Traditionally, a midline laparotomy wound is closed in layers co-opting the various layers separately; however, various other methods of closure have come into vogue in the recent years. One such is the single layer mass closure technique, in which all the layers of the abdominal wall are closed in single layer, except for the skin and subcutaneous tissues, which are closed in separate layers [1]. Yet another method, the retention closure technique incorporating all layers including skin and subcutaneous tissue closed in a single layer has become more popular for giving additional strength to the wound closure [2]. These methods are still current to minimise the wound complications following laparotomy especially in an emergency setting. They are usually employed in elective procedures although some reports state that the method of closure does not generally affect the outcome of surgery in elective situations owing to good nutritional status, adequate preparation of the patient for surgery and absence of associated risk factors [3]. Postoperative both early and late wound complication rates were lesser in the retention closure technique compared to the layered closure technique [4].
This study was conducted to determine which method of closure was superior in emergency laparotomies and to assess the various risk factors associated with poor wound healing. The incidence of early wound complications in elective and emergency midline laparotomy like infection and fascial dehiscence was compared between the layered closure and the retention closure techniques. The risk factors for wound dehiscence and burst abdomen in both techniques were documented.
Materials and Methods
This was a longitudinal cohort study conducted over a period of 12 months from January 2014 to January 2015. All the subjects fulfilling the inclusion and exclusion criteria attending the general surgery department in Mahatma Gandhi Medical College and Research Institute, Puducherry, India, were considered after obtaining Ethical Clearance (PG/2014/27). Those who underwent laparotomy were explained about the details of the study in their own language and informed consent was obtained. A total of 57 subjects were enrolled. The choice of closure of the laparotomy was left to the preference of the operating surgeon.
Inclusion criteria: All patients between 18 and 75 years undergoing elective or emergency midline laparotomy (upper or lower) were included.
Exclusion criteria: The patients with re-laparotomies and patients with co-morbid conditions such as an immunocompromised status and patients on chemotherapy or steroid treatment were excluded.
All patients underwent treatment as per department standard protocol. Initial assessment included complete history, general physical and systemic examination. All routine blood investigations such as complete blood count, blood urea, serum creatinine, serum electrolytes, blood sugar, liver function test, X-ray Chest and abdomen, ultrasonography/ Contrast Enhanced Computed Tomography (CECT) abdomen were done, if required.
Group A (Layered closure)
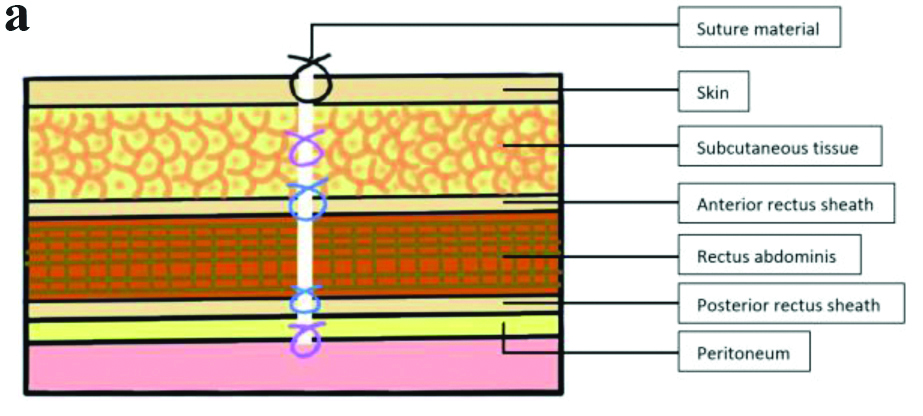
Peritoneum was closed by monofilament 2-0 polyglactin or left open, rectus sheath with monofilament 1-polypropylene; subcutaneous tissue was closed using monofilament 2-0 polyglactin, and skin was closed using monofilament 3-0 nylon in a sterile manner and dressing were applied [Table/Fig-1a].
Layered closure technique.
