A crucial understanding of teeth’ internal and external anatomy is critical for the successful outcome of endodontic therapy. The presence of two palatal roots in maxillary molars, particularly in the second molar is rare. The present case report addresses this anatomical variation in an 18-year-old female patient with a chief complaint of severe pain in the upper left back teeth region since one week. Preoperative radiographic evaluation of maxillary second molar did not reveal the aberrant anatomy due to its location and impaction of maxillary third molar onto the roots of the second molar. After access opening, inspection of the pulp chamber floor revealed a slightly deviated location of the palatal canal and a bleeding point mesial to the palatal canal. Intensive exploration for determining any additional canals was done using David Green (DG) 16 endodontic explorer under 3X magnification using dental loupes. A narrow field of view Cone Beam Computed Tomography (CBCT) was obtained to evaluate the unusual root canal morphology. Following a thorough analysis of CBCT, root canal treatment was performed employing a standard protocol. This case report highlights the successful diagnosis and management of the bilateral maxillary second molar with two separate palatal roots. With CBCT and magnification, determining the root morphology and canal configuration will be more accurate, further improving the quality of root canal treatment.
Case Report
An 18-year-old female patient with a non contributory medical history presented to the Department of Conservative Dentistry and Endodontics with the chief complaint of pain in her maxillary left back tooth region for one week. The pain was intermittent throughout the day, non radiating, aggravated by taking cold, hot foods and on mastication. The patient gave a history of previously initiated root canal therapy from a private dental center one week back. Due to the Coronavirus Disease (COVID) pandemic, the previous clinician was unavailable and hence she visited our institute. Clinical examination revealed a tooth restored with temporary filling with respect to 27, tender on percussion with no associated swelling. Pulp vitality testing of the involved tooth showed no response to electronic pulp tester (SybronEndo, Orange, CA) and cold (Endofrost, coltene). Preoperative radiographic evaluation revealed an access cavity filled with radiopaque restorative material with a slight widening of periodontal ligament space with respect to 27.
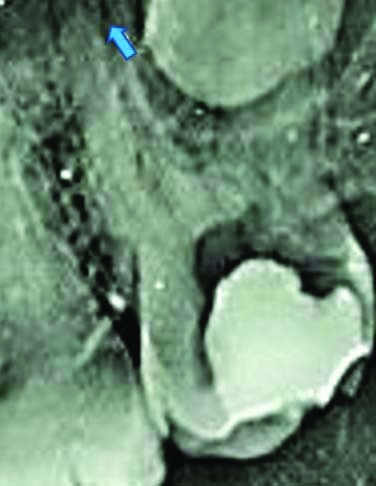
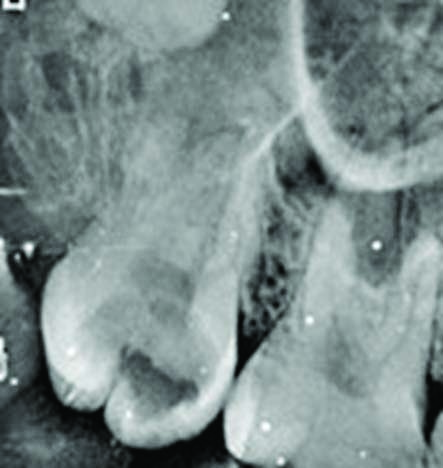
Hence, a diagnosis of previously initiated root canal therapy with symptomatic apical periodontitis was established based on clinical and radiographic findings [Table/Fig-1]. Informed consent was taken and the tooth was anaesthetised with Posterior Superior Alveolar (PSA) nerve block using 2% lignocaine (Astra Zeneca Pharma India Limited, Bangalore, India) and isolated with a rubber dam (Coltène/ Whaledent, OH, USA). After temporary restoration removal, pulp chamber revealed three canals and a bleeding spot in the floor of the pulp chamber mesial to the palatal canal and was assumed as perforation. The Intraoral Periapical (IOPA) radiograph of the concerned tooth did not offer any conclusive information. Inspection of the chamber floor for determining any additional canals was done using DG 16 endodontic explorer (Hu- Friedy, USA) under 3X magnification using dental loupes (Daray, Derbyshire). Intensive exploration revealed a catch at the bleeding point. A sterile cotton pellet was placed inside the pulp chamber, and the access cavity was sealed with Intermediate Restorative Material (IRM) (Caulk, Dentsply, USA).
Preoperative radiograph in which access opening has been done #27 with arrow mark depicting widening of periodontal ligament space at the periapex.
