Mimicker of Renal Cell Carcinoma- A Case Report
Giri Pranav1, Vasugi Arumugam2, Susruthan Murali3, Praveen Paul4, K Natarajan5
1 Medical Student (MBBS, 8th Semester), Department of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
2 Assistant Professor, Department of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
4 Postgraduate Student, Department of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
5 Professor, Department of Urology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vasugi Arumugam, Villivakkam, Chennai, Tamil Nadu, India.
E-mail: arumugamvasugi@yahoo.com
Oncocytoma is a rare epithelial tumour composed of oncocytes which are epithelial cells with excessive amount of mitochondria. The tumour is most often benign, and diagnosis can be made on the basis of histopathological examination. Here, the authors present a 64-year-old female patient, with complaints of abdominal discomfort and flank pain, along with history of loss of weight and appetite for one month. Radiology showed a left renal mass of measuring 9×7×4.5 cm involving the upper and middle pole suggestive of malignancy. Following which radical nephrectomy was done. Examination of gross specimen showed a fairly circumscribed brownish lesion in the upper and middle pole of left kidney measuring 8.8×7×4.5 cm with a central scar. There was no evidence of hilar and perirenal fat invasion. Histology showed sheets of large polygonal eosinophilic cells with centrally placed nucleus. The differentials were eosinophilic variant of clear cell renal cell carcinoma, chromophobe renal cell carcinoma and oncocytoma. A panel of Immunohistochemical (IHC) markers was performed for further categorisation and the lesional cells were positive for CD 117 and negative for CD 7 and CD 10. This ruled out the differentials and confirmed oncocytoma, thus ruling out the necessity for chemotherapy.
Immunohistochemistry, Nephrectomy, Oncocytoma
Case Report
A 64-year-old female patient, presented with complaints of abdominal discomfort and flank pain along with history of loss of weight and appetite for one month. On physical examination, there was a palpable mass in the left upper quadrant. Radiology revealed a large exophytic mass of size 9×7×4.5 cm involving the upper and middle pole of left kidney with a central scar. There was no evidence of renal sinus and renal vein involvement radiologically. The mass was thought to be malignant provisionally based on clinical and radiological features, following which a radical nephrectomy was done.
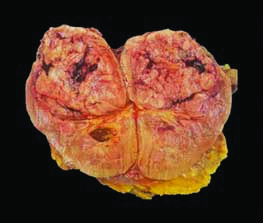
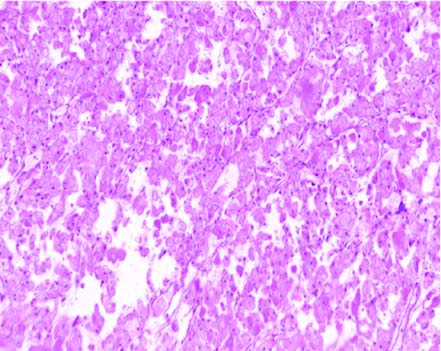
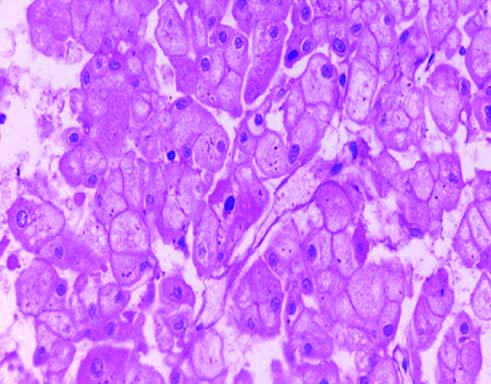
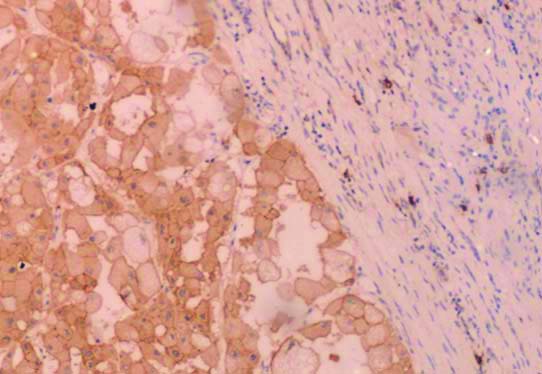
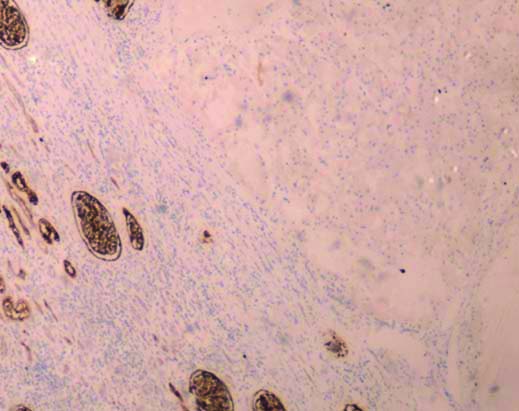
Examination of gross specimen showed a fairly circumscribed brownish lesion involving the upper and middle pole of left kidney measuring 8.8×7×4.5 cm with a central scar. There was no evidence of renal sinus, renal vein and perirenal fat invasion [Table/Fig-1]. Microscopy, revealed sheets of large polygonal eosinophilic cells arranged as cords and trabeculae [Table/Fig-2]. Individual cells were large with abundant eosinophilic granular cytoplasm and centrally placed round vesicular nucleus [Table/Fig-3]. The differentials were eosinophilic variant of clear cell renal cell carcinoma, chromophobe renal cell carcinoma and oncocytoma, all having similar morphology. A panel of IHC markers were performed and the lesional cells showed strong membraneous positivity for CD 117 [Table/Fig-4] and were negative for CD 7 and CD 10 [Table/Fig-5]. This ruled out the differentials and confirmed oncocytoma, thus ruling out the necessity for chemotherapy. Surgery remained the main stay of treatment and the patient was on follow-up for a period of one year and was doing well.