Group B (Retention closure)
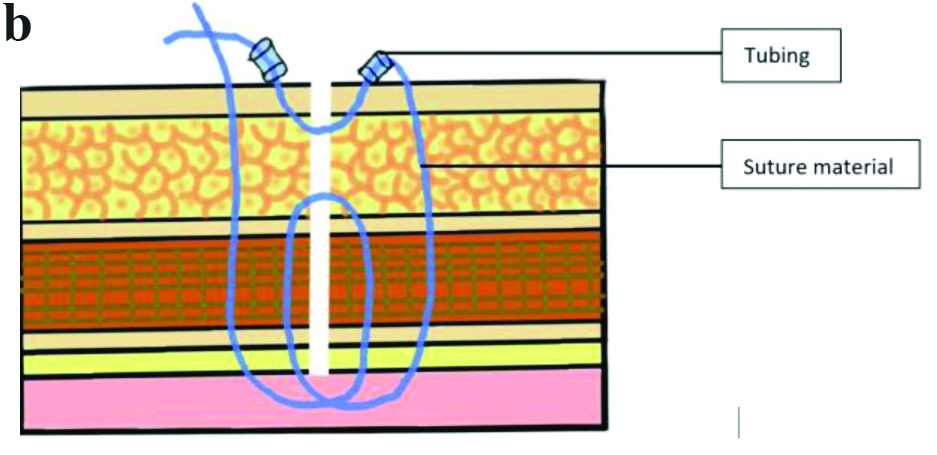
Peritoneum, posterior rectus sheath, rectus muscle, anterior rectus sheath, subcutaneous tissue and skin were closed in a single layer retention closure using monofilament 1 polypropylene; to provide cutting through of the sutures, the sutures were tied by threading them through small pieces of intravenous (i.v.) tubing cut to proper required size, each sutures were placed 1 inch apart with proper skin approximation as shown in [Table/Fig-1b].
Retention closure technique.
The outcomes of interest included documentation of wound healing (primary or secondary intention) in both groups, incidence of surgical site infection in groups, incidence of wound dehiscence and its depth (partial or complete) and postoperative pain scores at various intervals.
The following observations were made on the patients during the postoperative period:
Pain score: using the visual analogue scale [5] on day1, 2, 3, 7 and 10.
Surgical site infection: was diagnosed as per standard Healthcare Infection Control Practices Advisory Committee (HICPAC) criteria [6]. Pus culture and sensitivity test was sent if pus discharge was found in the postoperative period.
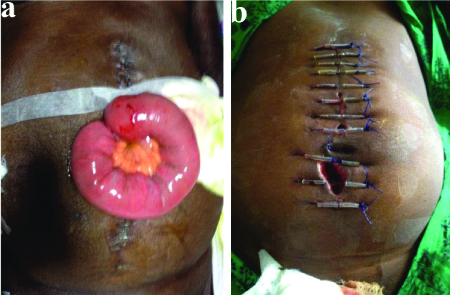
Fascial dehiscence/burst abdomen diagnosed by the operating surgeon [Table/Fig-2a,b].
a) Complete dehiscence in layered closure; b) Partial dehiscence in retention closure.
In the layered closure technique suture removal was done on postoperative day 10. In Retention closure technique suture removal was done on postoperative day 14.
Statistical Analysis
Statistical analysis was carried out using Statistical Package for the Social Sciences (SPSS) version 19.0 (IBM SPSS, US) software with regression modules installed. Chi-square test and t-test were used to analyse the data.
Results
A total of 57 patients underwent laparotomy. Layered closure was done in 30 patients and retention closure in 27 patients. Elective cases were more in number in the layered closure technique, out of 30 patients 21 (70%) were elective procedure and 9 (30%) were emergency procedure. In retention closure emergency cases were more in number, out of 27 patients 17 (63%) were emergency procedure and 10 (37%) were elective procedure.
On comparing pain scores in both groups on day 1, day 2, day 3, day 7 and day 10, the mean value of pain score was slightly higher in the retention closure technique but reached significance only on days 2 and 10 [Table/Fig-3].
