Case Report
A 49-year-old female patient reported to the Department of Oral Medicine and Radiology with the chief complaint of burning sensation on inner aspect of right cheek for one year. The family history, medical history, deleterious habit history and general examination of the patient were non contributory.
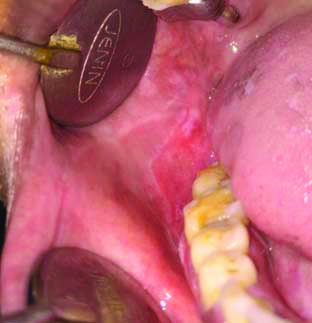
On inspection, a diffuse whitish area surrounded by erythematous area was seen in the right buccal mucosa with relation to 46. The overlying surface appeared smooth with lace-like pattern of white striations [Table/Fig-1]. On palpation, the lesion was non tender and non scrapable. The provisional diagnosis was Oral Lichen Planus (OLP). Patient had no other systemic diseases or any extraoral lesions.
Intraoral photograph showing oral lichen planus.
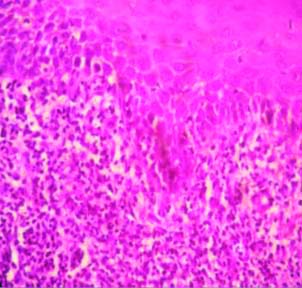
Incisional punch biopsy was done and the microscopic examination revealed presence of parakeratotic stratified squamous surface epithelium with atrophic changes. Rete ridges were saw-tooth shaped and there was dense band of chronic inflammatory cells in the juxtaepithetial connective tissue which was suggestive of erosive Lichen Planus (LP) [Table/Fig-2].
Photomicrograph (40 X, H&E stained) showing acanthosis with saw-tooth rete ridges and band like chronic inflammatory cells in the connective tissue.
Tracrolimus 0.1% ointment (along with topical anaesthetic, antiseptic and analgesic gel) was prescribed and she was recalled after two weeks, but she did not turn up. The patient came back after 10 months with the complaint of pain and swelling in the same region. She informed that she could not come for check-up due to the national lockdown because of the Coronavirus Disease 2019 (COVID-19) pandemic. She discontinued the medication given to her after continuing for two weeks without any consultation.
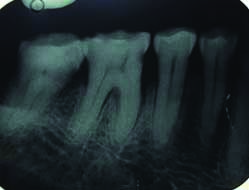
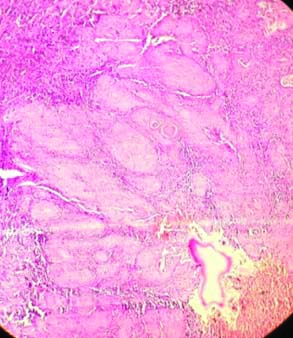
On intraoral examination, a diffuse swelling was seen involving the buccal vestibule in relation with 46, 47, size approximately 3×1.5 cm, extending upto the retromolar region and the overlying mucosa was fragile and reddish in colour. The lesion was tender on palpation and had an indurated margin [Table/Fig-3]. Intraoral periapical radiograph showed widening of the periodontal ligament space with discontinuation of lamina dura [Table/Fig-4]. Considering the history, clinical features and the fact that erosive LP has a high chance of malignant transformation the patient was advised for another biopsy. The histopathology findings revealed connective tissue stroma composed of dense collagen bundles, numerous epithelial cell island scattered within the matrix, epitheloid cells were pleomorphic with hyperchromatic nuclei, abnormal mitotic figures, nuclear pleomorphism, and presence of keratin pearls. The features were suggestive of moderately differentiated squamous cell carcinoma (T2N0MX) involving right gingivobuccal sulcus [Table/Fig-5].
Intraoral photograph showing non healing exophytic growth in the lower buccal vestibule of right side.

Intraoral periapical radiograph showing widening of the periodontal ligament space with discontinuation of lamina dura.
Photomicrograph (10X, H&E stained) showing invasion of proliferating neoplastic epithelial islands within the connective tissue stroma.
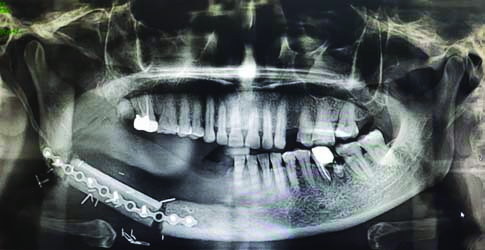
The patient was referred to Oral Surgery Department for further treatment. Segmental mandibulectomy was done with placement of free fibula graft with the help of continuous titanium plate. Patient came for follow-up after one month and showed satisfactory healing [Table/Fig-6,7].
Intraoral photograph showing postoperative site after partial mandibulectomy done.

Postoperative Orthopantomogram (OPG) showing free fibula graft was placed.
