Supracristal Ventricular Septal Defect (VSD) develops Aortic Regurgitation (AR) with the passage of time due to prolapse of the right coronary cusp. It brings clinical attention in early child hood with an incidental continuous murmur, recurrent respiratory tract infection of failure to thrive. This report is about a rare case of 52-year-old female who presented with increased fatiguability since the last six months. Clinical examination revealed the presence of cardiomegaly with holosystolic-diastolic murmur in Left Upper Sternal Border (LUSB). Echocardiography revealed the presence of supracristal VSD with moderate AR without prolapsing aortic leaflet or dilatation of aortic sinus. In view of presence of moderate AR, the patient was advised to be on Angiotensin Receptor Blocker (ARB) with regular follow-up to monitor the progression of AR. Such a late index presentation of supracristal VSD with moderate AR in fifth decade of life has not been described in literature so far. To conclude, nature retards the natural history with bless in disguise.
Coronary, Cusp, Echocardiography, Prolapse
Case Report
A 52-year-old female presented to the CO department with chief complaint of easy fatiguability, since last six months. She had no history of exertional angina, presyncope or syncope in the past. Patient had a thumping sensation in left chest in left lateral lying down position since last six months. She was non diabetic, non hypertensive without any family history of coronary artery disease. There was no history of recurrent respiratory tract infection in early childhood and also there was no history suggestive of acute rheumatic fever in childhood. There was no history of congenital heart disease in her paternal family and siblings.
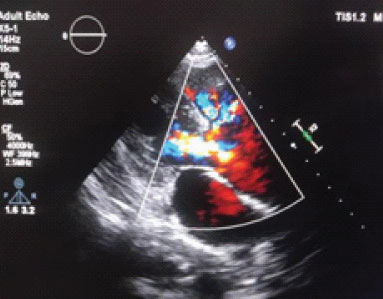
Clinical examination revealed the blood pressure of 150/60 mmHg in right arm supine position with the heart rate of 86 beats per minute. Cardiovascular system examination revealed cardiomegaly with apex beat in 6th intercostal space one cm lateral to mid clavicular line, forceful, ill-sustained in nature with presence of holosystolic- diastolic murmur in left upper parasternal border. Electrocardiogram revealed presence of left ventricular hypertrophy with presence of diastolic strain suggestive of volume overload condition. Echocardiography revealed the presence of small supracristal VSD with peak systolic gradient of 82 mmHg with presence of moderate AR [Table/Fig-1,2] with regurgitant jet /LVOT diameter of 8/20 mm and Pressure Half Time (PHT) of 360 msec. Interestingly, she did not have prolapsing right aortic cusp or aortic sinus dilatation.
Small supracristal VSD without RCC prolapse or coronary sinus dilatation;

Color doppler revealing supra cristal VSD with moderate AR.
In view of moderate AR, she was advised to be on angiotensin receptor blocker (Losartan 25 mg twice daily) with close follow-up to look for the progression of AR. ARBs relax the ascending aorta, intra-aortic pressure decreases causing a decrease in aortic and left ventricular gradient and subsequently the amount of regurgitation decreases. In brief, it halts the phenomenon of AR begets AR or retards the progression of AR. In the event of future progression to severe AR, it was planned to subject patient to surgical aortic valve replacement with pericardial patch closure of ventricular septal defect. She was followed-up after three and six months which revealed no significant progression of AR and she was doing well with ARB.
Discussion
Although supracristal VSD with Aortic Insufficiency (AI) is a well-recognised entity, controversy surrounds the condition, particularly in the areas of natural history, pathological anatomy, and surgical therapy. Laubry C and Pezzi C in 1921 first recognised the association of the two lesions [1]. A 5-8% of VSD are located high in the right ventricular outflow tract between pulmonary valve superiorly and crista supraventricularis inferiorly [1]. These defects are termed supracristal in contradistinction to the more typical membranous septal defect which is infracristal in location. These lesions, which result from abnormalities in fusion of the embryonal conal septum, are of particular importance because of the unusually high incidence of associated anomalies, particularly involving the aortic valve.
The AR, balloon like dilatation of the right coronary sinus of Valsalva, prolapse of the right coronary cusp and, rarely the left coronary cusp into the right ventricular infundibulum, and right coronary sinus of Valsalva-right ventricular fistula have all been reported as complications of the supracristal VSD [2-6]. The lesion is also an integral component of the Taussig Bing anomaly (double outlet right ventricle with supracristal VSD) and is present in the majority of patients with aortic arch interruption [7,8]. Its presence may range as high as 25% in oriental patients with tetralogy of Fallot [9]. The index patient had a rare isolated adulthood presentation of supracristal VSD with AR without prolapsing right coronary cusp or dilatation of coronary sinus in an elderly 52-year-old female; nature has retarded the disease progression to bless her in disguise.
