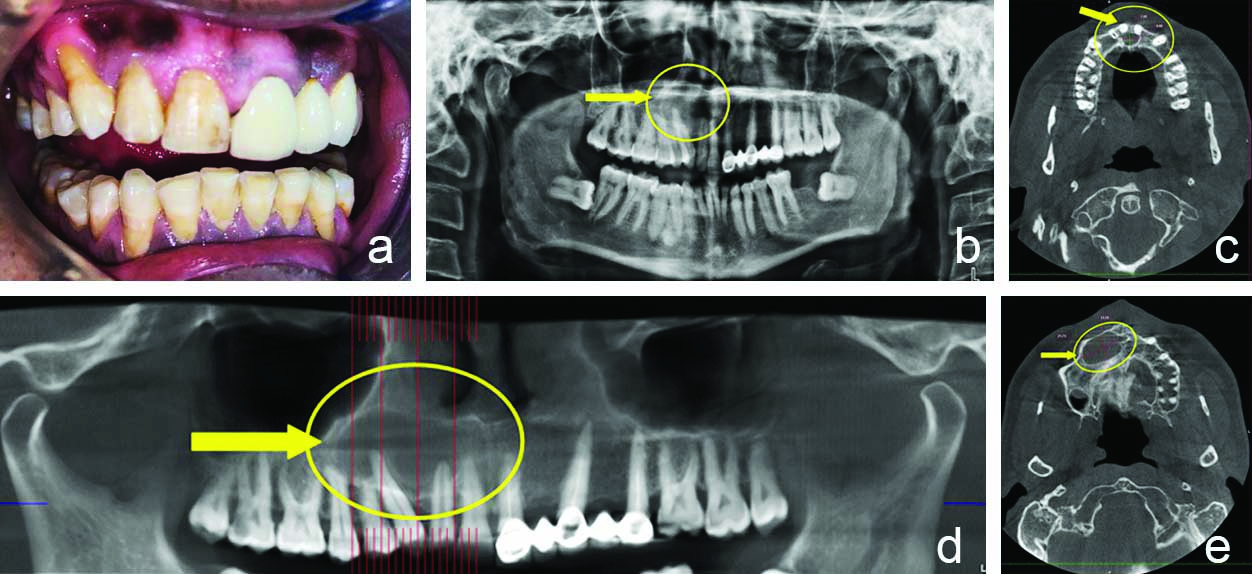
On radiographical examination, Orthopantomogram (OPG) revealed an ill-defined radiolucency on the distal surface of the crown region of 17 and on the mesial surface of the crown region of 18, indicating proximal caries in relation to 17 and 18. There was an additional incidental finding in the OPG, which revealed a unilocular well-defined radiolucency with a radiopaque sclerotic border in the anterior maxillary region, involving the apices of 11, 12, 13 and 14 [Table/Fig-1b]. On clinical examination, the teeth showed no mobility and the percussion test was also negative. Pulp vitality test was done using Waldent Electric Pulp Vitality Tester in relation to 11, 12, and 13 which showed immediate response, indicating that the associated teeth were vital.
Cone Beam Computed Tomography (CBCT) revealed two separate unilocular homogeneously hypodense regions with radiopaque sclerotic borders in the maxillary arch: An oval shaped lesion extending from the periapical portion of 11 to 21 palatally, measuring 9.00 mm (mesiodistally)×7.05 mm (labiopalatally)×8.85 mm (superior-inferiorly) in size [Table/Fig-1c] and a large ellipsoidal shaped lesion extending from mesial aspect of 11 to 15, measuring 21.73 mm×13.29 mm×15.56 mm in size [Table/Fig-1d and e]. The lesion involved both the anterior and posterior regions in the maxilla. Based on the radiological findings, a diagnosis of odontogenic cyst was made and differential diagnoses of odontogenic keratocyst, nasopalatine cyst and unicystic ameloblastoma were taken into consideration. Routine blood investigations were done. The patient was referred to the Department of Oral and Maxillofacial Surgery for cyst enucleation and was also referred to the Department of Conservative and Endodontics for root canal treatment, followed by post and core and fixed prosthesis in relation to 17 and restoration of 18.