Discussion
The Lichen Planus (LP) is an autoimmune mucocutaneous inflammatory disorder which affects either skin and/or mucous membranes and associated with a broad spectrum of clinical manifestations. It is mediated by an antigen-specific mechanism which helps in activation of cytotoxic T-cells, mast cell degranulation and Matrix Metalloproteinase (MMP) activation. OLP affects from 0.5% to 2% of the population and has a predilection for middle age and female gender [1].
Although the exact aetiology is still unknown, there are some associated factors such as; genetic (HLA-A3, A11, A26), dental materials (silver amalgam, gold), drugs {Non steroidal Anti-Inflammatory Drugs (NSAIDs), beta blockers), bacteria (Helicobactor pylori), virus (Human Herpes Virus-6 (HHV-6), Epstein-Barr Virus (EBV), Human Papilloma Virus (HPV), Hepatitis C Virus (HCV), stress, bowel’s disease (coeliac disease, ulcerative colitis and crohn’s disease), candida infections etc., [2]. The malignant transformation rate of OLP is 1.37% with an annual TR of 0.20% [1].
Oral Lichen Planus (OLP) is an autoimmune inflammatory disease where auto-cytotoxic CD8 + T-cells trigger apoptosis of the basal cells of the oral epithelium through Tumour Necrosis Factor (TNF)-α, Fas-Fas L-mediated or granzyme B-activated apoptosis [3,4]. In OLP, the expression of the Vascular Adhesion Molecules (VAM), such as Cluster of Differentiation (CD) 62E, CD54, CD106 etc., are increased by the sub-epithelial endothelial cells. Some of the cytokines that are responsible for upregulation of the VAM are: TNF-α, IFN-γ and IL-1. In T cells the Matrix Metallopeptidase-9 (MMP-9) is upregulated which can degrade the tissue matrix protein (collagen 4) and causes the basement membrane disruption in OLP [5].
The clinical presentation of OLP is white or grey-coloured thread-like papules in a linear, annular or retiform arrangement forming typical lacy, reticular patches, rings and streakes. The tiny white elevated dot seen at the intersection of white lines is known as Whickham’s striae. The lesions are usually asymptomatic, bilaterally/symmetrically anywhere in the oral cavity, but most common on buccal mucosa, tongue, lips, gingiva, floor of mouth, palate and may appear weeks or months before the appearance of cutaneous lesions. Erosive OLP is the most significant form of the disease because it shows symptomatic lesions [2].
The 1st case of transformation of an OLP case into Oral Squamous Cell Carcinomas (OSCCs) was reported in 1910 by Hallopeau H [6]. Arreaza A et al., explained how p53 plays an important role in malignant transformation of OLP. The p53 is an oncoprotein involved in the suppression of the proliferation of Deoxyribonucleic Acid (DNA) damaged cells via cell cycle regulation that results in the apoptosis of these cells. Impaired function of the p53 gene has been implicated in the development and progression of oral epithelial dysplasia and OSCC [7]. Tlsty TD and Coussens LM explained how inflammation increases the oxidative stress by the release of free radicals, growth factors and mediators of inflammation that promote cell survival seem to predispose the onset and stabilisation of mutations which can cause neoplastic transformation [8].
The possible high risk factors for malignant transformation from OLP includes, tobacco (smoking or chewing), alcohol, virus infection (Human papillomavirus, Epstein-Barr virus, hepatitis B virus, Human immunodeficiency virus, herpes simplex virus), bacterial infection (Treponema pallidum), fungal infection (Candidiasis), electro-galvanic reaction between unlike restorative metals, ultraviolet radiation from sunlight, genetic (5%), immunosuppressive drugs, malnutrition (iron, vitamin A, B, C deficiency) etc., [9]. In the present case, the probable factors associated with the patient could be fungal infection, vitamin deficiency or genetic causes. Giuliani M et al., reported that female gender, red clinical (erosive) form, and tongue had slightly more transformation risk (1.37%) of OLP into OSCC [1]. Tampa M et al., (2018) reported that numerous biomarkers expressed in OLP, including modulators of apoptosis (p53, MCL-1), cell cycle regulators (BMI1, p16), MMPs, and inflammation-related factors (TNF-α, IL-6, and COX-2) proves that there is a chance of malignant transformation into OSCC [6].
Ganesh D et al., reported that the chances of malignant transformation from OLP can be reduced by reducing the amount of inflammation by removing the aetiological cause like sharp cuspal edges of teeth, smoking and tobacco chewing habit, unnecessary exposure to radiation and uncontrolled used of steroids [10].
The risk of the malignant transformation of OLP is higher in women than in men, in the age group of 60–70 years [11]. Regarding the clinical type and site of OLP, Aghbari SMH et al., reported that the rates of malignant transformation were 1.7%, 1.3%, and 0.1% in erosive, atrophic, and reticular patterns, respectively [12]. There are case reports and studies in literature [13-15] about the malignant transformation of OLP which occurred within or more than 4 to 7 years; but in the index case the malignant transformation occurred just within an interval of one year.
