As face is the index of the mind, so is nail the index to health. Nail is one of the epidermal derivatives that produce the hardest epithelial structure known in mammalian biology. Nails not only provide aesthetic beauty to hand and feet but also aid in providing protection, tactile sensation and social communication. During the 5th century, Hippocrates described clubbing as a significant sign to the myriad of systemic manifestations [1]. Since then many nail findings have been identified in association with various diseases. Henceforth, nail examination should be an essential component of a complete dermatological examination. Furthermore at times, various nail abnormalities can be a presenting feature before other signs of the disease become apparent.
The increasing aesthetic concern among general public has made even the mildest nail alteration as an important issue for the patient. Abnormal nails are of paramount clinical importance, particularly when they are an exclusive feature devoid of other obvious symptom of a disease. Nail disorders comprise of 10% of all dermatological disorders, the main contributor being papulosquamous disorder [2]. Many studies have been done regarding nail changes in specific papulosquamous disorders especially psoriasis [3-6]. Nail disease was found to be frequent in psoriasis [4] and associated with greater severity of psoriasis and larger number of co-morbidities [3,5].
Nail psoriasis causing considerable cosmetic handicap, provokes both physical and psychological handicap in 93% of patients, restrain daily activities in 60% patients and 52% patients experience pain [5]. Pitting was found to be the most common manifestation [5] especially in finger nails [6]. A strong association was seen between nail changes and joint pain in psoriasis [6]. Only few studies have been done on nail changes in overall papulosquamous disorders. In one such study, it was noted that psoriasis and lichen planus had more nail involvement [7]. Nail Pitting, onycholysis and subungual hyperkeratosis were the most frequent nail changes found in papulosquamous disorders [8].
Hence, this study aimed to observe the spectrum of nail patterns in various papulosquamous disorders. Such studies will help to improve the knowledge about nail disorders in papulosquamous disorders and eventually help in their early diagnosis and effective management.
Materials and Methods
This observational descriptive cross-sectional study was conducted in a tertiary care set up at Government Coimbatore Medical College, Coimbatore from June 2016 to June 2017. Clearance from the Institutional Ethical Committee was obtained (Ethics Committee letter issued by Coimbatore Medical College and Hospital, dated-: 18th March, 2016).
Inclusion criteria: The patients of both sexes with papulosquamous disorders according to International Statistical Classification of Diseases and Related Health problems-tenth edition (ICD-10) [9] who attended the Dermatology Outpatient Department (OPD) during the study period were included.
Exclusion criteria: Patients who did not give consent for the study, pregnant and lactating females were excluded. Patients who had history of using artificial nails were also excluded as acrylic nails can induce severe nail changes.
Sample size calculation: Sample size was estimated using the formula:
n=Z2 p(1-p)/d2, assuming a prevalence of 10% (p) [2], confidence interval of 95% whose value is 1.96 (Z) and absolute precision of 6% (d). n=(1.96)×(1.96)×(0.1)×(0.9)/(0.06)(0.06). The derived sample size was 96. Then 8% was added for non response. Hence, the final sample size was calculated as 104 cases.
Thus, 104 cases of papulosquamous disorder were enrolled for the study.