Smith KA et al., reviewed their experience in 29 patients with VSD and AR; the most common cause of AR was a prolapsed aortic valve cusp, which occurred in 19 patients, aneurysmal dilatation of aortic sinus accounted for the regurgitation in three patients, two patients had both abnormalities and, in two patients no cause for the AR was found [10]. Those patients with aortic cusp prolapse commonly had large VSDs, of which nearly a third was supracristal. Because of cusp prolapse into the VSD, and sometimes into the right ventricular outflow tract, the findings at cardiac catheterisation often suggested erroneously that the VSD was small and that infundibular obstruction was present. The present case was unique in presentation in the fifth decade of life with AR without prolapse of aortic valve cusp or dilatation of aortic sinus.
Hitherto, proposed anatomic classification of VSD with AR as follows: type I, supracristal VSD and AI; type II, infracristal VSD and AI; type III, infracristal VSD and AI with infundibular Pulmonic Stenosis (PS);and type IV, supracristal VSD and AI with infundibular PS. Supracristal VSD with AR was again classified into three types as follows: Type Ia: VSD is supracristal and there is no herniation of the aortic valve cusp, Type Ib: VSD is supracristal and there is a thin conal muscular rim just beneath the pulmonic valve and the herniation of the aortic valve cusp is usually mild or moderate, Type Ic: VSD is supracristal and there is no conal muscle beneath the pulmonic valve. Aortic and pulmonic valves are side by side and the herniation of the aortic valve cusp is usually moderate or severe [11]. This case is typical of type 1a supracristal VSD with AR without prolapse of aortic cusp which is rare to encounter in clinical practice with index presentation in adulthood.
Somnath HS et al., studied supracristal VSD with AR in 362 Indian children, 16% had supracristal VSD and 10% had supracristal VSD with AR [12]. Mean age of children with supracristal VSD with AR was 13.4 years (2-45). Half of the children with supracristal VSD with AR had grade I or II AR and another half of them had grade III or IV AR. In most of the children with supracristal VSD with AR, left to right shunt was small with normal pulmonary pulmonary artery pressure. Prolapse of RCC was more common in supracristal VSD as compared to infracristal VSD and severity of AR was not related with the location of VSD either supracristal or infracristal. Maximum age at which VSD and AR presented was 45; interestingly the index patient presented much later than this largest Indian series reported so far.
Miller LR et al., described a case of supracristal VSD in a 27-year-old Chinese male with incidental pan systolic murmur who was quite asymptomatic and also, he had no AR [13]. They described there is more likelihood of picking up a supracristal VSD with AR in younger age than in elderly. Seetharam K and Pachulski R reported a case of 18-year-old male with supracristal VSD and severe AR with left ventricular systolic dysfunction which was missed during routine echocardiography but paradoxically picked up during routine cardiac auscultation [14]. Subsequently in the above patient small supracristal VSD was confirmed in cardiac MRI. Kumari V et al., described the presence of AR in 10 patients out of 12 patients with supra cristal VSD across their series of 114 cases of VSD. Median age of presentation of those cases was six months only [15]. Backer CL et al., described incidence of AR in supracristal VSD was 44% and age at the time of presentation was two weeks to 18 years with mean of 5.5 years [16].
Kawashima Y et al., described the median age of presentation of VSD with AR was 13.4 years across 35 patients of 4-25 years [11]. In their study among 35 patients, VSD was closed directly in 14 patients and with a Teflon patch in 21. The aortic valve was repaired in 16 patients, replaced in eight, and no interference was indicated in 11. In cases of supracristal VSD with AR, the involved semilunar cusp undergoes progressive detoriation and the valvular insufficiency progresses [17,18]. Sometimes the prolapsing cusp seals the VSD and those cases present as isolated AR. Interestingly, the index patient did not develop AR which is quite unnatural in the history of supracristal VSDs.
Ajij KU et al., defined supracristal VSD as a space between top of the ventricular septum and anterior aortic root in three of the four patients as noted in the index case [Table/Fig-1] [19]. Paradoxically the present case did not have prolapse of right coronary cusp or aortic dilatation. Smith KA et al., described 29 cases of VSD with AR between the age of 3-38 years [10]. The most common cause of AR was a prolapsed aortic valve cusp, which occurred in 19 patients. In the present case, may be the non-prolapsing weak aortic leaflet may be the cause of AR as prolapse of right coronary cusp or non-coronary cusp was not evident in echocardiography.