Gross image showing a well circumscribed lesion involving the upper and middle pole of left kidney.
Histology showing lesional cells arranged in cords and trabeculae (H&E, 100X).
Individual cells showing abundant eosinophilic granular cytoplasm and round nucleus (H&E, 400X).
Immunohistochemical (IHC) staining showing strong membraneous and cytoplasmic positivity for CD 117 (IHC, 200X).
Immunohistochemical (IHC) staining of CD 10 showing negative in lesional cells and positive in adjacent normal renal parenchyma (IHC, 200X).
Discussion
Renal oncocytomas are the second most common benign renal tumours that comprise approximately 3-7% of renal tubular epithelial tumours. Zippel L and Zur Kenntnis in 1942 reported the first case of renal oncocytoma [1]. Incidence commonly occurs in adults older than 50 years but a peak frequency is noted in the seventh decade of life. A slight male preponderance is noted [2]. The size may vary from 0.6-14 cm [3]. Most cases are diagnosed incidentally in radiology. However, some patients may present with flank pain, gross haematuria, dysuria, abdominal discomfort and a gross palpable mass [4]. Oncocytomas have a classic gross appearance. Most Oncocytomas have characteristic histological features which aids in the diagnosis, while few cases need the help of ancillary testing using immunohistochemistry to rule out the differential diagnosis. Cytogenetics may be rarely used for obtaining the definitive diagnosis.
Renal oncocytomas usually have an indolent course with excellent prognosis, but rarely few cases may have metastasis to liver and bone. Patients with rapid growth in tumour size have to be monitored and sampled extensively to rule out the possibility of coexisting renal cell carcinoma as Collision tumour. [5,6]. Surgical excision is curative if there have not been any metastases. However, metastases following radical nephrectomy have been reported [2].
Oncocytomas usually arise from the intercalated epithelial cells of the collecting duct. The genetic abnormalities associated with oncocytoma can be detected by karyotype analysis which includes diploid karyotype, loss of chromosome 1, loss of Y chromosome, rearrangement of 11q13 [2,4]. The 11q13 rearrangement affects the Cyclin D1 (CCND1) gene. It also has a close association with Birt-Hogg-Dube syndrome, which involves germline mutations in the folliculin gene (FLCN).
On radiology, they appear as well-circumscribed, homogenous solid masses with a central stellate scar, however scar may not be evident in few cases. Grossly, renal oncocytomas appear tan-brown or mahogany-coloured with a central stellate scar. Perinephric fat or rarely the renal vein involvement may be noted in few cases with no change in prognosis. Microscopically, the tumour cells are arranged as nests and tubules associated with fibrous or oedematous stroma. The tumour cells are large round eosinophilic with granular cytoplasm which is packed with mitochondria. Nuclei are round and homogenous and may contain small nucleoli. Tumour cells around the central scar may appear small with scant cytoplasm. Rarely, bizarre cells exhibiting moderate pleomorphism may be noted in some tumours. Atypical mitoses and necrosis are infrequent. Such non specific findings make a pathologist consider a list of differentials even after a frozen section examination [2].
