Medial Malleolus Fracture Fixation in Weber Type B and C Ankle Injuries
Mohd Rafeeq Wani1, Stanzin Sonum2, Zubair Younis Ringshawl3
1 PhD Scholar, Department of Orthopaedics, Government Medical College, Srinagar, Jammu and Kashmir, India.
2 PhD Scholar, Department of Orthopaedics, Government Medical College, Srinagar, Jammu and Kashmir, India.
3 PhD Scholar, Department of Orthopaedics, Government Medical College, Srinagar, Jammu and Kashmir, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohd Rafeeq Wani, House No-042, Narkara, Budgam, Srinagar, Jammu and Kashmir, India.
E-mail: wanirafiq2011@gmail.com
Introduction
Medial malleolus fractures are commonly encountered by orthopaedic surgeons in their daily practice. Medial malleolus fractures are articular fractures and hence need anatomical reduction to prevent the potential complications. Many methods of fixation are in practice for fixing medial malleolus with the aim to achieve stable fixation and union of the fracture site.
Aim
To evaluate the outcome of medial malleolus fracture fixation by three different methods- two partially threaded screws, one partially threaded screw and one k-wire and tension band wiring, in Weber type B and C ankle injuries.
Materials and Methods
This prospective interventional study was conducted from August 2017 to September 2020 in a tertiary care orthopaedics hospital in Srinagar, Jammu and Kashmir, India. A total of 40 patients (aged 18 years or greater) of Weber B and C types medial malleolus fracture, were included in the present study. The medial malleolus was fixed with two partially threaded screws in 16 patients (Group A), one partially threaded screw and one Kirschner wire (K)-wire in 14 patients (Group B) and tension band wiring was done in 10 patients (Group C). The fixation was decided on intraoperative finding of fragment size and comminution as well as quality of bone. The parameters assessed were time of union, delayed union, non union, ankle range of motion and symptomatic hardware. One-way Analysis of Variance (ANOVA) test was used to compare parametric data of the three groups. The p-value <0.05 was considered statistically significant.
Results
The mean age of the patients was 40.20 years with range 18-65 years. 22 patients were females and 18 were males and the male to female ratio was 0.81. The mean time of healing of fracture was 10.25 weeks in group A, 11.14 weeks in group B and 10.80 weeks in group C. There were two cases of delayed union, one each in group B and C. Symptomatic hardware was mostly seen in group C. There was no case of non union in the present study.
Conclusion
It can be concluded that all the three fixation methods used in this study achieved the union in comparable time duration with no case of non union. A particular method of fixation should be used by taking into consideration the type of fracture, size of the fragment, comminution and quality of the bone.
Delayed union, Non union, Tension band wiring
Introduction
Ankle injuries are among the most common orthopaedic injuries in adults [1]. The ankle joint is a complex hinge joint composed of articulations between tibia, fibula and talus. Medial malleolus articulates with the medial facet of the talus. The anterior and posterior colliculus on medial malleolus serve as attachment sites for superficial and deep fibres of the deltoid ligament respectively. The deltoid ligament provides medial stability to the tibiotalar joint. Most of ankle fractures are malleolar fractures, and isolated medial malleolus fractures have been reported to occur in approximately 8% of patients [2-4].
Medial malleolus fractures are articular fractures and hence need anatomical reduction to prevent the potential complications. Surgery is needed in medial malleolar fractures for anatomic reduction and/or early joint range of motion [5,6]. Several surgical techniques are available for fixation of medial malleolar fractures which include lag screws, k-wires, tension bands, staples, etc., [7-11].
Open reduction and fixation of medial malleolar fractures with two lag screw and one partially threaded screws is the standard technique for treating medial malleolar injuries [9,12,13]. Sometimes the ability to place two screws within the fragment may not be possible because of fragment size or comminution [14]. In small avulsion fractures, osteoporotic fractures, and comminuted fractures of medial malleolus tension band wiring have been found very effective [8,15]. In the literature, various studies are there to compare the different methods of fixation but most have not mentioned about the fracture characteristics like size of fragment, comminution and quality of bone [16-18].
Hence, the present study was conducted to evaluate the outcome of open reduction and internal fixation of medial malleolus fractures using three methods of fixation by taking into consideration the type of fracture, fragment size, comminution and quality of bone.
Materials and Methods
This prospective interventional study was conducted from August 2017 to September 2020 in a tertiary care orthopaedics hospital in Srinagar, Jammu and Kashmir, India. Ethical clearance was received from Institutional Ethical Committee (GMCE-10563). A written informed consent was taken from each patient for their inclusion in the study. The study was conducted as per the Declaration of Helsinki [19].