Chang CH et al., described direct closure of the defect and pericardial patch closure had similar outcome during repair of VSD with AR and they also described plication of the aortic valve is also a modality of surgical treatment of prolapsed aortic leaflet [20]. The index patient had a small supracristal VSD, in the event of necessity of surgical correction in future as the patient may develop severe AR, direct closure of the VSD may be a plausible option. Piazza F et al., described an interesting case of supracristal VSD with AR in a 15-year-old boy but the AR was due to prolapse of non coronary cusp due to Venturi effect known as Laubry-Pezzi Syndrome [21]. There was no prolapse of non coronary cusp in the present case; may be the weakened right coronary cusp attributed towards development of AR. Egbe A et al., described adults with supracristal VSD are at lower risk for AR progression but higher risk for aneurysm of sinus of Valsalva (aSOV) formation compared to historical pediatric cohorts [22]. Younger age was a predictor of AR progression and surgical intervention had no protective effect on complication rate. Likewise, in the present case there was non significant progression of AR after six months of follow-up with echocardiography. Kumari V et al., described AR was most commonly seen in supracristal VSD (83.3%; n=10) followed by perimembranous VSD (28.9%; n=33) [15]. Hussain AH et al., described the presentation of a 20-year-old boy with supracristal VSD with severe AR with severe reversible pulmonary artery hypertension who underwent emergency surgical direct VSD closure with excision of aortic leaflet followed by replacement [23].
Summarising the natural history, supracristal VSD with AR presents in relatively younger age and mandates surgery. This case is a unique and first description of index presentation of supracristal VSD with AR in 5th decade of life managed conservatively in view of presence of moderate AR without presence of left ventricular significant dilatation (55-75 rule: end systolic diameter >55 and end diastolic diameter >75) or left ventricular systolic dysfunction or pulmonary artery hypertension or progressive aortopathy (ascending aorta >45 mm).
Conclusion(s)
Natural history of congenital heart diseases varies in diversity, sometimes nature retards the progression to bless in disguise. This case was unique and is the first description of such a delayed presentation of a supracristal VSD with moderate AR without prolapse of aortic cusp or dilatation of the aortic sinus in the fifth decade of life. Nature gives, nature protects and heals also.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 25, 2021
Manual Googling: Jul 05, 2021
iThenticate Software: Jul 23, 2021 (14%)
[1]. Laubry C, Pezzi, C, Traite’ des maladies conge’nitales du coeur 1921 ParisBailliere [Google Scholar]
[2]. Deutch V, Blieden LC, Kraus Y, Yahini JH, Neufeld HN, Ventricular septal defect associated with aortic insufficiencyAm J Roentgenol 1969 106(1):32-41.10.2214/ajr.106.1.324238826 [Google Scholar] [CrossRef] [PubMed]
[3]. Tatsuno K, Konno S, Ando M, Sakakibara Pathogenetic mechanisms of prolapsing aortic valve and aortic regurgitation associated with VSDCirculation 1973 48(5):1028-37.10.1161/01.CIR.48.5.10284751947 [Google Scholar] [CrossRef] [PubMed]
[4]. Plauth WH Jr, Braunwald E, Rockoff SD, Mason DT, Morrow AG, Ventricular septal defect and aortic regurgitation; clinical, hemodynamic. and surgical considerationsAm J Med 1965 39(4):552-67.10.1016/0002-9343(65)90079-3 [Google Scholar] [CrossRef]
[5]. Van Praagh R, McNamara JJ, Anatomic types of ventricular septal defect with aortic insufficiency. Diagnostic and surgical considerationsAm Heart J 1968 75(5):604-19.10.1016/0002-8703(68)90321-9 [Google Scholar] [CrossRef]
[6]. Sakakibara S, Konno S, Congenital aneurysm of the sinus of Valsalva associated with ventricular septal defect. Anatomical aspectsAm Heart J 1968 75(5):595-603.10.1016/0002-8703(68)90320-7 [Google Scholar] [CrossRef]