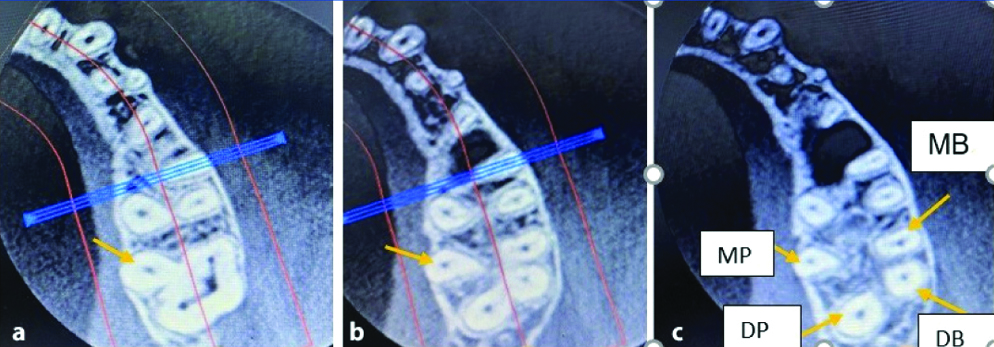
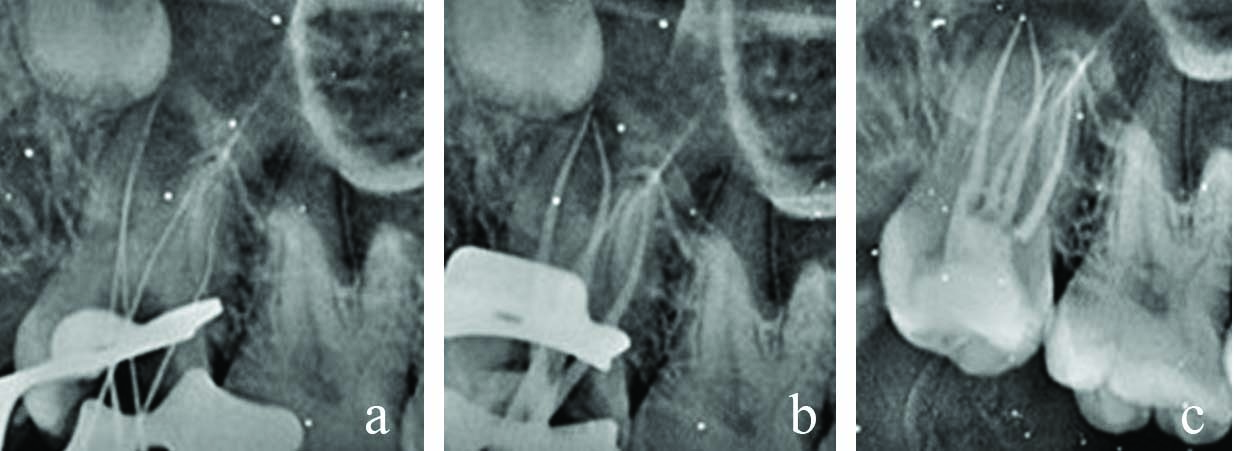
A CBCT (Carestream/Trophy, Marne-la-Vallée, France) of the partial arch was taken with exposure parameters of 120 kV and 5.0 Ma to evaluate whether it is an extra canal or an extra root and also to study its anatomy. An ultra-low radiation dose scan was done using a focused field of view. The images were reconstructed at 0.2 mm thickness increments. Axial view of CBCT with respect to 27 showed the presence of an additional palatal root [Table/Fig-2a-c]. Tooth 27 had four canals with four roots mesiobuccal, distobuccal, mesiopalatal, distopalatal. Initial instrumentation was performed using a 10 k-file (Mani, Inc, Tochigi, Japan). Coronal enlargement was done with Hyflex Electrical Discharge Machining (EDM) orifice opener (Coltene– Whaledent, Allstetten, Switzerland) to obtain straight line access. Each canal’s working length was determined using an electronic apex locator (Root ZX, J Morita Mfg. Corp., Japan) and confirmed radiographically with an IOPA [Table/Fig-3a].
Transverse section of CBCT showing four roots with four canals at a) cervical, b) middle, c) apical third respectively # 27 (MB mesiobuccal DB distobuccal MP mesiopalatal DB distopalatal, respectively.
a-c) Radiograph showing working length of all four roots #27, Master cone placement #27, Postoperative radiograph of maxillary second molar restored with bulk fill composite #27 respectively.