Inclusion criteria: Patients aged 18 years or greater, Weber B and C type medial malleolus fracture were included in the study after obtaining the informed consent.
Exclusion criteria: Patients with open fractures, injury more than three-week-old, multiple injuries, patients not fit for anaesthesia and patients who were lost to follow-up were excluded from the study.
The total sample of 40 participants was formed after following the above criterias. Ankle injuries were classified as per the weber classification [20]. This is a radiographic classification and is based on the position of fibular fracture in relation to syndesmosis. Type A fractures are distal to syndesmosis, type B are fractures at the level of syndesmosis and type C fractures are proximal to the level of syndesmosis.
Surgical procedure: A thigh tourniquet was used in all patients. An anteromedial incision was used about 5 cm starting 2-3 cm proximal to the fracture and distally curved slightly anteriorly. The incision was made directly up to the bone. A 1-2 mm periosteum was removed adjacent to the fracture ends. The fracture site was cleared of any interposing soft tissue. The fracture was then reduced and held with a towel clamp. The size of fragment and comminution of the fragment was assessed intraoperatively and the method of fixation was chosen accordingly. The fracture was then fixed with the following three methods:
Group A: Medial malleolus fractures consisting of single large fragment were fixed with two 4 mm partially threaded screws. These were designated as group A and comprise of 16 patients;
Group B: Medial malleolus fractures in whom the fragment size was not large enough to accommodate the second screw were fixed with one partially threaded 4mm screw and one k-wire to provide rotational control. These patients were designated as group B and comprise a total of 14 patients; and
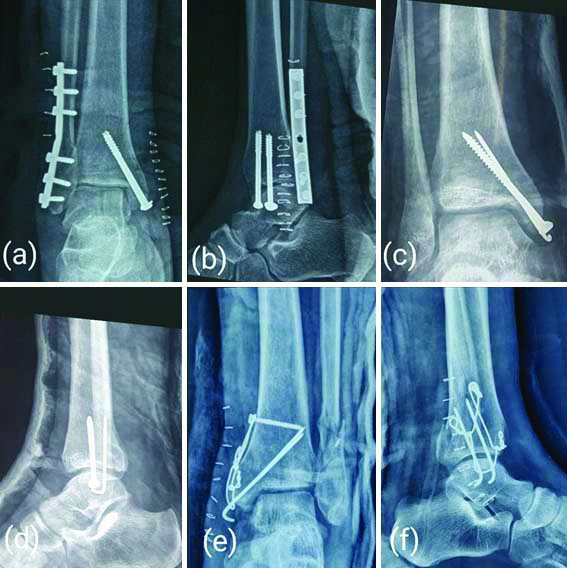
Group C: Medial malleolar fractures with small avulsed fragment, comminution and osteoporotic fragment were fixed with tension band wiring and were designated as group C. These constituted a total of 10 patients. Postoperative radiographs of medial malleolus fixation by three different methods are given in [Table/Fig-1].
Showing postoperative radiographs of medial malleolus fixation methods of few patients: a,b) 2 partially threaded screws; c,d) 1 partially threaded screw and 1 k-wire; e&f) tension band wiring.
A short leg cast was used for first six weeks after surgery. The patients were mobilised on the first postoperative day. Non weight bearing was advised for first six weeks and then weight bearing was advanced as per the radiological union of the fracture. The patients were periodically followed-up at two weeks, six weeks, three months, six months and final follow-up was done at one year. Patient demographic data (age, sex), mode of trauma, time interval between injury and surgery, surgical site infection, time of union, delayed union, non union, ankle range of motion and symptomatic hardware were assessed and recorded.
Fracture union was defined as resolution of the fracture line on radiographs, painless weight-bearing, and no or minimal tenderness to palpation over the fracture site. Delayed union was defined as time from fixation to fracture union greater than 12 weeks. Symptomatic hardware was diagnosed as patient having pain and there is tenderness on palpation over the prominent implant [21]. Total ankle range of motion includes both plantarflexion and dorsiflexion and was measured using a goniometer. Normal ankle range of motion in the sagittal plane varies between 65-75 degrees [22].
Statistical Analysis
Microsoft Excel was used for data compilation and statistical analysis was done using Statistical Package for Social Sciences (SPSS) Software, version 24.0, software (IBM, Armonk, NY). One-way ANOVA test was used to compare parametric data of the three groups. The p-value <0.05 was considered statistically significant.