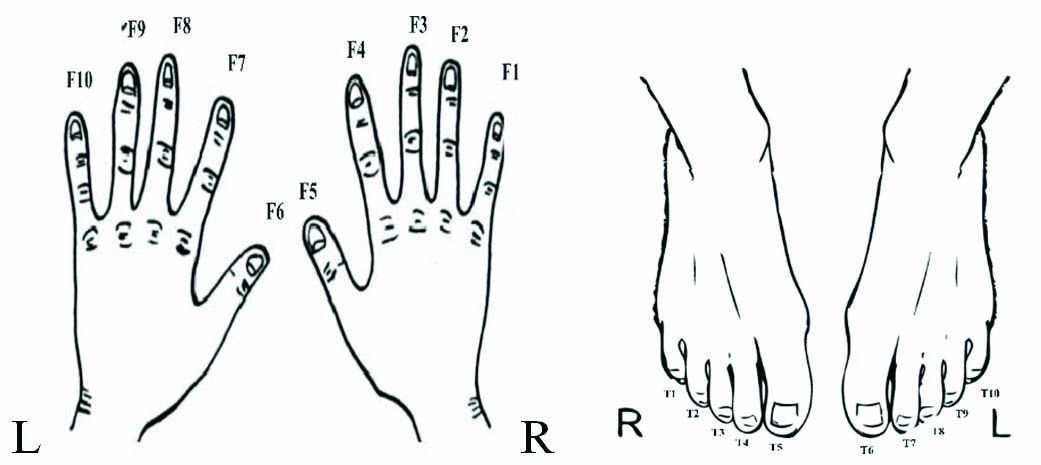
The type of papulosquamous disorder, presence of nail changes and their various patterns, the onset, progress and duration of skin and nail lesions were noted in detail. The co-morbidities were also noted. The toe nails were numbered 1 to 10 from right to left with right little toe was assigned number 1 and left little toe number 10. Similar numbering was given to fingers with the hand placed on the table with dorsum upwards [Table/Fig-1]. Thorough and detailed nail examination was carried out regarding the number of nail involvement, common nail to be involved and the different types of nail changes. Nail biopsy was not done as most of the patients did not give consent. Scrapping of nails for KOH mount was done for all cases.
Method of numbering digits.
The digits are numbered and read from right to left
Statistical Analysis
Data entry was done with Microsoft excel and analysis was done with Epi Info. Qualitative variables were expressed as percentage. Quantitative variables were expressed as mean.
Results
Among the 104 cases of papulosquamous, 61(59%) were males and 43 (41%) were females. Majority of the cases (n=29; 27.5%) were in 31-45 years age group (M=19; F=10) followed by 46-60 years (M=15; F=12). Least number of cases were in >60 years age group (n=8; 9.5%) as shown in [Table/Fig-2].
Age and sex distribution in papulosquamous disorder.
| Age (in Years) | Male | Female | Total |
|---|
| <12 | 10 | 5 | 15 (14%) |
| 13-30 | 12 | 13 | 25 (23.5%) |
| 31-45 | 19 | 10 | 29 (27.5%) |
| 46-60 | 15 | 12 | 27 (25.5%) |
| >60 | 5 | 3 | 8 (9.5%) |
| Total | 61 | 43 | 104 (100%) |
When all the 104 cases were clinically examined, nail changes were observed in 71(68%) cases. The age and sex distribution of these cases with nail changes is depicted in [Table/Fig-3].
Age and sex distribution in papulosquamous disorders with nail changes.
| Papulosquamous disorders with nail changes | Age and sex distribution |
|---|
| <12 years | 13-30 years | 31-45 years | 46-60 years | >60 years |
|---|
| M | F | M | F | M | F | M | F | M | F |
|---|
| Psoriasis (n=47; 66%) | 1 | 0 | 0 | 4 | 13 | 8 | 5 | 9 | 5 | 2 |
| Lichen Planus (n=9; 13%) | 0 | 1 | 1 | 0 | 3 | 2 | 0 | 1 | 0 | 1 |
| Pityriasis Rubra Pilaris (n=7; 10%) | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Lichen Nitidus (n=3; 5%) | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lichen Striatus (n=2; 3%) | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pityriasis Rosea (n=1; 1%) | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Paraps-oriasis (n=1; 1%) | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Pityriasis Lichenoides (n=1; 1%) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total (n=71)M=38 (54%)F=33 (46%) | 6 (8%) | 3 (6%) | 3 (4%) | 5 (7%) | 18 (23%) | 11 (13%) | 6 (8%) | 11 (15%) | 5 (10%) | 3 (7%) |
M: Male; F: Female
Males (n=38; 54%) were more affected than females (n=33; 46%) in the ratio 1.2:1. It was noted that majority of the nail disorders (n=29; 41%) were in 31-45 years age group and most of them were males (n=18; 23%). Psoriasis (n=47; 66%) was the most common papulosquamous disorder with nail changes followed by Lichen planus (n=9; 13%). In both diseases, males were more affected and were in the 31-45 years age group. In lichen nitidus (n=3) and lichen striatus (n=2), nail changes were noted only in children <12 years age. In the elderly age group (>60 years) nails were affects only in psoriasis (n=7) and Lichen planus (n=1). The nails were least affected in pityriasis rosea, Parapsoriasis and pityriasis lichenoides (n=1) [Table/Fig-3].