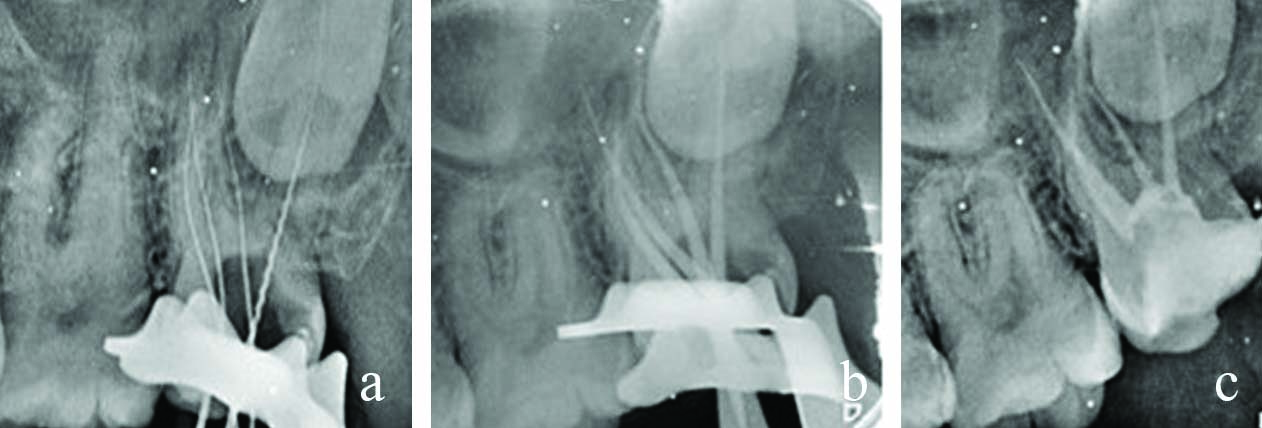
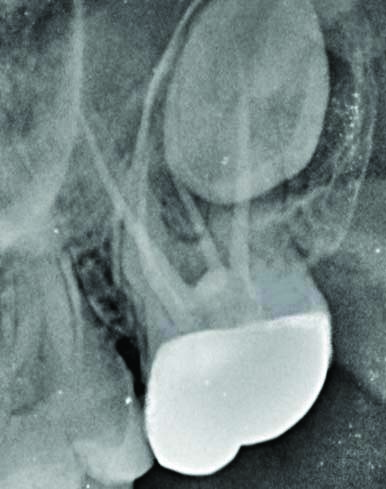
Glide path was established with 10/05 Hyflex EDM file ((Coltene- Whaledent, Allstetten, Switzerland) followed by which canals instrumented with Hyflex EDM rotary files till 25/~ (Coltene- Whaledent, Allstetten, Switzerland). Copious irrigation of the canals was done with 5ml of 3% Sodium Hypochlorite (NaOCl) (Vensons India, Bengaluru, India) and 5mL of 17% Ethylene Diamine Tetra-acetic Acid (EDTA) (Prime dental Pvt., Ltd., Thane) liquid between each file. With each irrigation flush of NaOCl and EDTA, sonic agitation of irrigant was done using an endoactivator (Dentsply Sirona) for one minute. Distilled water (Milli-Q water system, Millipore Corporation, Bedford, MA, USA) was used as the final irrigant. Root canals were dried with paper points and obturated with corresponding 25 size gutta-percha (Coltene-Whaledent, Allstetten, Switzerland) and AH plus sealer in the same visit (Dentsply, Konstanz, Germany) [Table/Fig-3b]. Finally, the tooth was restored with a bulk-fill composite restoration (EverX Posterior (EP)/GC Europe [Table/Fig-3c]. At one month follow-up, due to financial constraints and less interocclusal clearance, cast metal crowns were delivered to the patient. After one year of tooth number 27, the clinical and radiographic follow-up revealed that the patient was asymptomatic and periapical tissues were healthy [Table/Fig-4].
A one year follow-up radiograph.
As the same patient was asymptomatic with relation to 17 during the initial visit and due to financial constraints, she deferred the endodontic treatment. However, she developed severe pain in the upper right back tooth region of the jaw after ten days. The patient complained of lancinating pain, which was intermittent, non radiating, aggravated on mastication, cold foods, and relieved on taking medication, and there was no associated swelling #17. The clinical examinations revealed deep occlusal caries wrt. maxillary right second molar which was tender on percussion [Table/Fig-5]. Vitality testing of the involved tooth showed lingering pain to cold test and premature response to electric pulp tester (SybronEndo, Orange, CA).
Preoperative radiograph depicting wide occlusal caries with pulpal involvement #17.
