The surgical procedure pancreaticoduodenectomy is popularly known as Whipple’s operation. It is performed most commonly for neoplasms of periampullary region which include those arising from ampulla of Vater, head of pancreas, distal common bile duct and duodenum. Patients of periampullary cancers usually present with jaundice due to obstruction by periampullary mass [1]. Imaging modalities like ultrasound, Computed Tomography (CT) scans as well as invasive procedures like Endoscopic Retrograde Cholangio-Pancreaticography (ERCP) coupled with biopsy of the lesion are principal investigations apart from routine haematological parameters. Resectibility of the tumour is determined considering these investigations along with co-morbid factors like diabetes mellitus, hypertension, etc. Irrespective of the origin Whipple’s operation remains mainstay of treatment for periampullary neoplasms, as there is no effective alternative therapy [2].
Moreover, periampullary region is complex in its anatomy and histology. The preoperative clinical findings, imaging studies as well as intraoperative findings do not permit the identification of the specific site of origin of periampullary tumour. To evaluate origin of the tumour, a thorough gross examination and exhaustive histopathological examination of the resected Whipple’s specimen is mandatory [3]. Common perioperative complications of Whipple operation are biliary leak and delayed gastric emptying. There are multiple factors which can be correlated well with perioperative morbidity and mortality and are responsible for different biological behaviour of periampullary cancers [4]. These factors include clinical profile of patient, imaging studies, preoperative biopsy, site of origin, size, type, grade, differentiation, {Tumour (T), Nodes (N), Metastasis (M)} staging staging lymphovascular and perineural invasion positive resection margins of the tumour and lymph node metastasis [5]. Review of literature says that tumour arising from head of pancreas and distal common bile ducts have aggressive behaviour in the form of increased perioperative morbidity and mortality.
Localised pancreatic carcinoma patient have no recognisable symptoms, thus presenting late, mostly after metastasis to different organs. Therefore, the present study compared tumour arising from ampulla of Vater, head of pancreas, distal common bile duct and duodenum with respect to demographic profile, clinical features, biochemical investigations, gross morphology and histopathological features of the tumour. Clinicopathological concordance been made to compare biological behaviour of intestinal and pacreaticobiliary neoplasms with respect to outcome of the surgery.
Materials and Methods
This retrospective study was conducted in total 155 patients who had undergone Whipple’s operation over a period of ten years from January 2009 to December 2019 at a Indira Gandhi Government Medical College and Hospital, Nagpur, Maharastra in Central India. The study was conducted over a period of two years from July 2018 to July 2020.
Inclusion and Exclusion criteria: All cases which showed malignant tumour on histopathological examination were included in study, while those cases showing benign tumour and other lesion of pancreas on histopathological examination were excluded from study.
The demographic profile along with clinical details, preoperative investigations, intraoperative findings and perioperative outcome of the Whipple’s operation were obtained from Medical Record Office. Clinical details of patients taken into consideration were age, sex, presenting complaints, clinical signs. Preoperative investigations studied were complete blood count, liver function tests, Cancer Antigen 19-9 (CA 19-9) levels, ERCP, biopsy, Fine Needle Aspiration Cytology (FNAC if done), ultrasound examination and CT scan.