Oncocytomas are usually incidentally detected on radiology done for non urological complaints. Distinguishing a benign oncocytoma from a malignant lesion like renal cell carcinoma or a Collision tumour like Hybrid Oncocytic Chromophobe Tumour (HOCT) will be difficult on radiology. Hence, most oncocytomas are erroneously operated upon suspicion that it may be a malignant tumour. The evaluation of a kidney mass can also be done with core biopsy, fine needle aspiration, or resection. If the histology and staining patterns are difficult to interpret, conventional karyotyping and Fluorescence in situ hybridisation (FISH) may be considered to look for a diploid karyotype of loss of chromosome 1, which would be supportive for the diagnosis of oncocytoma [8,9].
Hence, it is understandable that distinguishing oncocytomas from malignant mimics based only on Haematoxylin and Eosin (H&E) staining and radiology is often inconclusive. Immunohistochemistry is what helps a pathologist clinch the diagnosis. The differential diagnosis include eosinophilic variant chromophobe renal cell carcinoma, succinate dehydrogenase-deficient renal cell carcinoma, tubulocystic renal cell carcinoma, papillary renal cell carcinoma with eosinophilic cytoplasm, and epithelioid angiomyolipoma. Immunohistochemistry aids in differentiating oncocytoma from renal cell carcinoma [Table/Fig-6].
Immunohistochemical (IHC) staining pattern in oncocytomas.
| Immunohistochemical markers | Staining pattern |
|---|
| Cytokeratin 7 | Negative or scattered rare positive cells |
| AMACR | Positive in low intensity |
| Vimentin | Negative but can be positive in cells around central scars or in oncoblasts |
| CD117, KIT, kidney specific cadherin | Positive |
| Hale’s colloidal iron, HMB45, melan A | Negative |
*HMB: Human melanoma black; Melan A: Melanoma antigen
Surgical excision remains the main stay of treatment. Partial nephrectomy suffice if the lesion is less than 4 cm and located in either upper or lower pole of the kidney [8]. The present case was treated by radical nephrectomy considering the lesion size and location. Literature search of similar case reports with their clinical presentation, IHC staining pattern and modality of treatment were mentioned in [Table/Fig-7] [9-12].
Literature search of varied presentations of oncocytoma [9-12].
| Authors | Patient details | IHC workup | Treatment |
|---|
| Kolníková G et al., [9], 2014 | 69Y/M presented with stabbing abdominal pain. Abdominal USG examination showed a tumour in the right kidney with well-limited lesions in the left kidney and the lung. | Tumour cells had negative immunoreactivity for RCC antigen, CD10, AMACR, Vimentin and positive for CD117, CK 7, E cadherin and EMA. | Radical nephrectomy was carried out on the patient. Therapy is now centered on the squamocellular carcinoma of the lungs which was discovered incidentally. Patient is doing well 12 months post surgery. |
| Akbulut S et al., [10], 2010 | 25/F, abdominal pain and 3-year-old palpable mass, Intravenous Pyleogram (IVP) showed a mass associated with her left kidney, leading to left hydrourete-ronephrosis. | CD117, E-cadherin positivity; vimentin, RCC marker negativity | Laparotomy was performed via a midline incision; 3380 g mass arising from the left kidney was excised along with the kidney. Patient doing well on six months follow-up. |
| Liu G et al., [11], 2017 | 48/F, noted with multiple left-kidney masses and a history of multiple Schwannomas. CT found multiple lesions occupying parenchyma of the left kidney. | Immunochemistry staining was positive for PAX-8, CA9, AE1/AE3, CD10, CK7 (partially), Epithelial Membrane Antigen (EMA) (partially), and negative for P504, RCC, TFE3, and Vimentin. | Laparoscopic partial left nephrectomy was performed. Uneventful post operative recovery, no medical issues during two month follow-up. Diagnosis was confirmed to be a HOCT. |
| Gaeta R et al., [12], 2019 | 44/M with history of hiatal hernia and GERD presented with asthenia, nausea, fever, jaundice, caused by HBV. Abdominal USG identified a solid exophytic mass in the lower left renal pole. | Papillary component of the neoplasia showed positivity for CK7, vimentin, BerEP4 and a weak positivity for CD10, oncocytoma areas were positive for CD117 and negative for the cytokeratines, vimentin and CD10, suggesting a hybrid tumour. | The patient underwent robot-assisted enucleation of the tumour with preoperative placement of ureteral stent in order to prevent post-operative urinous fistula. |
IHC: Immunohistochemistry; USG: Ultrasonography; CT: Computed tomography; GERD: Gastro-esophagoeal reflux disease; HBV: Hepatitis B virus; M: Male; F: Female; RCC: Renal cell carcinoma; AMACR: Alpha-methylacyl-CoA racemase, EMA: Epithelial membrane antigen; CK: Cytokeratin; TFE3: Transcription factor E3; HOCT: Hybrid oncocytic/chromophobe tumour
Conclusion(s)
Oncocytomas are mimickers of renal cell carcinoma clinically and radiologically. Histology and IHC stains aids to provide a definitive diagnosis and defines the lesion characterisation. Partial nephrectomy is considered the most appropriate treatment for the majority of patients with oncocytomas while renal cell carcinomas involves radical nephrectomy and chemotherapy as modality of treatment.