In the Department of Oral and Maxillofacial Surgery, the surgical site was painted with cipladine 5% solution to achieve asepsis and then the patient was draped. Infraorbital and nasopalatine blocks were given with Indoco Warren Lignox Lignocaine 2% with adrenaline 1:80,000 concentration. A crevicular incision with posterior releasing with Bard Parker blade (BP blade) number-15 was placed from 16 to 23 region, and then the mucoperiosteal flap of full thickness was raised till the vestibular depth. A bony window was created with the help of a round bur and the cystic lining was exposed. The cystic lesion was completely enucleated and chemical cauterization with carnoy’s solution for both the cyst was performed [Table/Fig-2a].
a) Enucleation with curettage; b) Two soft tissue specimens were received by the Department of Oral Pathology, measuring 20×15 mm from the labial side, and 8×6 mm from the palatal side; Macroscopically, they were creamish-white in colour and firm in consistency.

Irrigation of the cystic cavity was done with cipladine 5% solution and then the flap was closed by interrupted suture with Ethicon vicryl suture 3-0 polyglactin 910 SH-1 27" coated absorbable braid violet and 22 mm 1/2 circle reverse cutting needle taper point.
The excised specimen was sent to the Department of Oral Pathology for histopathological evaluation. Two soft tissue specimens were received by the Department of Oral Pathology, measuring 20 mm×15 mm from the labial side and 8 mm x 6 mm from the palatal side. Macroscopically, the submitted tissues were firm in consistency and creamish-white in colour [Table/Fig-2b].
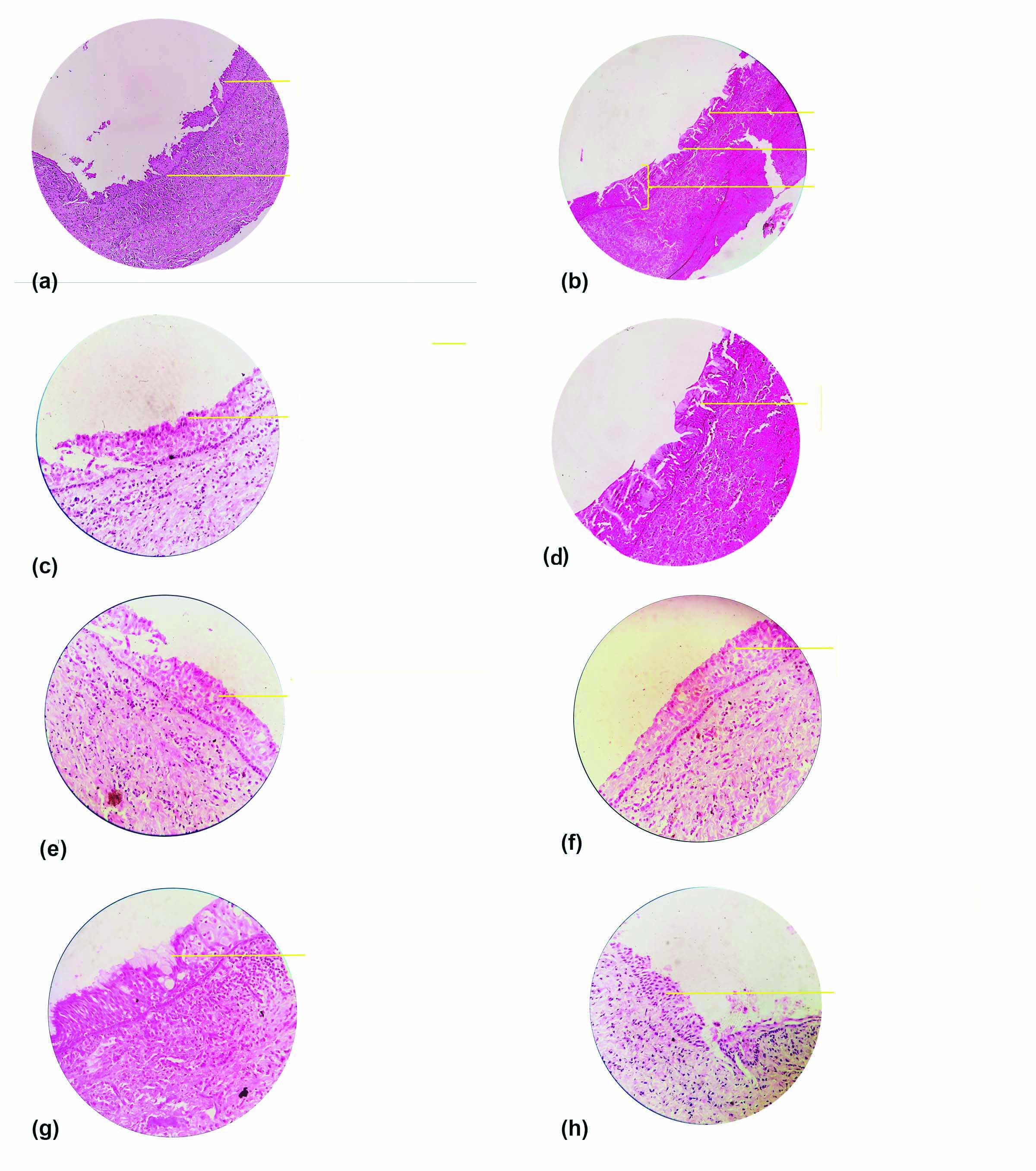
Microscopic examination of Haematoxylin and Eosin (H&E) stained soft tissue specimens exhibited a cystic lining that was non keratinised stratified squamous type [Table/Fig-3a] and was of variable thickness with a flat interface connective tissue wall [Table/Fig-3b]. The superficial epithelial layer showed hobnail cells and the basal and parabasal layers showed clear vacuolated cells. The epithelial layer had papillary projections with glandular microcyst or duct-like structures throughout the epithelium [Table/Fig-3b-f]. At places, the epithelial layer exhibited ciliated pseudostratified columnar cells with intraepithelial mucous goblet cells [Table/Fig-3b,g]. At one place, plaque like thickening was evident [Table/Fig-3h]. Underlying connective tissue showed bundles of collagen fibres, dense inflammatory cell infiltrate, blood vessels and macrophages. Correlating clinically, radiographically and histopathologically, a final diagnosis of GOC was made.
