Extracalvarial Porocarcinoma- A Rare Case Report
Satyam Singh1, Suhas Jajoo2, Abhishek Vaijnath Chaudhari3, Samarth Shukla4, Sourya Acharya5
1 Medical Intern, Department of Medicine, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
2 Professor, Department of Surgery, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
3 Junior Resident, Deparment of Surgery, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
4 Professor, Department of Pathology, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
5 Professor, Department of Medicine, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Satyam Singh, Medical Intern, Department of Medicine, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
E-mail: singhsatyam55@gmail.com
Eccrine Porocarcinoma (EPC) is a very rare malignant neoplasm of skin. It usually emerges from the ductal parts of sweat glands. It is seen mostly between the age group of 60 to 80 years with a female preponderance. Several cases of EPC have been reported in medical literature till date. Though, it rarely presents with distant metastasis, still evidences of metastasis to organs like lung, retroperitoneum, breast, urinary bladder and ovaries have been reported. Conventionally, it arises de novo, and may develop on sites of long standing eccrine poroma. Several unusual sites like trunk, head, face, eyelids, upper limbs, and scrotum have been reported; though lower extremities are the most common site of origin. Locoregional recurrence and metastasis have also been reported. Histopathological documentation of mitoses, lymphovascular invasion and measurement of tumour depth predicts adverse prognosis in EPC. Earlier, eccrine adenocarcinoma or malignant eccrine poroma terminology were used. As far as clinical presentation is concerned, the EPC is usually symptomless to begin with, which further ulcerates and may become aching and irritable. From a clinicopathological perspective the importance of the tumour lies in its early correct diagnosis, awareness of the close differentials, adequate surgery and most importantly clearance of surgical margins and adjuvant radiotherapy are mandatory decisions to prevent the high local recurrence. The basis of management involves wide local excision with clear margin. The following case, a 42-year-old male presented with an ulcerated mass on the scalp, which on further evaluation was diagnosed as an EPC of the scalp after histopathologic confirmation. The patient was treated with local wide excision with clear margin and was referred for radiotherapy.
Malignant neoplasms, Plaque, Scalp, Ulcerated nodule, Wide local excision
Case Report
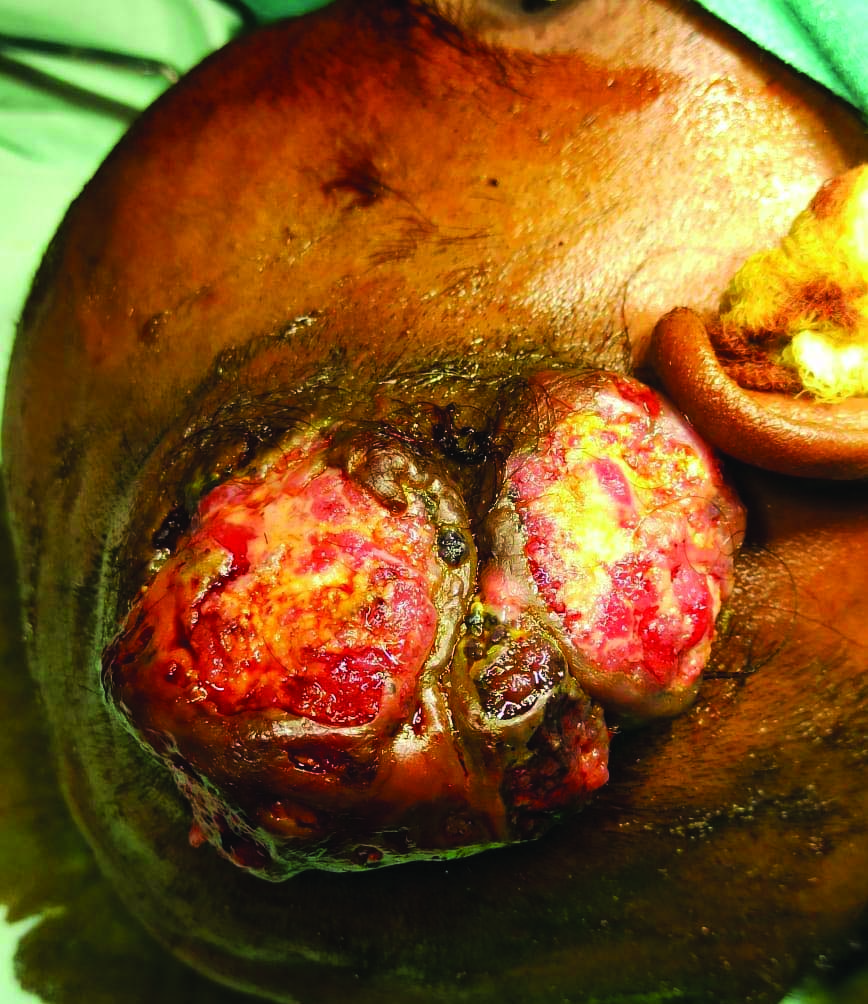
A 42-year-old male presented to Surgery Outpatient Department (OPD) with complaints of growth over right side of head since two years. On clinical examination, ulcerated mass of size approximately 8×8×6 cm over the right temporoparietal region with slough and discharge present [Table/Fig-1]. No lymph node was palpated at cervical, preauricular and postauricular area. No significant past history was present.