[7]. Van Praagh R, What is the Taussig-Bing malformationCirculation 1968 38(3):445-49.10.1161/01.CIR.38.3.4455673595 [Google Scholar] [CrossRef] [PubMed]
[8]. Roberts WC, Morrow AG, Braunwald E, Complete interruption of the aortic archCirculation 1962 26(1):39-59.10.1161/01.CIR.26.1.3914492799 [Google Scholar] [CrossRef] [PubMed]
[9]. Kozuka T, Nosaki T, Sato K, Ventricular septal defect in tetralogy of FallotAm J Roentgenol 1970 110(3):497-503.10.2214/ajr.110.3.4975489687 [Google Scholar] [CrossRef] [PubMed]
[10]. Smith KA, Olsen EGJ, Oakley CM, Goodwin JF, Cleland WP, Ventricular septal defect and aortic regurgitationThorax 1969 24(3):257-75.10.1136/thx.24.3.2575810367 [Google Scholar] [CrossRef] [PubMed]
[11]. Kawashima Y, Danno M, Shimizu Y, Matsuda H, Miyamoto T, Fujita T, Ventricular septal defect associated with aortic insufficiency anatomic classification and method of operationCirculation 1973 47(5):1057-64.10.1161/01.CIR.47.5.10574705572 [Google Scholar] [CrossRef] [PubMed]
[12]. Somnath HS, Gupta SK, Reddy KN, Murthy JS, Rao AS, Abraham KA, Ventricular septal defect with aortic regurgitation: A hemodynamic and angiographic profile in Indian subjectsIndian Heart J 1990 42(2):113-16. [Google Scholar]
[13]. Miller LR, Nemeth M, Flamm SD, Sung C, Stainback RF, Supracristal ventricular septal defectTexas Heart J 2006 33(1):96-97. [Google Scholar]
[14]. Seetharam K, Pachulski R, Case of supracristal ventricular septal defect and aortic regurgitation detected by cardiac auscultation but missed by diagnostic imagingCureus 2021 13(2):e1350210.7759/cureus.1350233786211 [Google Scholar] [CrossRef] [PubMed]
[15]. Kumari V, Shaikh AS, Zakai SB, Incidence of aortic regurgitation in association with type of ventricular septal defects and its immediate and intermediate outcome after surgical closureCureus 2018 11(7):e510210.7759/cureus.5102 [Google Scholar] [CrossRef]
[16]. Backer CL, Idriss FS, Zales VR, IIbawi MN, De Leon SY, Muster AJ, Mavroudis Surgical management of conal ventricular septal defectJ Thoracic Cardiovasc Surg 1991 102:288-96.10.1016/S0022-5223(19)36562-6 [Google Scholar] [CrossRef]
[17]. Rhodes LA, Keane JF, Keane JP, Fellows KE, Jonas RA, Castaneda AR, Long follow-up (to 43 years) of ventricular septal defect with audible aortic regurgitationAm J Cardiol 1990 66:340-45.10.1016/0002-9149(90)90846-S [Google Scholar] [CrossRef]
[18]. Leung MP, Beerman LB, Siewers RD, Bahnson HT, Zuberbuhler AR, Long term follow-up after aortic valvuloplasty and defect closure in ventricular defect and aortic regurgitationAm J Cardiol 1987 60:890-94.10.1016/0002-9149(87)91042-3 [Google Scholar] [CrossRef]
[19]. Ajij KU, Cole RB, Paul M, Echocardiographic features of supracristal ventricular septal defect with prolapsed aortic leafletAmerican Journal of Cardiology 1979 43(4):854-59.10.1016/0002-9149(79)90089-4 [Google Scholar] [CrossRef]
[20]. Chang CH, Lee MC, Shieh M, Surgical treatment of supracristal type of VSScandinavian Journal of Thoracic and Cardiovascular Surgery 1988 22(3):22110.3109/140174388091060663227324 [Google Scholar] [CrossRef] [PubMed]
[21]. Piazza F, Santoro G, Russo MG, Aortic insufficiency due to ventricular septal defect (Laubry-Pezzi syndrome)Journal of Cardiovascular Medicine 2013 14(2):164-65.10.2459/JCM.0b013e3283515c3022609868 [Google Scholar] [CrossRef] [PubMed]
[22]. Egbe A, Poterucha Joseph T, Dearani Joseph A, Warnes Carole A, Supracristal ventricular septal defect in adults; Is it time for a paradigm shiftInternational Journal of Cardiology 2015 198:09-14.10.1016/j.ijcard.2015.06.10026149330 [Google Scholar] [CrossRef] [PubMed]
[23]. Hussain AH, Hanif B, Khan G, Hasan K, Supracristal ventricular septal defect with severe right coronary cusp prolapseJournal of Pakistan Medical Association 2011 61(6):605-06. [Google Scholar]