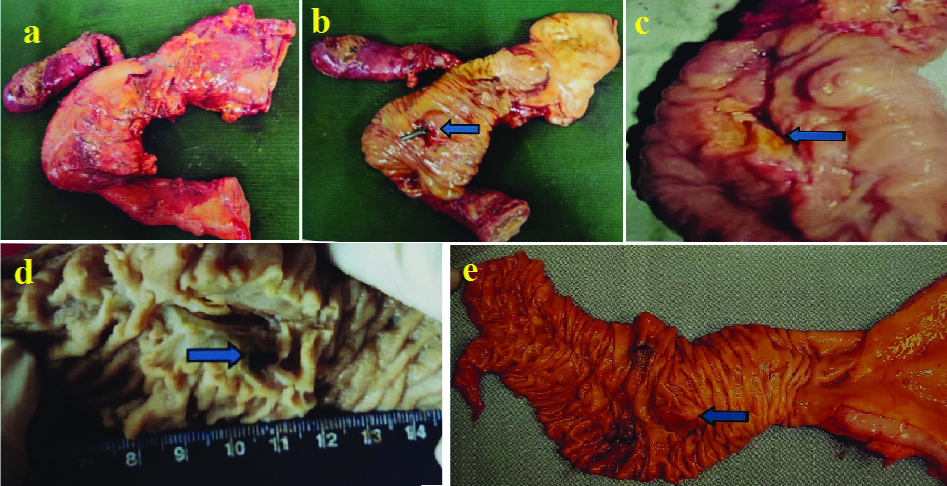
Detailed grossing of Whipple’s resected specimen was done according to standard protocol as depicted in [Table/Fig-1].
a) Whipple’s specimen showing gall bladder, cystic duct and parts of stomach, duodenum and pancreas, b) Mucosal surface of the same specimen showing polypoidal mass at stent site (arrow), c) Ulcerative growth at the periampullary region (arrow), d) Mucosal surface of Whipple’s specimen with slight bulge of ampulla and impacted stone at distal CBD (arrow), e) Shows 1.5×1.5 cm nodular growth at the ampulla (arrow)
Following sections had been submitted for processing and staining as per routine procedure:
Minimum four sections of tumour (with ampulla, with CBD, with duodenum and with head of pancreas).
Resection margins (proximal, distal, CBD, pancreatic).
Head, body and neck of gall bladder (if received).
Lymph nodes dissected.
Separately sent lymph nodes (if any)
The H&E stained slides were reviewed and various parameters were studied like presence or absence of the tumour, site of origin of tumour (ampulla/head of pancreas/distal common bile duct/duodenum), histological type (adenocarcinoma/neuroendocrine/lymphoma etc.,), differentiation (well/ moderate/ poor), depth of invasion, LVI (yes/no), perineural infiltration (yes/no), lymph node status metastasis (yes/no), resection margin status (involved/not involved) and TNM staging. Perioperative complications as well as follow-up (if available) were studied. The postoperative follow-up of minimum 30 days was kept of all patients included in the study group.
Statistical Analysis
Statistical analysis was carried out using Chi-Square test. The p-value <0.05 was considered statistically significant. The Statistical Package for Social Science (SPSS) version 20.0 was used for data analysis.
Results
Out of total 155 patients, maximum numbers of cases 151 (97.41%) were of malignant tumours in the periampullary region while tumour was absent in two cases had no tumour, one case was of benign adenoma of ampulla and one was of type 1 choledochal cyst. Therefore, only 151 cases with presence of tumour were taken into consideration. Tumours from ampulla were most common (101/151) followed by those from Common Bile Duct (CBD) (22/151) and pancreas (22/151) while duodenum was the least common site with 6/151 cases.
The maximum number of cases were found in the age group between 41-70 years i.e., 112 (74.17%), (p-value=0.108). There was higher incidence of tumours observed in males than females, (p-value=0.601) as shown in [Table/Fig-2].
Age and sex distribution according to tumour site.