Results
The study consisted of total of 40 cases. The patient characteristics and mode of trauma are given in [Table/Fig-2]. The mean age of the patients was 40.20 years with range 18-65 years. Twenty two patients were females and 18 were males and the male to female ratio was 0.81. The mode of injury was fall in 29 patients and 11 patients had trauma due to motor vehicle accident. Mean duration from the time since injury to surgery was 4.1 days with range 2-9 days. There was no statistically significant difference between the three groups in terms of age and interval time between injury and surgery (p-values of 0.701 and 0.733 respectively using one-way ANOVA test).
| Variables | Group A | Group B | Group C |
|---|
| No of patients | 16 | 14 | 10 |
| Age group (years) | 18-54 | 21-58 | 26-65 |
| Mean age (years)±SD | 38.68±10.84 | 39.35±10.70 | 45.30±13.45 |
| Sex | M: 9 | M: 6 | M: 3 |
| F: 7 | F: 8 | F: 7 |
| Sex ratio (male/female) | 1.28 | 0.75 | 0.42 |
| Mean interval time between injury and surgery (days)±SD | 4.06±2.23 | 3.85±1.65 | 4.50±2.24 |
| Mode of injury | Fall=11 | Fall=10 | Fall=8 |
| Motor vehicle accident=5 | Motor vehicle accident=4 | Motor vehicle accident=2 |
M: Male; F: Female
The average time of union of fracture was 10.25 weeks in group A, 11.14 in group B and 10.80 in group C. One-way ANOVA test showed no statistically significant difference in the three groups with respect to time of union (p-value=0.406) and ankle range of motion (p-value=0.514). At two weeks stitches were removed. Two patients develop superficial wound infection which was treated according to culture sensitivity. At six weeks, cast was removed and clinical and radiological assessment was done. weight bearing was allowed as per radiological and clinical signs of union. At 3 months again clinical and radiological assessment was done. Two patients had delayed union at this time and these were followed at two weeks intervals. one of them united at 18 weeks and other at 20 weeks. At six months further assessment was done and any complication noted including symptomatic hardware, which was observed in 13 patients. There were two case of wound site infection which was successfully treated with antibiotics. There was no case of non union in the present study [Table/Fig-3].
| Groups | Mean time of union (weeks) | Symptomatic hardware | Delayed union | Non union | *Total ankle range of motion (plantarflexion and dorsiflexion) | Wound infection |
|---|
| Group A | 10.25 | 3 (18.75%) | 0 | 0 | 57.81° | 0 |
| Group B | 11.14 | 5 (35.71%) | 1 (7.14%) | 0 | 55.71° | 1 (7.14%) |
| Group C | 10.80 | 5 (50%) | 1 (10%) | 0 | 55.50° | 1 (10%) |
One-way ANOVA test showed no significant difference with respect to time of union (p-value=0.406) and ankle range of motion (p-value=0.514); *ankle range of motion was taken one year postoperatively
Discussion
Medial malleolus fixation is important for stabilisation of ankle injuries. The aim of the present study was to assess the results of three methods of fixation for fixing medial malleolus fractures by taking into consideration fracture characteristics and quality of bone. Particular method of fixation was utilised depending on intraoperative findings and quality of bone. Large fragments were fixed using two screws. Sometimes the size of the fragment does not allow a second screw and in these cases, an additional k-wire was used to prevent the rotation of the fragment and to achieve more stable fixation. Small avulsed fragment, comminuted and highly osteoporotic fractures were fixed with tension band wiring. Tension band wiring have been found more effective in small avulsion fractures, osteoporotic fractures, and comminuted fractures [3,15].
In the present study, mean time of union was 10.25 weeks in group A. Mohammed AA et al., had mean time of union of 11.8 week in their study [16]. In Group C, the mean duration of union was 10.80 weeks in the present study. Kochai A et al., had 12 weeks [18].
There was no case of non union in the present series. Similar results are also reported by Barnes H et al., and Mandel J et al., in 2019 who used headless compression screws for fixation [7,14]. In the present study, 100% union rate was achieved probably because of strictly adhering to the basic technique of fixation by taking care of soft tissue and periosteum, anatomical reduction and stable fixation. This was also because different methods were used based on the fracture characteristics and quality of bone. In addition, patients with open fractures and multiple injuries were excluded from the study that could have negatively affected the results.
Implant related problems were the most frequent complication in the present study. The problem was seen in tension band wiring group and in most of the patients the prominent k wire ends were the cause. Georgiadis GM and White DB reported rate of 64% for implant-related complications in their series in 1995 [23]. Ostrum RF and Litsky AS on the other hand found 15% patients with hardware problem [8]. These patients have pain on the medial aspect of ankle and on examination, they had tenderness over the implant. These patients improved by removal of hardware once the fracture has healed.