Based on the findings, a diagnosis of symptomatic irreversible pulpitis with symptomatic apical periodontitis was made. The root canal treatment procedure was explained, and informed consent was taken. Preoperative radiographic evaluation revealed atypical root canal anatomy. Careful periodontal probing from mesial to distal side on the palatal aspect revealed a concavity on palatal surface and the probe dipped in the centre of palatal surface indicating a furcation. On either side of this concavity, two contours were appreciated hence the clinical examination confirmed two palatal roots. The tooth was anaesthetised with a Posterior Superior Alveolar (PSA) nerve block with 2% lignocaine (Astra Zeneca Pharma India Limited, Bangalore, India) and isolated with a rubber dam. Following access opening, based on the clinical experience gained from the previous tooth #27 and slightly deviated location of the palatal canal, the access cavity was modified from conventional triangular to trapezoidal shape to achieve straight line access for all canals [Table/Fig-6]. The second palatal canal orifice was explored with the aid of a DG-16 explorer (Hu- Friedy, USA), and its presence was confirmed with a dental operating microscope at 5X magnification (Labomed Dental Microscope Prima DNT, USA). It was found mesial to the usual location of the palatal canal [Table/Fig-6]. The mesiopalatal root showed moderate apical curvature towards the distal root, while the distopalatal root was relatively straight. The distance between the two palatal canal orifices was more trapezoid formed upon joining the imaginary lines connecting the four orifices was wider on the palatal side and narrower on the buccal side. The same treatment protocol was followed as in case report one [Table/Fig-7a-c]. After one year, the clinical and radiographic follow-up revealed that the patient was asymptomatic and periapical tissues were healthy [Table/Fig-8].
Clinical image under dental operating microscope.
MB: Mesiobuccal; DB: Distobuccal; MP: Mesiopalatal; DP: Distopalatal

a-c) Working length determined radiographically #17, Master cone placement #17, Obturation followed by postendodontic restoration #17.
A one year follow-up radiograph.

Discussion
Successful root canal treatment depends on thorough biomechanical instrumentation and three-dimensional obturation of the entire pulp space. Undetected extra roots or canals are recognised as a significant reason for the failure of root canal treatment [1,2]. Maxillary second molars have the most complicated root canal systems [3]. Kim Y et al., reported that in maxillary second molars 4.63% had one root, 10.72% had two roots, 82.7% had three roots, and 5.6% had four roots [4]. Four rooted molars with double palatal roots were reported to occur in 1.1% to 1.5% of maxillary second molars [5,6]. The bilateral occurrence of this phenomenon has also been documented [7].
In the present case, owing to the anatomical location of maxillary second molars and impaction of the third molar onto the roots of second molars, the unusual anatomy was not appreciable on a radiograph. Therefore, the concept of the narrow field of view CBCT provided a three dimensional (3D), low-radiation/high-resolution solution to assist successful endodontic diagnostic and treatment problems in case of variations in tooth anatomy [8,9].
With regard to tooth no 27, the extra root was successfully diagnosed and treated with the assistance of CBCT. Matherne RP et al., researched the benefit of CBCT imaging in endodontic treatment; they concluded that CBCT images always identified a greater number of root canal systems than digital images [10]. Purushotham M and Sahoo H treated a maxillary molar with the aid of a dental operating microscope and careful exploration of the pulp chamber with ultrasonic tips. Upon locating a bleeding point CBCT was taken to rule out any further complex anatomy similar to the present case report [11].
CBCT slices revealed four distinct roots with four canals. Moreover, mesiobuccal and distobuccal canals were relatively closer than the mesiopalatal and distopalatal canals. Thus, the box formed by joining the imaginary lines connecting the four orifices was wider on the palatal side, giving a trapezoidal shape [12]. A similar wider location of palatal orifices than palatal orifices was observed by Alani AH, Patel S and Patel P [7,13] Carlsen O and Alexandersen V classified these teeth according to the side of the crown with which the accessory palatal root is associated [14]. Hence according to this classification, this case belongs to radix mesiolingualis- the accessory root has an affinity to the pronounced mesiopalatal part of the crown. According to Ahmed HMA et al., the root canal configurations are depicted as 427 Mesio-buccal (MB)1 Distobuccal (DB)1 Mesiopalatal (MP)1 Distopalatal (DP)1, 417 MB1 DB1 MP1 DP1, respectively [15].
Not all scenarios need CBCT imaging. Al Qahtani A et al., published a case report describing the retreatment of maxillary second molars with two palatal roots. As the preoperative radiograph revealed four roots, they performed retreatment based on anatomic guide lines [16]. By relying on the experience and use of magnification, such variations could be treated successfully. The same was followed in case of tooth 17. Magnification aids like dental operating microscopes and loupes help to locate anatomic aberrations better by improving visualisation [13]. Thus precise access cavity and diagnostic aids such as dental operating microscope eliminate many potential problems such as missing additional canals and provide a better insight into root canal anatomy.