Pain score in the postoperative period.
| Postoperative days | Layered closure Mean±SD | Retention closure Mean±SD | p-value |
|---|
| Day 1 | 3.40+1.19 | 3.63+1.36 | 0.50 |
| Day 2 | 3.00+1.14 | 3.56+1.01 | 0.05 |
| Day 3 | 2.60+0.93 | 2.59+0.93 | 0.976 |
| Day 7 | 2.00+0.74 | 2.37+1.10 | 0.151 |
| Day 10 | 1.20+0.10 | 1.85+0.77 | 0.008 |
t-test was used to analyse the data; p-value <0.05 is considered to be statistically significant
[Table/Fig-4] shows wound dehiscence rates in the two procedures. Overall, in the layered closure group there were three dehiscences, one partial and two complete and in the retention closure group there were again three dehiscences, all of them partial. There was no statistical difference between the two groups in dehiscence rates.
Wound dehiscence rates in the two groups.
| Closure status | Wound dehiscence rates | p-value |
|---|
| Layered closure | Retention closure | Total |
|---|
| No dehiscence | 27 | 24 | 51 | 0.89 |
| Partial dehiscence | 1 | 3 | 4 | 0.249 |
| Complete dehiscence | 2 | 0 | 2 | 0.17 |
Chi-square test was used to analyse the data; p-value <0.05 is considered to be statistically significant
[Table/Fig-5] shows wound healing rates in two closure techniques. Overall, in the layered closure group, wound healing occurred by primary intention in 27 patients and secondary intention in three patients. In the Retention closure group, wound healing occurred by primary intention in 24 patients and secondary intention in three patients. There was no statistical difference between the two groups (p-value=0.89).
Wound healing in the two groups.
| Closure status | Wound healing | p-value |
|---|
| Primary intention | Secondary intention | Total |
|---|
| Layered closure | 27 (90%) | 3 (10%) | 30 (100%) | 0.89 |
| Retention closure | 24 (89%) | 3 (11%) | 27 (100%) |
Chi-square test was used to analyse the data; p-value <0.05 is considered to be statistically significant
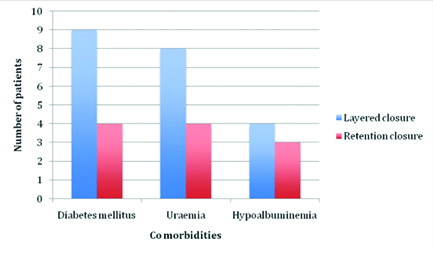
[Table/Fig-6] shows the distribution of co-morbidities in both the groups. Diabetes mellitus was present in nine patients in the layered closure group and 4 patients in retention closure group. Uraemia was present in eight patients in layered closure group and four patients in retention closure group. Hypoalbuminemia was present in four patients in layered closure group and three patients in retention closure group.
Co-morbidities in the two groups.
[Table/Fig-7] shows wound infection rates and its association with uraemia, hypoalbuminemia and diabetes mellitus in the two groups. Overall, 17 patients developed wound infection, out of which 12 patients had wound infection in the layered closure group and five patients in the retention closure group. This difference was not significant (p-value=0.077). The incidence of infection was significantly higher in patients with uraemia (p-value=0.002) and in those with hypoalbuminemia (p-value=0.01).
Wound infection and its association with uraemia, diabetes mellitus, and hypoalbuminemia.
| Closure | Wound infection | Total | p-value |
|---|
| Present (n=17) | Absent (n=40) |
|---|
| Layered Closure (LC) | 12 (40%) | 18 (60%) | 30 (100%) | 0.077 |
| Retention Closure (RC) | 5 (18.5%) | 22 (81.5%) | 27 (100%) |
| Total | 17 (29.8%) | 40 (70.2) | 57 (100%) |
| Uraemia |
| Present | 8 (66.7%)(LC: 6) (RC: 2) | 4 (33.3%)(LC: 2) (RC: 2) | 12 (100%) | 0.002 |
| Absent | 9 (20.0%)(LC: 6) (RC: 3) | 36 (80.0%)(LC: 16) (RC: 20) | 45 (100%) |
| Total | 17 (29.8%) | 40 (70.2%) | 57 (100%) |
| Hypoalbuminemia |
| Present | 5 (71.4%)(LC: 3) (RC: 2) | 2 (28.6%)(LC: 1) (RC: 1) | 7 (100%) | 0.01 |
| Absent | 12 (24.0%)(LC: 9) (RC: 3) | 38 (76%)(LC: 17) (RC: 21) | 50 (100%) |
| Total | 17 (29.8%) | 40 (70.2%) | 57 (100%) |
| Diabetes mellitus |
| Present | 6 (42.2%)(LC: 5) (RC: 1) | 7 (53.8%)(LC: 4) (RC: 3) | 13 (100%) | 0.143 |
| Absent | 11 (25.0%)(LC: 7) (RC: 4) | 33 (35.0%)(LC: 14) (RC: 18) | 44 (100%) |
| Total | 17 (29.8%) | 40 (70.2%) | 57 (100%) |
Chi-square test was used to analyse the data; p-value <0.05 is considered to be statistically significant
Pus discharge was found in 10 patients, most of the culture and sensitivity reports were sterile. Only in three patients organisms were isolated, which was Escherichia coli in two patients and Pseudomonas aeruginosa in one patient. Appropriate antibiotics were escalated depending on the sensitivity report.