*HMB: Human melanoma black; Melan A: Melanoma antigen
IHC: Immunohistochemistry; USG: Ultrasonography; CT: Computed tomography; GERD: Gastro-esophagoeal reflux disease; HBV: Hepatitis B virus; M: Male; F: Female; RCC: Renal cell carcinoma; AMACR: Alpha-methylacyl-CoA racemase, EMA: Epithelial membrane antigen; CK: Cytokeratin; TFE3: Transcription factor E3; HOCT: Hybrid oncocytic/chromophobe tumour
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 21, 2020
Manual Googling: Jan 16, 2021
iThenticate Software: Sep 27, 2021 (18%)
[1]. Zippel L, Zur Kenntnis, Der oncocytemVirchow Arch Pathol Anat 1942 308(1):360-82.10.1007/BF02593372 [Google Scholar] [CrossRef]
[2]. Romis L, Cindolo L, Patard JJ, Messina G, Altieri V, Salomon L, Frequency, clinical presentation and evolution of renal oncocytomas: Multicentric experience from a European DatabaseEur Urol 2004 45(1):53-57.10.1016/j.eururo.2003.08.00814667516 [Google Scholar] [CrossRef] [PubMed]
[3]. Alamara C, Karapanagiotou EM, Tourkantonis I, Xyla V, Maurer CC, Lykourinas M, Renal oncocytoma: A case report and short review of the literatureEuropean Journal of Internal Medicine 2008 19(7):e67-e69.10.1016/j.ejim.2008.03.00319013370 [Google Scholar] [CrossRef] [PubMed]
[4]. Chao DH, Zisman A, Pantuck AJ, Freedland SJ, Said JW, Belldegrun AS, Changing concepts in the management of renal oncocytomaUrology 2002 59(5):635-42.10.1016/S0090-4295(01)01630-2 [Google Scholar] [CrossRef]
[5]. Sejben I, Szabo Lukacs ZN, Lorand M, Farkas S, Gabor C, Papillary renal cell carcinoma embedded in an oncocytoma: Case report of a rare combined tumour of the kidneyCan Urol Assoc J 2013 (7-8):E513-16.10.5489/cuaj.41423914273 [Google Scholar] [CrossRef] [PubMed]
[6]. Vasuri F, Fellegara G, Collision renal tumoursInt J Surg Pathol 2009 17:338-39.10.1309/AJCPQ0P1YHDBZUFL26486747 [Google Scholar] [CrossRef] [PubMed]
[7]. Fan YH, Chang YH, Huang WJS, Chung HJ, Chen KK, Renal oncocytoma: Clinical experience of Taipei Veterans General HospitalJournal of the Chinese Medical Association 2008 71(5):254-58.10.1016/S1726-4901(08)70116-3 [Google Scholar] [CrossRef]
[8]. Dechet CB, Bostwick DG, Blute ML, Bryant SC, Zincke H, Renal oncocytoma: Multifocality, bilateralism, metachronous tumour development and coexistent renal cell carcinomaJ Urol 1999 162(1):40-42.10.1097/00005392-199907000-0001010379735 [Google Scholar] [CrossRef] [PubMed]
[9]. Kolníková G, Marinová P, Gál V, Mečiarová I, Mišanko V, Rampalová J, Renal Oncocytoma with Invasive Histopathologic Features- Case ReportKlin Onkol 2014 27(2):138-42.10.14735/amko201413724739051 [Google Scholar] [CrossRef] [PubMed]
[10]. Akbulut S, Senol A, Cakabay B, Sezgin A, Giant renal oncocytoma: A case report and review of the literatureJ Med Case Reports 2010 4:52https://doi.org/10.1186/1752-1947-4-5210.1186/1752-1947-4-5220205900 [Google Scholar] [CrossRef] [PubMed]
[11]. Liu G, Li Y, Li Z, Zhou J, Huo Z, Ji Z, Renal hybrid oncocytic/chromophobe tumour associated with multiple schwannomasMedicine (Baltimore) 2017 96(48):e893910.1097/MD.000000000000893929310387 [Google Scholar] [CrossRef] [PubMed]
[12]. Gaeta R, Tognetti A, Kauffmann EF, Pollina LE, Case report of a combined oncocytoma and type 1 papillary renal cell carcinoma: A rare entityPathologica 2019 111(1):37-40.10.32074/1591-951X-52-1831217621 [Google Scholar] [CrossRef] [PubMed]