Adhering to the basic technique of approach for medial malleolus fixation is essential as the soft tissue coverage is less which can lead to implant related problems after surgery [18]. Care should be taken not to remove much of periosteum and only few mm of periosteum should be removed adjacent to the fracture site to visualise the fracture reduction. Interposed soft tissue at the fracture site should be removed as this is a cause for non union of these fractures [24]. Comparison of various parameters of present study with previous other studies is given in [Table/Fig-4] [14,16,18].
Comparison of outcome of present study with previous studies. [14,16,18]
| S. No. | Author’s name and year | Place of the study | Sample size | Median age (years) | Mean time of union | Symptomatic hardware | Non union |
|---|
| Tension band wiring group |
| 1. | Mohammad AA et al., [16] (2016) | Iraq | 10 | 37 | 9.4 weeks | --- | 0 |
| 2. | Kochai A et al., [18] (2018) | Turkey | 26 | 38.23 | 10 weeks | 30% | 0 |
| 3. | Present study | Jammu and Kashmir, India | 10 | 36.50 | 10.80 weeks | 50% | 0 |
| Two screw fixation group |
| 1. | Kochai A et al., [18] (2018) | Turkey | 32 | 36.84 | 12 weeks | 34% | 0 |
| 2 | Mandel J et al., [14] (2019) | New York, USA | 149 | 49.20 | 3.84±2.54 months | --- | 0 |
| 3 | Present study | Jammu and Kashmir, India | 16 | 36 | 10.25 weeks | 18.75% | 0 |
Limitation(s)
Small sample size of the study group and fixation of the lateral column or syndesmosis was not taken into consideration while assessing the outcomes.
Conclusion(s)
Medial malleolus fixation is important for stability of the ankle joint and to achieve anatomical reduction to prevent possible complications. Based on the outcomes of the study, it can be concluded that all the three fixation methods used in this study achieved the union in comparable time duration. A particular method of fixation should be used by taking into consideration the type of fracture, size of the fragment, comminution and quality of the bone. In addition, meticulous care of soft tissue and periosteum should be taken at the time of surgery. However, further studies are needed in order to come to a final conclusion.
M: Male; F: Female
One-way ANOVA test showed no significant difference with respect to time of union (p-value=0.406) and ankle range of motion (p-value=0.514); *ankle range of motion was taken one year postoperatively
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 18, 2021
Manual Googling: Aug 19, 2021
iThenticate Software: Sep 04, 2021 (18%)
[1]. Juto H, Nilsson H, Morberg P, Epidemiology of adult ankle fractures: 1756 cases identified in Norrbotten county during 2009-2013 and classified according to AO/OTABMC Musculoskelet Disord 2018 19(1):44110.1186/s12891-018-2326-x30545314 [Google Scholar] [CrossRef] [PubMed]
[2]. Chaudhry S, Egol KA, Ankle injuries and fractures in the obese patientOrthop Clin North Am 2011 42(1):45-53.10.1016/j.ocl.2010.07.00321095434 [Google Scholar] [CrossRef] [PubMed]
[3]. Hasselman CT, Vogt MT, Stone KL, Cauley JA, Conti SF, Foot and ankle fractures in elderly white women. Incidence and risk factorsJ Bone Joint Surg Am 2003 85(5):820-24.10.2106/00004623-200305000-0000812728031 [Google Scholar] [CrossRef] [PubMed]
[4]. Strauss EJ, Egol KA, The management of ankle fractures in the elderlyInjury 2007 38(suppl 3):S02-09.10.1016/j.injury.2007.08.00517723786 [Google Scholar] [CrossRef] [PubMed]
[5]. Jaffe D, Christian MW, Weber A, Henn RF III, Incarceration of the posterior tibial tendon in an isolated comminuted medial malleolus fractureJ Foot Ankle Surg 2017 56(6):1312-15.10.1053/j.jfas.2017.05.01628697881 [Google Scholar] [CrossRef] [PubMed]
[6]. Earl M, Wayne J, Brodrick C, Vokshoor A, Adelaar R, Contribution of the deltoid ligament to ankle joint contact characteristics: a cadaver studyFoot Ankle Int 1996 17(6):317-24.10.1177/1071100796017006048791077 [Google Scholar] [CrossRef] [PubMed]