Ulcerated mass of size approximately 8×8 cm over right temporoparietal region with slough and discharge present.
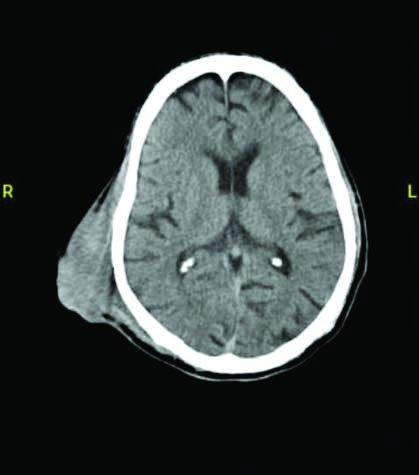
On further radiological investigations, Computed Tomography (CT) of head suggested extracalvarial heterogeneously enhancing soft tissue density lesion with areas of necrosis and a calcific foci within suggestive of neoplastic aetiology [Table/Fig-2]. Punch biopsy from the growth was sent for histopathological examination which showed hypertrophied atypical squamous epithelial linings, papillary dermis showed two to three islands of atypical basal cells with pigmentation showing peripheral palisading and cleftings suggestive of basal cell carcinoma of pigmented variety. Differential diagnosis include angiosarcoma over right side of scalp, haemangioma, basal cell carcinoma, Eccrine Porocarcinoma (EPC) was made. Patient underwent wide local excision of growth over right side of head along with margins. Defect was then reconstructed with rotatory flap over scalp and split skin grafting.
Computed Tomography (CT) Head suggested extracalvarial heterogeneously enhancing soft tissue density lesion with areas of necrosis and calcific foci.
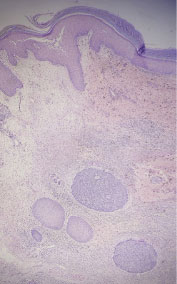
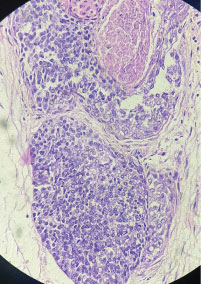
Excised specimen was sent for histopathological evaluation. Multiple sections were examined from the tumour mass [Table/Fig-3]. The histopathological sections of Hematoxylin and Eosin stain (H&E) stained slides showed unremarkable squamous epithelial lining, papillary dermis shows lobules and nests of atypical adnexal cells comprising of eosinophilic as well as basaloid cells, lobules were seen extending into the reticular dermis, at places the lobular masses underwent central necrosis forming cystic cavities, histopathological features were suggestive of porocarcinoma. It also showed lymphovascular emboli and stromal invasion [Table/Fig-4,5].
Section from the gross excised mass shows size of 8×8×6 cm, the mass appears lobulated to nodular with skin attached and superficial ulceration, on cut section the mass appears predominantly solid with areas of haemorrhage and sloughing at places.

On microscopic analysis: H&E stained slide 4X view shows unremarkable epidermis with dermis showing evidence of malignant adnexal epithelial cells arranged in lobules separated by fibrous septae.
H&E stained slide 40X view shows malignant epithelial adnexal cells arranged in lobules are separated by fibrous septae; few lobules showing central necrosis; cells are cuboidal with moderate pale cytoplasm and vesicular nuclei; occasional cells showing one to two nucleoli.
Further considering the malignant potential of the tumour and the site of origin the surgical oncologist advised localised radiotherapy, patient has undergone the recommend cycle and dosage of radiotherapy and on the first follow-up after one month, the site appeared to be healing and unremarkable.