a) Microscopic examination of H&E stained soft tissue section exhibited a cystic lining that was non keratinised stratified squamous type with flat connective tissue wall interface. The epithelial lining showed papillary projections (10 X); b) Microscopic examination of H&E stained soft tissue section exhibited a cystic lining with variable thickness. The epithelial layer was composed of glandular microcyst or duct-like structures and mucous goblet cells (10 X); c) Microscopic examination of H&E stained soft tissue section exhibited hobnail cells on the surface eosinophilic cuboidal cells (40 X); d) Microscopic examination of H&E stained soft tissue section exhibited apocrine snouting of hobnail cells in the superficial epithelial layer (40 X); e) Microscopic examination of H&E stained soft tissue section exhibited intra-epithelial microcysts or duct like spaces (40 X); f) Microscopic examination of H&E stained soft tissue section exhibited papillary projections (tufting) into the cystic lumen (40 X); g) Microscopic examination of H&E stained soft tissue section exhibited mucous goblet cells in the epithelial layer (40 X); h) Microscopic examination of H&E stained soft tissue section exhibited plaque like thickenings in the epithelial layer (40 X).
The patient was followed-up for a year and there was no sign of recurrence [Table/Fig-4].
The patient was followed-up for a year and there was no sign of recurrence.

Discussion
Odontogenic cysts are relatively common lesions occurring in the oral cavity, and they form a major part of the total biopsies received by any Oral Pathologist. This diversified group of lesions exhibit varying presentations in the maxilla and mandible, ranging from a small innocuous lesion to a highly aggressive and destructive lesion, which may even transform into a malignancy [1].
GOC was first documented in 1987, by Padayachee Arun and Van Wyk CW as Sialo-Odontogenic Cyst. Two cases were reported having identical clinical, radiographical and histopathological characteristics of both botryoid odontogenic cyst and central mucoepidermoid tumor. This cyst was suggested to be of salivary gland origin, as it exhibited mucous cells and pools of mucin in the epithelial lining [2]. Later Gardner DG et al., in 1988, described eight cases of this cyst in his article and renamed it as GOC, suggesting that the term sialo odontogenic cyst was used informally and so should be abandoned. The cystic lining exhibited ball-like plaques, reminiscent of those seen in the periodontal cysts and adenomatoid odontogenic cysts with pools of mucicarmine positive material within the epithelium, which suggested it to be of odontogenic origin [3].
In 2017, World Health Organisation (WHO) classified GOC under odontogenic cysts histopathologically, and described it as developmental cyst with stratified squamous epithelial lining that simulates salivary gland or glandular differentiation” [4]. There are less than 200 cases of GOC reported all over the world so far [5]. It is clinically rare and histopathologically unusual cyst with an unpredictable and potentially aggressive behaviour, with a frequency of 0.012-1.3% of all the jaw cysts [6,7]. It is common in patients aged between 40-70 years, with a male predilection [8].