| Variables | Tumour site | Total |
|---|
| Age group (years) | Ampulla | CBD | Pancreas | Duodenum |
|---|
| ≤30 | 7 (6.9%) | 0 | 1 (4.5%) | 1 (16.7%) | 9 (5.96%) |
| ≤31-40 | 9 (8.9%) | 4 (18.2%) | 5 (22.7%) | 0 | 18 (11.92%) |
| 41-50 | 29 (28.7%) | 4 (18.2%) | 5 (22.7%) | 0 | 38 (25.17%) |
| 51-60 | 33 (32.7%) | 5 (22.7%) | 5 (22.7%) | 1 (17%) | 44 (29.14%) |
| 61-70 | 14 (13.9%) | 7 (31.8%) | 5 (22.7%) | 4 (67%) | 30 (19.87%) |
| >70 | 9 (8.9%) | 2 (9.1%) | 1 (4.5%) | 0 | 12 (7.95%) |
| Sex |
| Male | 60 (59.4%) | 15 (68.2%) | 13 (59.1%) | 5 (83.3%) | 93 (61.6%) |
| Female | 41 (40.6%) | 7 (31.8%) | 9 (40.9%) | 1 (16.7%) | 58 (38.4%) |
| Total | 101 | 22 | 22 | 6 | 151 |
CBD: Common bile duct
As seen in [Table/Fig-3], the major presenting complaint was Yellowish Discolouration of Sclera (YDS) and Yellowish Discolouration of Urine (YDU) irrespective of site except in pancreatic cancers, where majority of cases presented with pain in abdomen. Abdominal lump was the major clinical finding in carcinomas of head of pancreas while jaundice was the major clinical sign at other sites as shown in [Table/Fig-3].
Distribution of chief complaints and signs according to tumour site.
| Chief complaints | Tumour site | Total |
|---|
| Ampulla | CBD | Pancreas | Duodenum |
|---|
| Pain in abdomen | 8 (7.9%) | 2 (9.1%) | 16 (72.7%) | 1 (16.7%) | 27 (17.9%) |
| YDS/YDU | 93 (92.1%) | 20 (90.9%) | 6 (27.3%) | 5 (83.3%) | 124 (82.1%) |
| p-value | 0.001 (significant) | |
| Signs |
| Abdominal lump | 8 (7.9%) | 2 (9.1%) | 15 (68.2%) | 1 (16.7%) | 26 (17.2%) |
| Jaundice | 85 (84.2%) | 20 (90.9%) | 7 (31.8%) | 5 (83.3%) | 117 (77.5%) |
| Pallor, jaundice | 8 (7.9%) | 0 | 0 | 0 | 8 (5.3%) |
| p-value | <0.001 (significant) | |
Values are represented in number and percentage; p-value <0.05 was considered statistically significant; Analysis was carried out using Chi-square test; YDS: Yellowish discolouration of sclera; YDU: Yellowish discolouration of urine; CBD: Common bile duct
The CA 19-9 levels was available in 102 cases out of 151 cases and raised levels of CA 19-9 observed in 96 (96/102= 94.1%) cases irrespective of site, (ampulla was 59, CBD was 14, pancreas was 21 and duodenum=2; p-value=0.817). Adenocarcinoma (145, 96.02%) was the most common histological type of malignant tumour followed by neuroendocrine carcinomas 3 (1.9%). Incidence of mucinous adenocarcinoma, signet ring cell adenocarcinoma and adenocarcinoma with squamous differentiation was found to be 0.7% each.
Histopathologically, maximum number of cases (116, 76.8%) were Moderately Differentiated (MD) and were seen in ampullary and pancreatic carcinomas while Well Differentiated (WD) carcinomas were seen in (25, 16.6%) cases mainly in the ampulla and duodenum, (p-value=0.060).
A 86.4% (19/22) of pancreatic cancer showed presence of LVI while CBD tumours showed presence in 59.1% (13/22) cases. The LVI was seen in 32.7% (33/101) and 33.3% (2/6) cases of ampullary and duodenal carcinomas respectively, (p-value= 0.001). Perineural invasion was significantly high 90.9% (20/22) in pancreatic cancers as compared to other sites. This was followed by carcinoma of the CBD 63.6% (14/22), (p-value=0.001). Lymph node metastasis was seen in 77.3% (17/22) and 45.5% (10/22) cases of pancreatic and CBD cancers respectively which was found to be statistically significant, (p-value=0.001). Ampullary carcinomas showed only 8.9% (9/101) cases with lymph node metastasis.
Very few cases of positive resection margin were seen in ampulla 1.98% (2/101), CBD 13.6% (3/22) and duodenum 16.7% (1/6) as compared to pancreatic carcinomas 40.9% (9/22), (p-value=0.001).