In the study population, all the cases of psoriasis (n=47; 100%) and pityriasis rubra pilaris (n=7; 100%) had nail changes as shown in [Table/Fig-4].
Characteristics of nail changes in Papulosquamous Disorders.
| Papulosquamous disorders n=104 | No. of cases with nail changes in the study population n=71/104 (68.2%) | Common nails involved | Time interval between onset of skin lesion and nail disease | Most common nail change in each disorder |
|---|
| Psoriasis (n=47) | 47 (100%) | F4,5,T5 | 4.2 years | Pitting |
| Lichen Planus (n=23) | 9 (39.1%) | F 4 | 1.2 years | Thinning of nail plate |
| Pityriasis Rosea (n=10) | 1 (10%) | F 6 | 2 months | Beau’s Line |
| Pityriasis Rubra Pilaris (n=7) | 7 (100%) | T5,6 | 6 Months | Nail plate thickening |
| Lichen Nitidus (n=5) | 3 (60%) | F3,4 | 3 months | Leukonychia |
| Lichen Striatus (n=4) | 2 (50%) | F4 | 4 months | Longitudinal striation |
| Parapsoriasis (n=3) | 1 (33.3%) | F5,T5 | 1.4 years | Beau’s line |
| Pityriasis Lichenoides (n=5) | 1 (20%) | T5,6 | 3 months | Beau’s line |
F: Fingernail; T: Toe nail
The incidence of nail involvement was least in pityriasis rosea (n=1; 10%). The mean duration of onset of nail changes following appearance of skin lesions was longer for psoriasis (4.2 years) and shorter for Pityriasis rosea (two months). The common nails involved and the most common nail changes in each papulosquamous disorder are shown in detail in [Table/Fig-4].
The KOH mount for onychomycosis was positive among 5 (7.8%) cases with nail changes and all of them had psoriasis.
Pitting of nails (n=44; 62%) was the most common nail pattern noted followed by subungual hyperkeratosis (n=24; 34%), thick nail and longitudinal striations (both n=19; 27%). The least common nail pattern was pterygium (n=1; 1%) as shown in [Table/Fig-5]. Upper limb nails were more affected than lower limb nails in general.
Nail patterns observed in the papulo squamous disorders in descending frequency.
| Nail changes | Most common limb/Nail involved | Ps n=47 n (%) | LP n=9 n (%) | PRP n=7 n (%) | L.S n=2 n (%) | LN n=3 n (%) | PR n=1 n (%) | Pp n=1 n (%) | PLC n=1 n (%) | Total n=71 n (%) |
|---|
| Pitting | UL/F4,5 | 37 (79%) | - | 7 (100%) | - | - | - | - | - | 44 (62%) |
| SUH | LL/T5 | 19 (40%) | - | 5 (71%) | - | - | - | - | - | 24 (34%) |
| Thick nail | LL/T7 | 12 (25.5%) | - | 7 (100%) | - | - | - | - | - | 19 (27%) |
| Longitudinal striations | LL/T5 | 16 (34%) | 2 (22%) | - | 1 (50%) | - | - | - | - | 19 (27%) |
| Beau’s lines | LL/T6 | 11 (23%) | 1 (11%) | 3 (42.8%) | - | - | 1 (100%) | 1 (100%) | 1 (100%) | 18 (25%) |
| Rough nails | LL/T5 | 16 (34%) | 2 (22%) | - | - | - | - | - | - | 18 (25%) |
| Onycholysis | UL/F6 | 17 (36%) | - | - | - | - | - | - | - | 17 (24%) |
| Oil drop sign | UL/F8 | 15 (32%) | - | - | - | - | - | - | - | 15 (21%) |
| Onychomedesis | LL/T5 | 13 (27.6%) | - | - | - | - | - | - | - | 13 (18%) |
| Longitudinal melanonychia | LL/T7 | 7 (14.8%) | 4 (44%) | - | - | - | - | 1 (100%) | - | 12 (17%) |
| Splinter haemorrhage | UL/F5 | 7 (14.8%) | - | - | - | - | - | - | - | 7 (9%) |
| Nail dystrophy | LL/T7 | 4 (8.5%) | 1 (11%) | - | - | - | - | - | - | 5 (7%) |
| Thin nails | UL/F5 | - | 5 (55%) | - | - | - | - | - | - | 5 (7%) |
| Leukonychia | UL/F5 | - | - | - | 1 (50%) | 3 (100%) | - | - | - | 4 (6%) |
| Trachyonychia | All | - | 3 (33%) | - | - | - | - | - | - | 3 (4%) |