[Table/Fig-8] shows the wound dehiscence rates in the two groups and its association with co morbid conditions. Although co-morbidity significantly increased the risk of dehiscence, no difference could be demonstrated between the two methods of closure in partial dehiscence (p-value=0.249) and complete dehiscence (p-value=0.17), as regards the effects of coexisting morbidity. Presence of diabetes mellitus, uraemia and hypoalbuminemia significantly increased the risk of wound dehiscence (p-value=0.029) (p-value=0.006) (p-value=0.001), respectively.
Wound dehiscence and its association with diabetes mellitus, uraemia and hypoalbuminemia.
| Morbidity status | Wound dehiscence (n=6) | Total | p-value |
|---|
| Absent | Partial | Complete |
|---|
| Diabetic status |
| Diabetic | 10 (76.9%) | 1 (7.7%) (LC) | 2 (15.4%)(LC) | 13 (100%) | 0.029 |
| Non diabetic | 41 (93.2%) | 3 (6.8%) (RC) | 0 | 44 (100%) |
| Total | 51 (89.5%) | 4 (7.0%) | 2 (3.5%) | 57 (100%) |
| Uraemic status |
| Present | 8 (66.7%) | 2 (16.7%)(LC: 1) (RC: 1) | 2 (16.7%)(LC) | 12 (100%) | 0.006 |
| Absent | 43 (95.6%) | 2 (4.4%) (RC) | 0 | 45 (100%) |
| Total | 51 (89.5%) | 4 (7.0%) | 2 (3.5%) | 57 (100%) |
| Hypoalbuminemia |
| Present | 1 (14.3%) | 4 (57.1%)(LC: 1) (RC: 3) | 2 (28.6%)(LC) | 7 (100%) | 0.001 |
| Absent | 50 (100%) | 0 | 0 | 50 (100%) |
| Total | 51 (89.5%) | 4 (7.0%) | 2 (3.5%) | 57 (100%) |
Chi-square test was used to analyse the data; LC: Layered closure; RC: Retention closure; p-value <0.05 is considered to be statistically significant
Discussion
Midline incision is the most preferred method in all laparotomies from historical times, owing to easy access and being less time consuming [7]. Postoperative wound failure tends be a major complication following laparotomy despite advances in surgical technique, antibiotic coverage, suture material.
Wound failure usually occurs due to several risk factors including, patients associated co-morbid conditions like Diabetes Mellitus, malnutrition, anaemia, uraemia, postoperative sudden increase in intra-abdominal pressure due to vomiting, coughing and sneezing etc., [8]. For these reasons various methods of closure have been preferred by surgeons depending on their experience and intra-abdominal contamination during the time of surgery.
The incidence of wound disruption following laparotomy was reported as 1-3%, and amounts to nearly 50% of all major postoperative complications [1]. A pinkish discharge from the laparotomy wound or sensation of something giving way in the abdomen noticed by the patients are indicators for burst abdomen [9].
To overcome wound complications, various types of closure and associated complication rates have been reported by several authors. In 1995, Sivam NS et al., had studied a comparison of the Smead-Jones closure and Layered closure in a group of 403 patients and had reported that wound dehiscence rate was less (3.0%) in Smead-Jones closure compared to layered closure. They concluded that, both early and late wound complication rates were lesser in Smead jones technique compared to the layered closure technique [4].