Clinically, patients usually exhibit a painless, slowly growing intra-osseous lesion, involving the anterior region of the mandible, but in the literature, there are few cases reported involving the anterior region of the maxilla [9-12]. Urs AB et al., have observed expansion in relation to the cystic lesion along with thinning, erosion, or perforation of the cortical plates in some of their cases [13]. At times, the lesion can also cause nerve compression or any other secondary infections in the jaw, which can lead to severe pain [14]. Li L et al., in 2016, described the recurrence of pain in their patient due to compression of the posterior superior alveolar nerve by the lesion [7]. In the present case, the lesion was completely asymptomatic, involving both the maxillary anterior and posterior region, which is quite uncommon. Radiographically, GOC is localised intraosseously presenting as either a unilocular or a multilocular radiolucent lesion, surrounded by radiopaque sclerotic margin [8]. At times, GOC can also cause perforation of the cortex bone along with tooth displacement and resorption [9]. It can mimic other developmental cysts like dentigerous cysts, lateral periodontal cyst or globulomaxillary cyst [15,16]. Their differentiating features are presented in [Table/Fig-5]. In this case, GOC presented as two separate unilocular lesions located in the anterior and posterior regions of the maxilla, crossing the midline which is quite rare and there is no such case reported in the scientific literature.
Radiographic differentiating features of GOC [16].
| Glandular odontogenic cyst | Dentigerous cyst | Lateral periodontal cyst | Globulomaxillary cyst |
|---|
| Well-defined radiolucency, with scalloped sclerotic margins. | Well-defined radiolucency, usually associated with hyperostotic borders unless they are secondarily infected. | Cyst is seen as a round or ovoid, well-defined radiolucency with hyperostotic borders. | Cyst appears as pear-shaped or tear-shaped radiolucency. Small end of the pear is directed toward the crest of alveolar ridge. |
| It is a unilocular or multilocular radiolucency. | Usually, it is unilocular but sometimes it may appear multilocular. | It is a unilocular lesion. | It is a unilocular region. |
| It is usually found at the apex of the tooth. | Cyst may envelop the crown symmetrically, but it may expand laterally from the crown. Cyst is usually attached with the cementoenamel junction. | It is usually found between the cervical margins and the apex of adjacent root surfaces and may or may not be in contact with root surfaces. | It develops between apex of both the vital teeth. |
| Mostly associated with anterior mandibular region. | Mostly associated with impacted mandibular and maxillary third molars and canines. | Mostly associated with vital mandibular canine and premolar area and is followed by the anterior region of the maxilla. | Mostly associated with maxillary lateral incisor and canine area. |
| Age: 30-40 years | Age: 11-30 years | Age: 22-85 years | Age: 20-40 years |
Histopathologically, GOC shows multiple features. However, often all the features are seen only at focal areas or not all the features are seen in the cyst. In addition, few of these features are known to occur in other lesions such as Botryoid-Odontogenic Cyst, Radicular Cyst, Dentigerous Cyst, or Low-Grade-Mucoepidermoid Carcinoma [17].
To avoid this confusion, Gardner DG et al., gave few microscopic parameters that were adapted from previously reported microscopic features of GOC [Table/Fig-6] [3].
Microscopic features given by Gardner DG et al., (1988) [3]
| The cyst is lined with stratified squamous epithelium of varying thickness, exhibiting a flat interface with the underlying connective tissue without any inflammatory infiltrate. |
| The superficial layer of the epithelium consists of eosinophilic cuboidal cells making the surface irregular and sometimes papillary. |
| Cilia may be present on the surface of eosinophilic cuboidal cells. |
| Pools of mucicarmine-positive material are present within the epithelium. |
| Mucous cells are usually prominent on the surface. |
| Basal cells are sometimes hyperchromatic and may be vacuolated. |
| Epithelial cells may be arranged into apparently spherical structures. |
| Irregularly shaped calcifications may be present in the connective tissue beneath the epithelium. |
The features of Gardner DG et al., were later modified by Kaplan I et al., and divided the features into major and minor criteria. As a guideline, authors suggested that atleast focal presence of each of the major criteria should be mandatory, whereas minor criteria need not be present for diagnosis, but may just support it [14] [Table/Fig-7].