| Pterygium | UL/F2 | - | 1 (11%) | - | - | - | - | - | - | 1 (1%) |
Ps: Psoriasis; LP: Lichen planus; PRP: Pityriasis rubra pilaris; LS: Lichen striatus; PR: Pityriasis rosea; Pp: Parapsoriasis; PLC: Pityriasis lichenoides chronica; SUH: Subungual hyperkeratosis; UL: Upper limb; LL: Lower limb; F: Finger nail; T: Toe; n: is no. of subjects in each category. The total no. of changes in nail varies
Psoriasis patients with nail changes were found to have many other comorbidity like diabetes mellitus, hypertension and atopy [Table/Fig-6]. Arthritis was present only in psoriasis patients with nail involvement (n=10; 21%). One case of psoriasis and three cases of Pityriasis rubra pilaris had Human Immunodeficiency Virus (HIV).
Co-morbidities in papulosquamous disorders with nail changes.
| Papulosquamous disorders n=71 | Co-morbidities in papulosquamous disorders with nail changes |
|---|
| Diabetes mellitus | Hypertension | HIV | Atopy | Arthritis |
|---|
| Psoriasis (n=47) | 7 (15%) | 11 (23%) | 1 (2%) | 9 (19%) | 10 (21%) |
| Lichen Planus (n=9) | - | - | - | 1 (11%) | - |
| Pityriasis Rubra Pilaris (n=7) | - | - | 3 (43%) | 1 (14%) | - |
| Lichen Nitidus (n=3) | - | - | - | 2 (66%) | - |
| Lichen Striatus (n=2) | - | - | - | | - |
| Pityriasis Rosea (n=1) | - | - | - | - | - |
| Parapsoriasis (n=1) | - | - | - | - | - |
| Pityriasis Lichenoides (n=1) | - | - | - | 1 (100%) | - |
HIV: Human immunodeficiency virus
Psoriasis (Ps): Of the 104 cases, 47 cases had psoriasis and all were found to have nail changes. The most common pattern of nail change observed was pitting (n=37) followed by subungual hyperkeratosis (n=19) [Table/Fig-5] and onycholysis (n=17). The least common nail abnormality observed was nail dystrophy (n=4) followed by longitudinal melanonychia (n=7) and splinter haemorrhage (n=7). Finger nail was more frequently involved than toe nail. The most common nail abnormality seen in finger nail was pitting and most common nail abnormality seen in toe nail was subungual hyperkeratosis [Table/Fig-7]. The most common nail involved in upper limb was thumb (F5) and index finger (F4). The commonest toe nail involved in lower limb was great toe nail (T5). The mean time gap between the onset of skin lesion and nail changes was 4.2 years.
Psoriasis- subungual hyperkeratosis.

Lichen Planus (LP): There were 23 cases of Lichen planus and of them nine showed nail changes. Nail changes were more frequently observed in finger nails than toe nails. The most common nail involvement seen in lichen planus was thinning of nail plate (n=5; 55%) especially in finger nails followed by longitudinal melanonychia mainly in toe nails (n=4; 44%) [Table/Fig-5]. The least common nail changes were pterygium, dystrophic nails and Beau’s lines. The maximum time interval between the onset of skin lesions and nail changes was 1.2 years. The most common nail involved in lichen planus was F4 (right ring finger nail). A total of 3 (33 %) patients had trachyonychia or Twenty-nail dystrophy [Table/Fig-8].
Lichen planus- twenty-nail dystrophy.

Pityriasis Rubra Pilaris (PRP): All the seven cases of PRP had nail changes. The most common nail involved was great toe nail (T 5,6). [Table/Fig-4]. The most common nail pattern abnormality noted was thickening of nail plate and pitting (n=7) followed by subungual hyperkeratosis (n=5) and Beau’s lines (n=3) [Table/Fig-5].