Maximum numbers of stage 2 cancers 81.82% (18/22) were seen in pancreas followed by duodenum 50% (3/6). Ampulla and CBD showed slightly higher incidence of stage 1 disease i.e., 55.4% (56/101) and 54.6% (12/22) cases respectively. None of the presented cases showed stage 4 disease, (p-value=0.001) [Table/Fig-4].
Various parameters studied after reviewing H&E-stained slides.
| Parameters | Tumour site | Total |
|---|
| Ampulla | CBD | Pancreas | Duodenum |
|---|
| Histological grades of periampullary carcinomas | WD | 18 (17.8%) | 3 (13.6%) | 1 (4.6%) | 3 (50.0%) | 25 (16.6%) |
| MD | 77 (76.2%) | 19 (86.4%) | 18 (81.8%) | 2 (33.3%) | 116 (76.8%) |
| PD | 6 (6.0%) | 0 (0.0%) | 3 (13.6%) | 1 (16.7%) | 10 (6.6%) |
| LVI | Yes | 33 (32.7%) | 13 (59.1%) | 19 (86.4%) | 2 (33.3%) | 67 (44.4%) |
| No | 68 (67.3%) | 9 (40.9%) | 3 (13.6%) | 4 (66.7%) | 84 (55.6%) |
| PNI | Yes | 38 (37.6%) | 14 (63.6%) | 20 (90.9%) | 1 (16.7%) | 73 (48.3%) |
| No | 63 (62.4%) | 8 (36.4%) | 2 (9.1%) | 5 (83.3%) | 78 (51.7%) |
| LN mets | Yes | 9 (8.9%) | 10 (45.5%) | 17 (77.3%) | 2 (33.3%) | 38 (25.2%) |
| No | 92 (91.1%) | 12 (54.5%) | 5 (22.7%) | 4 (66.7%) | 113 (74.8%) |
| Resection margin involved | Yes | 2 (1.98%) | 3 (13.6%) | 9 (40.9%) | 1 (16.7%) | 15 (9.9%) |
| No | 99 (98.02%) | 19 (86.4%) | 13 (59.1%) | 5 (83.3%) | 136 (90.1%) |
| TNM staging | Stage I | 56 (55.4%) | 12 (54.6%) | 1 (4.54%) | 2 (33.3%) | 71 (47%) |
| Stage II | 42 (41.6%) | 9 (40.9%) | 18 (81.82%) | 3 (50.0%) | 72 (47.7%) |
| Stage III | 3 (3.0%) | 1 (4.5%) | 3 (13.64%) | 1 (16.7%) | 8 (5.3% |
LVI: Lymphovascular invasion; PNI: Perineural infiltration; LN mets: Llymph node metastasis;
MD: Moderately differentiated; WD: Well differentiated; PD: Partially differentiated;
CBD: Common bile duct
More postoperative complications were in CBD 31.8% (7/22) and pancreatic 36.4% (8/22) cancers as compared to ampullary 15.8% (16/101) and duodena 16.7% (1/6) cancers. In the perioperative period, most of the cases (6/7= 85.7%) of CBD cancer were expired followed by cases of pancreatic 2 (25%) and ampullary cancers 4 (25%), [Table/Fig-5]. There was only one complicated case of duodenal cancer without mortality. None of the cases expired intraoperatively. The H&E stained slides were reviewed and various parameters were studied like presence or absence of the tumour [Table/Fig-6].