[7]. Barnes H, Cannada LK, Watson JT, A clinical evaluation of alternative fixation techniques for medial malleol fracturesInjury 2014 45(9):1365-67.10.1016/j.injury.2014.05.03125042063 [Google Scholar] [CrossRef] [PubMed]
[8]. Ostrum RF, Litsky AS, Tension band fixation of medial malleolus fracturesJ Orthop Trauma 1992 6(4):464-68.10.1097/00005131-199212000-000131494102 [Google Scholar] [CrossRef] [PubMed]
[9]. Ricci WM, Tornetta P, Borrelli J Jr, Lag screw fixation of medial malleolar fractures: A biomechanical, radiographic, and clinical comparison of unicortical partially threaded lag screws and bicortical fully threaded lag screwsJ Orthop Trauma 2012 26(10):602-06.10.1097/BOT.0b013e318240451222437423 [Google Scholar] [CrossRef] [PubMed]
[10]. Schiedts D, Fleurat E, Bouger D, Bastaraud H, Osteosynthesis of internal malleolar fracture by staplersRev Chir Orthop Reparatrice Appar Mot 1997 83(1):70-73. [Google Scholar]
[11]. SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS, Complication rates following open reduction and internal fixation of ankle fracturesJ Bone Joint Surg Am 2009 91(5):1042-49.10.2106/JBJS.H.0065319411451 [Google Scholar] [CrossRef] [PubMed]
[12]. Fowler TT, Pugh KJ, Litsky AS, Taylor BC, French BG, Medial malleolar fractures: a biomechanical study of fixation techniquesOrthopedics 2011 34(8):349-55.10.3928/01477447-20110627-0921815575 [Google Scholar] [CrossRef] [PubMed]
[13]. Pollard JD, Deyhim A, Rigby RB, Comparison of pullout strength between 3.5-mm fully threaded, bicortical screws and 4.0-mm partially threaded, cancellous screws in the fixation of medial malleolar fracturesJ Foot Ankle Surg 2010 49(3):248-52.10.1053/j.jfas.2010.02.00620362467 [Google Scholar] [CrossRef] [PubMed]
[14]. Mandel J, Behery O, Narayanan R, Konda SR, Egol KA, Single- vs 2-Screw Lag Fixation of the Medial Malleolus in Unstable Ankle FracturesFoot Ankle Int 2019 40(7):790-96.10.1177/107110071984099530971114 [Google Scholar] [CrossRef] [PubMed]
[15]. Johnson BA, Fallat LM, Comparison of tension band wire and cancellous bone screw fixation for medial malleolar fracturesJ Foot Ankle Surg 1997 36(4):284-89.10.1016/S1067-2516(97)80074-9 [Google Scholar] [CrossRef]
[16]. Mohammed AA, Abbas KA, Mawlood AS, A comparative study in fixation methods of medial malleolus fractures between tension bands wiring and screw fixationSpringer Plus 2016 5(1):04-09.10.1186/s40064-016-2155-z27186494 [Google Scholar] [CrossRef] [PubMed]
[17]. Shayaa S, Comparative study of operative fixation of fracture of medial malleolus by malleolar screw verses tension band wiringInt J Surg Sci 2020 4(4):157-63.10.33545/surgery.2020.v4.i4c.553 [Google Scholar] [CrossRef]
[18]. Kochai A, Turker M, Çicekli O, A comparative study of three commonly used fixation techniques for isolated medial malleolus fractureEklem Hastalik Cerrahisi 2018 29(2):104-09.10.5606/ehc.2018.6144930016610 [Google Scholar] [CrossRef] [PubMed]
[19]. World Medical AssociationDeclaration of Helsinki: Ethical Principles for Medical Research Involving Human SubjectsJAMA 2013 310(20):2191-94.10.1001/jama.2013.28105324141714 [Google Scholar] [CrossRef] [PubMed]
[20]. Hughes JL, Weber H, Willenegger H, Kuner EH, Evaluation of ankle fractures: Non operative and operative treatmentClin Orthop Relat Res 1979 138:111-19. [Google Scholar]
[21]. Loder RT, The influence of diabetes mellitus on the healing of closed fracturesClin Orthop Relat Res 1988 232(232):210-16.10.1097/00003086-198807000-00028 [Google Scholar] [CrossRef]
[22]. Grimston SK, Nigg BM, Hanley DA, Engsberg JR, Differences in ankle joint complex range of motion as a function of ageFoot Ankle Int 1993 14(4):215-22.10.1177/1071100793014004078359768 [Google Scholar] [CrossRef] [PubMed]
[23]. Georgiadis GM, White DB, Modified tension band wiring of medial malleolar ankle fracturesFoot Ankle Int 1995 16(2):64-68.10.1177/1071100795016002027767448 [Google Scholar] [CrossRef] [PubMed]
[24]. Muller GM, Fractures of internal malleolusBr Med J 1945 2(4418):32010.1136/bmj.2.4418.32020786271 [Google Scholar] [CrossRef] [PubMed]