Lichen Nitidus (LN): Three out of the five cases of LN had nail changes and all had leukonychia. Most common nail involved was middle finger nail (F3) and index finger nail (F4).
Lichen Striatus (LS): Of the four cases of LS, two had nail changes. Longitudinal striations with thinning of nail plate were seen in one patient involving the index fingers (F4). The other nail change observed was punctate leukonychia.
Pityriasis Rosea (PR): In this study, PR was seen in 10 patients. Of them, only one patient had nail changes. He had Beau’s line which appeared after three months of onset of skin lesions.
Parapsoriasis (Pp): Beau’s lines were seen in thumb nails and longitudinal melanonychia was observed in great toe nail in one of the three cases of Parapsoriasis.
Pityriasis Lichenoides Chronica (PLC): Out of the five cases of pityriasis lichenoides only one had nail changes. Beau’s lines were seen over both great toes.
Psoriasis and lichen planus had most number of nail pattern changes while para psoriasis and pityriasis lichenoides had the least. Beau’s lines was observed in most of the papulosquamous disorders except Lichen nitidus and Lichen striatus. Time gap for onset of nail lesion was longer for psoriasis and shorter for pityriasis rosea.
Discussion
The papulosquamous disorders have gained considerable importance due to the sheer number of cases seen in the daily practice. All of them present with papules, scaly plaques or patches, leading to a clinical dilemma on arriving upon an accurate diagnosis. Distinguishing each disease becomes the need of the hour as treatment and prognosis for each is specific. As most of the papulosquamous disorders have nail changes with specific patterns, a thorough examination of all the 20 nails will definitely help to distinguish that particular papulosquamous disorder and manage accordingly.
This present study was done at Government Coimbatore Medical College, Coimbatore to observe such nail patterns specific to various Papulosquamous disorders. In the present study, out of 104 cases, 71 (68%) had nail changes. Majority (41%) of them were in 31-45 years age group. Males were more affected than females in the ratio 1.2:1. This correlated with the study done by David BG et al., where about 39 were males and 11 were females in 50 cases of papulosquamous disorders with nail changes [8]. But their mean age was 46.5 years. In this study, psoriasis was the most common papulosquamous disorder which correlates with many previous studies done on this topic of interest [5,6,10].
David AR et al., have noted that 1.5-3% of population have psoriasis and upto 50% of psoriatics have nail involvement. This proportion may cumulatively increase to 80-90% over their lifetime [11]. All the psoriasis patients (100%) in this study had nail changes. Klaassen KM et al., have noted that patients with psoriasis capitis, genital psoriasis, and psoriatic arthritis have a higher frequency of nail involvement [5]. In an observation by Gladman DD and, Rahman P; the incidence of psoriatic arthritis was 7% in psoriasis patients [12]. Raposo I and Torres T has noted that psoriatic arthritis show a higher percentage of nail involvement (70-80%) [13]. In this study, psoriatic arthritis was seen in 10 cases (21%) and all of them (100%) had nail changes.
Nail psoriasis affects the finger nails more commonly than toe nail [14]. In a study, on nail psoriasis by Ghosal A et al., 32% finger nail and 24% toe nail involvement were noted. Similar findings were observed in this study [6]. Characteristics of nail psoriasis begin principally after the onset of skin lesions [14]. In this study, the time interval between onset of skin lesion and nail lesion for psoriasis was 4.2 years; whereas it was nine and 11.5 years in studies by Klaassen KM et al., and Vander Velden HM et al., respectively [5,15]. According to studies by Klaassen KM et al., and Ghosal A et al., the most common feature of nail psoriasis is pitting [5,6]. In psoriasis patients in this study, pitting was the most common nail change, especially in finger nails and subungual hyperkeratosis was more common in toe nails. This was comparable to the study conducted by Salomon J et al., where pitting and subungual hyperkeratosis were the most common finger and toe nail changes noted in 65% and 33% cases of psoriasis, respectively [10]. In this study, right thumb and index finger nail were commonly affected in upper limb and right great toe was most affected in lower limb. Brazzelli V et al., had reported similarly that the fourth fingernail (index finger) and first great toe nail were the most affected finger and toe nails in nail psoriasis [16].