Distribution of postoperative complications and outcome of complications (morbidity) according to tumour site.
| Complications (n=151) | Tumour site | Total |
|---|
| Ampulla | CBD | Pancreas | Duodenum |
|---|
| Yes | 16 (15.8%) | 7 (31.8%) | 8 (36.4%) | 1 (16.7%) | 32 (21.2%) |
| No | 85 (84.2%) | 15 (68.2%) | 14 (63.6%) | 5 (83.3%) | 119 (78.8%) |
| p-value | 0.097 (not significant) | |
| Outcome (n=32) |
| Alive | 12 (75.0%) | 1 (14.3%) | 6 (75.0%) | 1 (100%) | 20 (62.5%) |
| Expired | 4 (25.0%) | 6 (85.7%) | 2 (25.0%) | 0 | 12 (37.5%) |
| p-value | 0.027 (significant) | |
Values are represented in number and percentage; p-value <0.05 was considered statistically significant; Analysis was carried out using Chi-square test
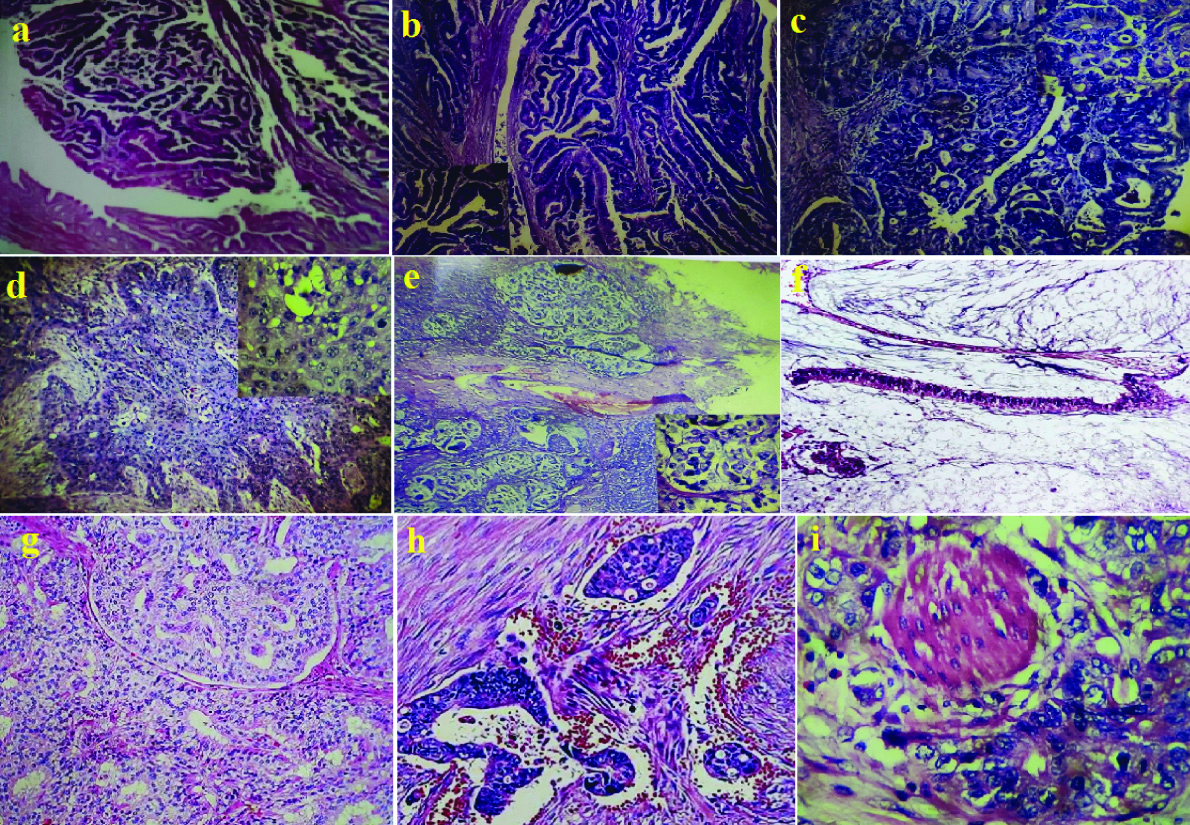
a) Moderately Differentiated (MD) adenocarcinoma arising from CBD with zone of transformation (H&E,40X); b) Well Differentiated (WD) adenocarcinoma (intestinal type) arising from ampulla (H&E,40X); c) Moderately differentiated adenocarcinoma of ampulla (H&E,40X); d) Adenocarcinoma with squamous differentiation (H&E,40X); e) Signet ring cell adenocarcinoma of ampulla (H&E,40X); f) Mucinous adenocarcinoma of the ampulla (H&E,40X); g) Neuroendocrine tumour of duodenum, (H&E,40X) h) Lymphovascular invasion in a case of adenocarcinoma (H&E,40X); i) Perineural invasion in a case of adenocarcinoma of ampulla (H&E,40X).