Microscopic features given by Kaplan I et al., (2005) [14].
| Major criteria | Minor criteria |
|---|
| Squamous epithelial lining with flat connective tissue wall interface, lacking basal palisading [Table/Fig-3a] | Lining epithelium with papillary projections [Table/Fig-3a] |
| Variations in thickness of epithelial lining with or without epithelial sphere or whorls or focal luminal proliferation [Table/Fig-3b] | Ciliated cells |
| Cuboidal eosinophilic cells or “hobnail” cells [Table/Fig-3c] | Multicystic or multiluminal architecture |
| Intraepithelial mucous pool with mucous goblet cells, with or without crypts lined by mucous-producing cells [Table/Fig-3b] | Clear or vacuolated cells in basal or spinous layer |
| Glandular microcyst or duct-like structure in the epithelial layer [Table/Fig-3b] | |
Fowler CB et al., recorded ten microscopic parameters of GOC [18] [Table/Fig-8]. Authors suggested that a combination of specific microscopic features, not necessarily corresponding with their major and minor criteria, can appear to be helpful in making an accurate diagnosis of GOC. So, he proposed the presence of 7 or more microscopic parameters that were highly predictive of diagnosis of GOC, and presence of 5 or less microscopic parameters that were highly predictive of non GOC or GOC mimicker [18].
Microscopic features given by Fowler CB et al., (2011) [18].
| Surface eosinophilic cuboidal cells, also called “hobnail cells” [Table/Fig-3c] |
| Intraepithelial microcysts or duct-like spaces [Table/Fig-3e] |
| Apocrine snouting of hobnail cells [Table/Fig-3d] |
| Clear or vacuolated cells |
| Variable thickness of the cyst lining [Table/Fig-3b] |
| Papillary projections or “tufting” into the cyst lumen [Table/Fig-3a,f] |
| Mucous goblet cells [Table/Fig-3g] |
| Epithelial spheres or plaque-like thickenings [Table/Fig-3h] |
| Cilia on the surface of eosinophilic cuboidal cells |
| Multiple compartments |
In the present case, on histopathological evaluation, the haematoxylin and eosin slide revealed non keratinised stratified squamous type epithelium of varying thickness. The superficial epithelial layer showed hobnail cells and the basal and parabasal layers showed clear vacuolated cells. The epithelial layer had papillary projections with glandular microcyst or duct-like structures throughout the epithelium. At places, the epithelial layer exhibited ciliated pseudostratified columnar cells with intraepithelial mucous goblet cells. At one place, plaque like thickening was evident. These features led to the diagnosis of GOC.
Treatment is generally influenced by the size of lesion, involvement of the teeth, cortical bone perforation, history of recurrence and proximity to vital anatomic structures. The preferred choice of treatment involves enucleation or curettage, and to avoid recurrence 1.0 to 1.5 cm margins and some overlying mucosa is resected from the jaw [19]. The GOC has been associated with high recurrence rate of 21-55%, because of its multilocular nature, tendency of thin epithelium to separate from underlying connective tissue capsule thus making removal difficult at the time of surgery and because of conservative treatment of the lesion [16]. Follow-up should be continued for atleast six months to three years by clinical examination and radiographic examination, to avoid recurrence of this cyst [19].
Conclusion(s)
Glandular Odontogenic Cyst (GOC) being a rare and a unique lesion, exhibits many variations clinically and radiographically. Hence, it can create a problem in diagnosis, as it mimics many other odontogenic cysts. A proper histopathological evaluation and its correlation with the clinical findings is necessary. Since, the lesion is aggressive and is associated with high recurrence rate, it further more emphasises the need of correct diagnosis of this rare entity. It has been suggested to follow-up these cases for a period of one year.