In lichen planus, nail changes are present in nearly 5-10% of patients and are more common in children. Permanent nail change can occur in one or more nails in 4% of affected individuals [17]. In this study, out of 23 cases of LP, 9 (39.5%) patients had nail changes. The characteristic nail changes observed were thinning, longitudinal melanonychia, and trachyonychia. In a study by Scher RK and Fischbein R; 10% of patients affected by nail lichen planus had trachyonychia or twenty nail dystrophy [18]. Among the nine LP patients with nail changes, 3 (33%) patients had twenty-nail dystrophy in this study. Lichen planus in children can present as twenty-nail dystrophy and resolve spontaneously as per study by Grover C et al., [17]. In a study conducted by Scheinfeld NS et al., trachyonychia was found to be common in children between age of 3-12 years [19]. In this study, of the three cases of trachyonychia, two were children. David BG et al., noted in their study that nail changes were frequently observed in finger nails than toe nails which is comparable to this study [8]. In this study, the most common nail involved in lichen planus was F4 (right hand ring finger nail). The most common nail changes observed were thinning of nail plate and longitudinal melanonychia in finger and toe nails, respectively.
In pityriasis rubra pilarisis patients of this study, the most common nail changes observed were thickening of nail plate, pitting and subungual hyperkeratosis which is comparable to the study by Mortimer PS and Dawber RP; [20]. Most common nail involved were great toe nails of both feet.
There are reports of onychodystrophy developing two months after appearance of skin lesions in pityriasis rosea. In this study, only one patient out of the 10 cases of PR had Beau’s lines after two months of onset of skin lesions, which is comparable to a literature which reports nail changes comprising of multiple transverse indentations and pitting [21].
In this study, all the patients with lichen nitidus were children less than 12 years of age. Leukonychia was seen in three patients which is similar to an observation by Natarajan S and Dick DC who noted that nail changes are mild and restricted in LN [22]. The most characteristic nail lesions are irregular longitudinal grooving and ridging of the nail plate. Rarely, trachyonychia was observed by Albayrak H et al., which was not observed in this study [23].
Tosti A et al., reported longitudinal ridging and splitting as the common features of nail involvement in lichen striatus [24]. The most frequent pattern of nail involvement as observed by Shilpa YK et al., was single finger nail change and the nail most commonly affected being the thumb [25]. In this study two patients of lichen nitidus had longitudinal striations and leuconychia affecting right great toe and thumb nail respectively.
In this study, only one patient of parapsoriasis and pityriasis lichenoides chronic had nail changes presenting as Beau’s line involving the thumb nail and great toe nail.
Limitation(s)
This study conducted in a single city with a less sample size cannot be extrapolated to the general population. It is from a Government college hospital which draws patients of low socio-economical background which might have influenced its outcome. There is very less number of similar studies to compare and contrast. Though, it is the main reason for undertaking this study, the same happens to be a limitation too.
Conclusion(s)
In this study, it was observed that the nail changes were more common in psoriasis, lichen planus and pityriasis rubra pilaris among the papulosquamous disorders. Pitting and subungual hyperkeratosis were the highly frequent nail patterns. Nail changes form an indispensible part of papulosquamous disease manifestation. Its degree of involvement is well correlated with the disease severity. The pattern of involvement is unique to the various disease subsets of the papulosquamous penumbra. In spite of the above credentials, nail changes in papulosquamous disorders other than psoriasis and lichen planus are not much discussed in the medical literature. This study conducted in a medical college hospital has thrown light on the clinical importance of nail changes in all the papulosquamous disorders and emphasised the need for more such studies in future.
M: Male; F: Female
F: Fingernail; T: Toe nail
Ps: Psoriasis; LP: Lichen planus; PRP: Pityriasis rubra pilaris; LS: Lichen striatus; PR: Pityriasis rosea; Pp: Parapsoriasis; PLC: Pityriasis lichenoides chronica; SUH: Subungual hyperkeratosis; UL: Upper limb; LL: Lower limb; F: Finger nail; T: Toe; n: is no. of subjects in each category. The total no. of changes in nail varies
HIV: Human immunodeficiency virus