Conclusion(s)
Any variations in root canal morphology can be identified with the recent innovations in diagnostic and operating aids. Anatomical deviations can occur in any tooth; therefore, clinicians should anticipate these variations and utilise all the available diagnostic tools to manage them.
[1]. Vertucci FJ, Root canal morphology and its relationship to endodontic proceduresEndod Topics 2005 10(1):03-29.10.1111/j.1601-1546.2005.00129.x [Google Scholar] [CrossRef]
[2]. Cantatore G, Berutti E, Castellucci A, Missed anatomy: Frequency and clinical impactEndod Topics 2006 15(1):03-31.10.1111/j.1601-1546.2009.00240.x [Google Scholar] [CrossRef]
[3]. Badole GP, Bahadure RN, Warhadpande MM, Kubde R, A rare root canal configuration of maxillary second molar: A case reportCase Rep Dent 2012 2012:767582Epub 2012 Jul 810.1155/2012/76758222830061 [Google Scholar] [CrossRef] [PubMed]
[4]. Kim Y, Lee SJ, Woo J, Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: Variations in the number of roots and canals and the incidence of fusionJ Endod 2012 38(8):1063-68.10.1016/j.joen.2012.04.02522794206 [Google Scholar] [CrossRef] [PubMed]
[5]. Sımşek N, Keleş A, Bulut ET, Unusual root canal morphology of the maxillary second molar: A case reportCase Rep Dent 2013 2013:13823910.1155/2013/13823923573426 [Google Scholar] [CrossRef] [PubMed]
[6]. Yang B, Lu Q, Bai QX, Zhang Y, Liu XJ, Liu ZJ, Evaluation of the prevalence of the maxillary molars with two palatal roots by cone-beam CTZhonghua Kou Qiang Yi Xue Za Zhi 2013 48(6):359-62.Chinese [Google Scholar]
[7]. Alani AH, Endodontic treatment of bilaterally occurring 4-rooted maxillary second molars: Case reportJ Can Dent Assoc 2003 69(11):733-35. [Google Scholar]
[8]. Todd R, Cone beam computed tomography updated technology for endodontic diagnosisDent Clin North Am 2014 58(3):523-43.10.1016/j.cden.2014.03.00324993922 [Google Scholar] [CrossRef] [PubMed]
[9]. Abramovitch K, Rice DD, Basic principles of cone beam computed tomographyDent Clin North Am 2014 58(3):463-84.10.1016/j.cden.2014.03.00224993919 [Google Scholar] [CrossRef] [PubMed]
[10]. Matherne RP, Angelopoulos C, Kulild JC, Tira D, Use of cone-beam computed tomography to identify root canal systems in vitroJ Endod 2008 34(1):87-89.10.1016/j.joen.2007.10.01618155501 [Google Scholar] [CrossRef] [PubMed]
[11]. Purushotham M, Sahoo H, Cone beam computed tomography-aided endodontic management of second maxillary molar with two separate palatal roots: A case reportCureus 2020 12(3):e734710.7759/cureus.7347 [Google Scholar] [CrossRef]
[12]. Versiani MA, Pécora JD, de Sousa-Neto MD, Root and root canal morphology of four-rooted maxillary second molars: A micro-computed tomography studyJ Endod 2012 38(7):977-82.10.1016/j.joen.2012.03.02622703664 [Google Scholar] [CrossRef] [PubMed]
[13]. Patel S, Patel P, Endodontic management of maxillary second molar with two palatal roots: A report of two casesCase Rep Dent 2012 2012:590406Epub 2012 Dec 410.1155/2012/59040623304565 [Google Scholar] [CrossRef] [PubMed]
[14]. Carlsen O, Alexandersen V, Radix mesiolingualis and radix distolingualis in a collection of permanent maxillary molarsActa Odontol Scand 2000 58(5):229-36.10.1080/00016350075005178211144874 [Google Scholar] [CrossRef] [PubMed]
[15]. Ahmed HMA, Versiani MA, De-Deus G, Dummer PMH, A new system for classifying root and root canal morphologyInt Endod J 2017 50(8):761-70.10.1111/iej.1268527578418 [Google Scholar] [CrossRef] [PubMed]
[16]. Al Qahtani A, Abdulrab S, Alhadainy H, Management of a failed endodontic treatment for a maxillary second molar with two separate palatal rootsClin Case Rep 2018 6(9):1735-38.10.1002/ccr3.170830214753 [Google Scholar] [CrossRef] [PubMed]