[1]. Gul S, Shah AA, Bashir S, Bashir S, Different treatment modalities for OKC of jawsInt J Res Health Allied Sci 2020 6(3):118-20. [Google Scholar]
[2]. Padayachee A, Van Wyk CW, Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: Sialo-odontogenic cyst?J Oral Pathol 1987 16(10):499-504.10.1111/j.1600-0714.1987.tb00680.x3127563 [Google Scholar] [CrossRef] [PubMed]
[3]. Gardner DG, Kessler HP, Morency R, Schaffner DL, The glandular odontogenic cyst: An apparent entityJ Oral Pathol 1988 17(8):359-66.10.1111/j.1600-0714.1988.tb01298.x3146620 [Google Scholar] [CrossRef] [PubMed]
[4]. El-Naggar Adel K, John KC, Chan Grandis J. Rubin, Takashi Takata, Pieter J, Slootweg. WHO Classification of Head and Neck Tumours 2017 Print [Google Scholar]
[5]. Kadam VD, Changule GR, Choudhary SH, Gade LP, Glandular odontogenic cyst in a young Indian female: A rare case report with review of literatureJ Indian Acad Oral Med Radiol 2020 32(3):30010.4103/jiaomr.jiaomr_34_20 [Google Scholar] [CrossRef]
[6]. Chandolia Betina Bajpai Manas Arora Manika (2017). Glandular Odontogenic CystJ Coll Physicians Surg Pak 2017 27(3):S23-25. [Google Scholar]
[7]. Li L, Singh P, Ping J, Li X, Glandular odontogenic cyst of posterior maxilla: A rare entityInt J Case Rep Imag 2016 7(4):254-60.10.5348/ijcri-201644-CR-10632 [Google Scholar] [CrossRef]
[8]. Yanduri S, Deepa KK, Kumar BV, Suma S, Madhura MG, Vakade CD, Glandular odontogenic cyst: Analysis of clinicopathological features of five casesIndian Journal of Oral Health and Research 2017 3(1):4010.4103/ijohr.ijohr_22_17 [Google Scholar] [CrossRef]
[9]. Olawuyi AB, Effiom OA, Ogundana O, Odukoya O, Glandular odontogenic cyst of the maxilla in a Nigerian: Case report and review of literaturePort Harcourt Med J 2017 11:103-06.10.4103/phmj.phmj_1_17 [Google Scholar] [CrossRef]
[10]. Jafarian AH, Rahpeyma A, Khajehahmadi S, Recurrent glandular odontogenic cyst of maxilla-a case reportIran J Pathol 2015 10(2):160 [Google Scholar]
[11]. Rao JB, Kumar KJ, Kumar BP, Glandular odontogenic cyst involving the posterior part of maxillary sinus, a rare entityJ Maxillofac Oral Surg 2010 9(1):72-75.10.1007/s12663-010-0020-023139573 [Google Scholar] [CrossRef] [PubMed]
[12]. Ogura I, Tsuchimochi M, Ono J, Kanri Y, Okada Y, Fujii K, Glandular odontogenic cyst: a report of four casesOral Science International 2017 14(2):43-49.10.1016/S1348-8643(17)30018-6 [Google Scholar] [CrossRef]
[13]. Urs AB, Kumar P, Augustine J, Malhotra R, Glandular odontogenic cyst: Series of five casesJ Oral Maxillofac Pathol 2017 21(2):23910.4103/jomfp.JOMFP_167_1628932033 [Google Scholar] [CrossRef] [PubMed]
[14]. Kaplan I, Gal G, Anavi Y, Manor R, Calderon S, Glandular odontogenic cyst: Treatment and recurrenceJ Oral Maxillofac Surg 2005 63(4):435-41.10.1016/j.joms.2004.08.00715789313 [Google Scholar] [CrossRef] [PubMed]
[15]. Shah M, Kale H, Ranginwala A, Patel G, Glandular odontogenic cyst: A rare entityJ Oral Maxillofac Pathol 2014 18(1):8910.4103/0973-029X.13192224959044 [Google Scholar] [CrossRef] [PubMed]
[16]. Ferreira JC, Vêncio EF, de Sá RT, Gasperini G, Glandular odontogenic cyst in dentigerous relationship: An uncommon case reportCase Rep Dent 2019 2019:864715810.1155/2019/864715831355014 [Google Scholar] [CrossRef] [PubMed]
[17]. Shah AA, Sangle A, Bussari S, Koshy AV, Glandular odontogenic cyst: A diagnostic dilemmaIndian J Dent 2016 7(1):3810.4103/0975-962X.17937127134453 [Google Scholar] [CrossRef] [PubMed]
[18]. Fowler CB, Brannon RB, Kessler HP, Castle JT, Kahn MA, Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosisHead Neck Pathol 2011 5(4):364-75.10.1007/s12105-011-0298-321915706 [Google Scholar] [CrossRef] [PubMed]
[19]. Marx RE, Stern D, Oral and maxillofacial pathology: A rationale for diagnosis and treatment 2012 Hanover ParkQuintessence Publishing Company [Google Scholar]