The index patient did not have any co-morbidity or deleterious habit history. Due to the unfortunate COVID-19 pandemic, the patient could not come for follow-up for a long period while also discontinuing the medication. As a result, the untreated erosive LP, which has a potential of malignant transformation, progressed into moderately differentiated squamous Cell Carcinoma (SCC).
The relevance of the present case report was that, potentially malignant disorders of the oral cavity need regular follow-up and failure to do so may result in malignant transformation in certain cases.
Conclusion(s)
As a dentist, it is our prime duty to diagnose and follow-up lesions which can have a malignant transformation and to also increase the awareness among general public about such lesions. The highest risk of malignant transformation is seen in erosive form of OLP. That’s why patients with OLP are advised to avoid additional risk factors such as tobacco and alcohol and followed at minimum an year interval as prognosis and patient survival is directly related to stage and grade of cancer at its initial diagnosis.
[1]. Giuliani M, Troiano G, Cordaro M, Corsalini M, Gioco G, Muzio LL, Rate of malignant transformation of oral lichen planus: A systematic reviewOral Dis 2019 25(3):693-709.10.1111/odi.1288529738106 [Google Scholar] [CrossRef] [PubMed]
[2]. Gupta S, Jawanda MK, Oral Lichen Planus: an update on etiology, pathogenesis, clinical presentation, diagnosis and managementIndian J Dermatol 2015 60(3):222-29.10.4103/0019-5154.1563152612014611896819 [Google Scholar] [CrossRef] [PubMed] [PubMed]
[3]. Zhou XJ, Sugarman PB, Savage NW, Walsh LJ, Seymour GJ, Intra-epithelial CD8+T cells andbasement membrane disruption in oral lichen planusJ Oral Pathol Med 2002 31:23-27. [Google Scholar]
[4]. Sugerman PB, Satterwhite K, Bigby M, Autocytotoxic T-cell clones in lichen planusBr J Dermatol 2000 142:449-56.10.1046/j.1365-2133.2000.03355.x10735949 [Google Scholar] [CrossRef] [PubMed]
[5]. Abbate G, Neoplastic transformation of oral lichen: Case report and review of the literatureActa Otorhinolaryngol Ital 2006 26:47-52. [Google Scholar]
[6]. Tampa M, Caruntu C, Mitran M, Mitran C, Sarbu I, Rusu LC, Markers of oral lichen planus malignant transformationDisease Markers 2018 2018:195950610.1155/2018/195950629682099 [Google Scholar] [CrossRef] [PubMed]
[7]. Arreaza A, Rivera H, Correnti M, p53 expression in oral lichenoid lesions and oral lichen planusGen Dent 2015 63(1):69-72. [Google Scholar]
[8]. Tlsty TD, Coussens LM, Tumour stroma and regulation of cancer developmentAnnu Rev Pathol 2006 1(1):119-50.10.1146/annurev.pathol.1.110304.10022418039110 [Google Scholar] [CrossRef] [PubMed]
[9]. Grover MC, Malik NS, Kumar A, More VP, Bhambar RS, Potentially malignant disorders- an updateJ Adv Med Dent Scie Res 2014 2(3):56-61. [Google Scholar]
[10]. Ganesh D, Sreenivasan P, Ohman J, Wallstrom M, Braz-silva PH, Giglio D, Potentially malignant oral disorders and cancer transformationAnticancer Research 2018 38:3223-29.10.21873/anticanres.1258729848669 [Google Scholar] [CrossRef] [PubMed]
[11]. Gonzalez-Moles MA, Scully C, Gil-Montoya JA, Oral lichen planus: Controversies surrounding malignant transformationOral Dis 2008 14(3):229-43.10.1111/j.1601-0825.2008.01441.x18298420 [Google Scholar] [CrossRef] [PubMed]
[12]. Aghbari SMH, Abushouk AI, Attia A, Malignant transformation of oral lichen planus and oral lichenoid lesions: A meta-analysis of 20095 patient dataOral Oncol 2017 68:92-102.10.1016/j.oraloncology.2017.03.01228438300 [Google Scholar] [CrossRef] [PubMed]
[13]. Soo J, Kokosis G, Ogilvie M, Jiang X, Powers DB, Rocke DJ, A rare case of malignant transformation of oral lichen planus of the mandiblePlastic and Reconstructive Surgery- Global Open 2016 4(12):e107010.1097/GOX.000000000000107028293492 [Google Scholar] [CrossRef] [PubMed]
[14]. Fitzpatrick SG, Hirsch SA, Gordon SC, The malignant transformation of oral lichen planus and oral lichenoid lesions: A systematic reviewJ Am Dent Assoc 2014 145(1):45-56.10.14219/jada.2013.1024379329 [Google Scholar] [CrossRef] [PubMed]
[15]. Gándara-Rey JM, Diniz Freitas M, Gándara Vila P, Blanco Carrión A, Suárez Peñaranda JM, Garcia Garcia A, Malignant transformation of oral lichen planus in lingual location: report of a caseOral Oncology Extra 2004 40(1):01-04.10.1016/S1741-9409(03)00002-5 [Google Scholar] [CrossRef]