Discussion
In present study, the periampullary carcinomas were most commonly seen in males in age group of 51-60 years with a mean age of 53 years which is comparable with the study done by Chan C et al., and Cameron JL et al., [6,7]. Obstructive jaundice was the most common presentation of all patients followed by pain in abdomen, weight loss and anorexia etc. When compared with site of origin, pancreatic cancer was more likely to present with abdominal pain (72.7%). Tumours arising from ampulla had icterus as chief presenting complaint observed in 92.1% cases. Patients with tumours arising from duodenum and distal common bile duct also presented with icterus in 83.3% and 92.1% cases, respectively. These findings are comparable with the study done by Chauhan A et al., [8].
The tumour marker like CA 19-9 was available in 102 cases and it was raised in 96 (94.1%) cases. However, it was raised in all 21 cases of pancreatic cancers (100%), two cases of duodenal cancers (100%) as well as 14 (93.3%) cases of distal cholangicarcinomas. A 92.2% of ampullary cancers had increased level of preoperative CA19-9. These findings are correlated with the previous studies [9,10]. Ultrasound examination report was available in 134/155 cases and showed periampullary mass with grossly dilated distal common bile duct and pancreatic duct with intrahepatic biliary dilatations in majority of cases. The CT scan report was available in 137/155 cases which confirmed obstruction by periamputary mass causing abrupt cut-off of common bile duct and pancreatic duct. These investigations could not confirm the real site of origin of tumour in previous as well as present study. The ERCP studies carried out in 80/155 cases also showed periampullary mass, preoperative stenting done in selected cases. Biopsy of periampullary mass done in 133 cases showed invasive adenocarcinomas in 124 cases. There were two cases of signet ring cell adenocarcinoma while one case each of papillary adenocarcinoma, poorly differentiated adenocarcinoma versus neuroendocrine tumour, benign adenomatous lesion and chronic inflammation. Two cases were having suspicion of malignancy and one case had no tumour on biopsy.
The most common site of origin of periampullary tumour was ampulla followed by distal CBD, pancreas and duodenum. This result is in accordance with the study done by Chan C et al., and Tarazi RY et al., [6,11]. A total of 67 cases had dilated CBD with diameter more than 0.8 cm. Two of cases in the present study showed CBD diameter of 1.8 cm and 1.5 cm, respectively. The most commonly observed gross morphological pattern was infiltrative followed by polypoidal, ulcerative and nodular growth. The most common histological type was adenocarcinoma followed by neuroendocrine tumour which is similar to previous studies [12,13]. The overall median size of the tumour in Whipple’s specimen was 1.44 cm2. Tumours arising from duodenal mucosa were larger in size (5.1 cm2) while amputary carcinomas were smallest (1 cm2). Tumours arising from pancreas and CBD had median size of 3.1 cm2 and 2.2 cm2, respectively. These observations are similar to study of Chan C et al., Michelassi F et al., and Yeo CJ et al., [6,13,14].
Moderate differentiation was most commonly observed histological grade in periampullary carcinomas which is correlated with various studies [14,15]. Perineural and lymphovascular infiltration was seen more commonly in pancreatic cancers, this is comparable with the study done by Hatzaras I et al., [10]. Lymph node metastasis was significantly high in pancreatic cancers followed by distal cholangiocarcinomas, these findings comparable with the study done by Michelassi F et al., and Yeo CJ et al., both these studies concluded aggressive behaviour of pancreatic cancers as seen in present study [13,14]. We had no case of macroscopic tumour extension to any of the resection margins (R2). The TNM tumour staging system applied in the present study of 151 cases of pancreaticoduodenectomies revealed 47% cases with stage 1 and stage 2 disease each and 5% cases of stage 3. However, there was no case of stage 4 disease at any of the sites. Similar finding reported in other studies [16-18].