Discussion
The EPC is a rare tumour of skin evolve from intra-epidermal portion of sweat gland constituting 0.005-0.01% of all tumours of skin [1]. This tumour was the first malignant tumour arising from acrosyringium and initially coined as epidermotropic eccrine carcinoma [2]. Such tumour is often reported in middle and old age with average age around 67 years and woman are more prone to it [3-5].
Porocarcinoma is an infrequent carcinoma emerges from inner part of sweat gland which was first described in 1963 by Pinkus and Mehregan named “Epidermotropic eccrine carcinoma” and later Mishisma and Moriko introduced term “EPC” in 1969 [6,7]. It occurs late in adult life and in both sexes with female preponderance [3,5]. Lower extremities are the most usual site followed by trunk, upper extremity, head and neck [7]. The most common presentation is a mass or nodule which may be ulcerated, become itchy and may bleed on touch. It rarely occurs in scalp, face, ear, eye lid and genitalia. In the present case, it was an ulcerated mass of size approximately 8x8 cm over Right temporoparietal region of scalp with discharge present. Differential diagnosis considered were Angiosarcoma over right side of scalp, Haemangioma, Basal cell carcinoma, EPC. Clinically, it was diagnosed as angiosarcoma over right side of scalp.
Histopathological features of EPC show intra-epidermal nests or cords of polygonal anaplastic cells invading downwards into dermis and subcutaneous tissue. The neoplastic cells exhibit clear cytoplasm, large hyperchromatic nuclei and nucleolar prominence. Persistent mitosis and necrosis are also visible. The chance of recovery from EPC depends on: (a) lymph vascular invasion; (b) tumour margin status after resection; (c) mitotic count (>14/HPF); (d) depth of invasion in deeper tissue (>7 mm) [7,8]. All of the above features are poor prognostic factors.
Present case showed classical microscopic characteristics of EPC including dermal invasion, features of necrosis along with mitotic activity. The histopathological differential diagnosis that falls into the features described usually is trabecular carcinoma, Merkel cell carcinoma and metastatic adenocarcinomas [4]. Metastatic adenocarcinomas in this scenario were ruled out because of the absence of classical features of acinar and glandular pattern of tumour cells with squamous hyperplasia of the epithelium which was absent in this case [9]. Trabecular carcinoma and Merkel cell carcinoma shows trabecular arrangement with typical nuclear characteristics of fine granular chromatin, nuclear moulding, fragmentation and abundant mitosis which were absent in the present case [7]. Sometimes, the tumour cells of eccrine poroma may show low grade cytological atypia but infiltrative growth pattern, necrosis and frequent mitosis are usually not seen. Neoplastic cells of porocarcinoma demonstrate PAS reactive, diastase labile glycogen positivity in their cytoplasm [1]. When the microscopic features are not confirmatory, then immunohistochemical positivity for Carcinoembryonic Antigen (CEA), Epithelial Membrane Antigen (EMA), Cytokeratins (CK)-7 and negative S-100 and CK-20 aid in confirming the diagnosis [1,3,4,10,11]. Newer markers like Ki-67 can also predict recurrence and metastasis [12]. In rare instances other imaging modalities like Contrast Enhanced Computed Tomography (CECT), Fluorodeoxyglucose -Positron Emission Tomography (FDG-PET) and endoscopic examination may become mandatory for identifying the secondaries in metastatic porocarcinomas [13].
Kurashige Y et al., conducted a study which included eight patients with porocarcinoma. The mean age of patients were 72.6 years, six were male patients. The duration of growth ranged from four months to five years. Only one case had metastasis which was treated with adjuvant radiotherapy and chemotherapy after surgery. All cases survived till follow-up [14].
Management of EPC is wide local excision or Moh’s micrographic surgery with microscopic certification of free margin [1,3,6,7,15]. In case of localised lymph node inclusion, lymph node dissection should be think of. In comparison to radiotherapy, chemotherapy is appropriate and productive for treatment of metastatic lesions [1,3]. Adjuvant radiotherapy helps to decrease the chances of local recurrence.
The novelty of the present case was based on the fact that it was not only a rarity but also because of the atypical site of presentation as well as its close resemblance with other benign as well as malignant epithelial and adnexal tumour counterparts.