Murtaza B et al., in 2008, studied modified abdominal wound closure in 36 patients and had reported wound infection rate of 33.33% and wound dehiscence rate of 2.77%. They concluded that the modified technique (Retention closure) used in managing the patients with generalised peritonitis and metastatic abdominal tumours (complicated/high risk laparotomies) was associated with a lower incidence of serious complications like wound dehiscence and incisional hernia formation compared to other recommended techniques [3]. Another study done by Khorgami Z et al., in 2013, concluded that prophylactic retention sutures reduced the risk of wound dehiscence following midline laparotomy in high risk patients with multiple risk factors which were likely to affect wound healing [10].
Similarly, Mohanad A in 2014 had reported comparing mass closure and retention closure in 150 patients. The wound infection rate was 15.8% and 13.8% and the wound dehiscence rate was 13.5% and 4.1% respectively between the two procedures. They concluded that prophylactic retention sutures can decrease the incidence of abdominal wound dehiscence. However, although there was a decrease incidence of postoperative evisceration, wound infection and postoperative pain, this did not reach statistical significance [11].
Bande A et al., in 2018, studied comparing single layer closure and layered closure in 97 patients. The wound infection rate was 17.18% and 42.42% and burst abdomen rate was 1.5% and 3.03%, respectively between the two procedures. They concluded that single layer closure was less time consuming with fewer postoperative complications and superior to layered closure technique [12].
All these studies [3,4,10-12] were in accordance with the results and inference obtained in present study. In present study, we compared layered closure and Retention closure in both elective and emergency cases. The incidence of wound infection was high among Layered closure technique. Out of 30 patients, 12 (40%) developed wound infection. On the other hand, in the retention closure technique, out of 27 patients only five patients (18.5%) developed wound infection, even though emergency cases were more among Retention closure technique. This difference observed clinically was, however, not statistically significant (p=0.07). In a similar study done by Bhavikatti G et al., in 2019, comparing Mass closure and Layered closure. The wound infection rate was 13.33% and 36.66% and burst abdomen rate was 23.33% and 3.33%, respectively between the two groups [13].
On comparing wound dehiscence in both the groups, in the Layered closure technique, out of 30 patients three patients developed wound dehiscence, 1 (3.3%) had partial dehiscence and 2 (6.6%) had complete dehiscence. In Retention closure 3 (11%) patients developed partial dehiscence and none developed complete dehiscence. The three patients with partial dehiscence were emergency procedures with extensive peritoneal contamination. Hypoalbuminemia and Uraemia in these three patients could have contributed to the dehiscence. Recent study done by Nitin KB et al., in 2020, had found that wound dehiscence rate was 13.3% in conventional layered closure technique and 2.2% in modified Smead jones technique. The study concluded modified Smead jones technique had lower incidence of wound dehiscence when compared to conventional closure technique [14].
We found a significant association between wound discharge and dehiscence when related to compromised renal function. Uraemic patients (urea >40 mg/dL and creatinine >2 mg/dL) were more likely to develop wound discharge and dehiscence. In a similar study done by Ramneesh G et al., 38% of Uraemic patients developed wound dehiscence [15].
We also found there was significant association between Hypoalbuminemia (serum albumin <3.0 gm) and wound discharge with dehiscence. The study by Ramneesh G et al., had similar findings [15]. Hypoalbuminemia delays wound healing by prolonging the inflammatory phase and impairing proliferation and fibroplasia, collagen synthesis, neoangiogenesis and wound remodelling [15].
Limitation(s)
The limitations of the study included a small sample size, non randomisation and lack of long term follow-up to ascertain the rates of incisional hernias.
Conclusion(s)
Retention closure has advantages over layered closure in preventing wound infections and burst abdomen. Various risk factors are associated with postoperative wound complications, among which hypoalbuminemia and uraemia were significant.
t-test was used to analyse the data; p-value <0.05 is considered to be statistically significant
Chi-square test was used to analyse the data; p-value <0.05 is considered to be statistically significant
Chi-square test was used to analyse the data; p-value <0.05 is considered to be statistically significant
Chi-square test was used to analyse the data; p-value <0.05 is considered to be statistically significant
Chi-square test was used to analyse the data; LC: Layered closure; RC: Retention closure; p-value <0.05 is considered to be statistically significant