None of the cases in the present, had intraoperative complications while perioperative complications were seen in 32 patients. The most common complications were biliary leak followed by wound infection, pancreatic fistula, bronchopneumonia, Acute Respiratory Distress Syndrome (ARDS), pus in lesser sac, anastomotic leak, bleeding, burst abdomen, gastric outlet obstruction, septicaemia and acute renal failure. Three patients developed respiratory complaints in the form of breathlessness and cough and all of them died and autopsies were performed where final cause of death was given as bronchopneumonia. There was another group of three patients having acute respiratory complaints, all of them expired and final cause of death after autopsies performed was given as ARDS. There were two cases with complication of pus formation in the lesser sac as a result of surgery. The first one was a 46-year-old female patient with infiltrative growth at ampulla showing MD adenocarcinomas. Despite putting her on higher intravenous antibiotics, the patient expired on postoperative day 6. The second case with pus formation in lesser sac was of 63-year-old male having infiltrative growth of pancreas and showing features of poorly differentiated adenocarcinoma with perineural invasion. The patient expired on postoperative day 17. Anastomotic leak was seen in two cases, both of them were adenocarcinomas arising from distal CBD showing lymphovascular and perineural invasion. The first case of 70-year-old male, a known diabetic had infiltrative growth and microscopic involvement of CBD resection margin by tumour cells (R1 resection status). The patient expired on postoperative day 4. Second case with ulcerative growth of distal CBD of a 60-year-old male patient had nodal metastasis. The patent expired on postoperative day 5. A 45-year-old female patient of MD adenocarcinoma from distal CBD developed features of septicaemia and breathlessness. The patient died on postoperative day 15 the postmortem examination of which showed final cause of death as septicaemia complicated by ARDS and bronchopneumonia. Thus, overall perioperative mortality in the study was 7.9% accounting for 12 deaths, only two of them were females. Distal cholangiocarcinoma was found to be more aggressive in the form of perioperative mortality followed by pancreatic and ampullary carcinoma.
According to review of literature distal CBD cancers have less aggressive biological behaviour than pancreatic carcinomas, but the present study shows that histomorphological factors like perineural or LVI, nodal metastasis may have impact on immediate postoperative period of these cancers. Other factors like age, sex, differentiation, TNM staging were found to be equally associated with adenocarcinomas arising from the four sites of origin as described.
Limitation(s)
Long term follow-up of cases was not possible in this study as majority of patients were defaulters or referred to outside speciality oncology services for follow-up. Also, lack of awareness, socio-economic status plays a role in poor follow-up.
Conclusion(s)
Whipple’s operation is a routine procedure performed at our institute for tumours of periampullary region which are often malignant. Whipple procedure is associated with a unique set of common complications and also continues to be associated with considerable morbidity. Knowledge of the complications as well as a detailed understanding of normal postoperative anatomy helps in the arriving at the correct diagnosis. With careful patient selection, Whipple procedure can be performed safely. Long term survival in patients with periampullary adenocarcinoma can be predicted by preoperative laboratory values, intraoperative factors, and pathologic findings.
CBD: Common bile duct
Values are represented in number and percentage; p-value <0.05 was considered statistically significant; Analysis was carried out using Chi-square test; YDS: Yellowish discolouration of sclera; YDU: Yellowish discolouration of urine; CBD: Common bile duct
LVI: Lymphovascular invasion; PNI: Perineural infiltration; LN mets: Llymph node metastasis;
MD: Moderately differentiated; WD: Well differentiated; PD: Partially differentiated;
CBD: Common bile duct
Values are represented in number and percentage; p-value <0.05 was considered statistically significant; Analysis was carried out using Chi-square test