Conclusion(s)
Extracalvarial Porocarcinoma of scalp is an infrequent malignant adnexal tumour. The treating surgeon and the surgical pathologist should keep the differentials of malignant adnexal tumours in mind and make it a point to distinguish such tumours form closely resembling pure epithelial tumours of skin as well as identify the neoplastic potential of these tumours to avoid recurrence. Regional excision with negative margin forms the basis of treatment. This case was a typical model of the above diagnosed infrequent neoplasm and highlights the necessity of proper diagnosis of the lesion in the evaluation of any exophytic neoplasm of scalp.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 25, 2021
Manual Googling: Jul 31, 2021
iThenticate Software: Sep 14, 2021 (17%)
[1]. Fung YP, Eccrine porocarcinoma of the faceHong Kong Dermatol Venereoly Bul 1999 7(2):72-74. [Google Scholar]
[2]. Asghar HA, Mahmood H, Faheem M, Rizvi S, Khan KA, Irfan J, Porocarcinoma: A rare sweat gland malignancyJ Col Phys Surgeon Pak 2009 19(6):389-90. [Google Scholar]
[3]. Bhat W, Akhtar S, Khotwal A, Platt AJ, Primary eccrine porocarcinoma of the finger with transit forearm and axillary metastasisAnn Plast Surg 2011 66(4):344-46.10.1097/SAP.0b013e3181e35c8d21042176 [Google Scholar] [CrossRef] [PubMed]
[4]. Song SS, Wu Lee W, Hamman MS, Jiang SI, MOHS micrographic surgery for eccrine porocarcinomaDermatol Surg 2015 41(3):301-06.10.1097/DSS.000000000000028625742554 [Google Scholar] [CrossRef] [PubMed]
[5]. Bolognia JL, Jorizzo JL, Schaffer JV, Dermatology 2012 3rd editionPhiladelphiaElsevier Saunders:539-544. [Google Scholar]
[6]. Pinkus H, Mehregan AH, Epidermotropic eccrine carcinoma: A case combining features of eccrine poroma and Paget’s dermatosisArchives of Dermatology 1963 88(5):597-606.10.1001/archderm.1963.0159023010501514060075 [Google Scholar] [CrossRef] [PubMed]
[7]. Mishima Y, Morioka S, Oncogenic differentiation of the intraepidermal eccrine sweat duct: eccrine poroma, poroepithelioma and porocarcinomaDermatology 1969 138(4):238-50.10.1159/0002539895771637 [Google Scholar] [CrossRef] [PubMed]
[8]. Melgandi W, Benson R, Hakin A, Bhasker S, Porocarcinoma scalp with high risk features treated with surgery and adjuvant radiotherapy: A case report and review of literatureJ Egypt Natl Canc Inst 2016 28(3):195-98.10.1016/j.jnci.2016.05.00427302529 [Google Scholar] [CrossRef] [PubMed]
[9]. Rana RE, Verma SS, Puri VA, Baliarsing AS, Case Report-Sweat gland tumour (Eccrine Porocarcinoma) of scalp: A rare tumourIndian J Plast Surg 2005 38(1):51-53.10.4103/0970-0358.16498 [Google Scholar] [CrossRef]
[10]. Masamatti SS, Narasimha A, Bhat A, Chowdappa V, Eccrine porocarcinoma of the scalp: A rare case report with review of literatureJ Clin Diagn Res 2016 10:ED15-16.10.7860/JCDR/2016/16083.714926894080 [Google Scholar] [CrossRef] [PubMed]
[11]. Devi NR, Valarmathi K, Lilly M, Satish S, Mishra N, Primary axillary porocarcinoma: A rare cutaneous tumourJ Clin Diagn Res 2016 10(2):ED04 [Google Scholar]
[12]. Shen J, Pan X, Lu Y, Pan D, Ma Y, Zhan R, A case of eccrine porocarcinoma characterized by a progressive increase in the level of Ki-67 index: Case report and review of literatureBMC Surgery 2019 19(1):01-08.10.1186/s12893-019-0595-431601219 [Google Scholar] [CrossRef] [PubMed]
[13]. Le HM, Faugeras L, De Moor V, Fervaille C, Vander Borght T, Collette F, Eccrine Porocarcinoma: A Challenging Diagnostic and Therapeutic Tumoural EntityCase Rep Oncol 2021 14(2):700-05.10.1159/00051498434177519 [Google Scholar] [CrossRef] [PubMed]
[14]. Kurashige Y, Minemura T, Nagatani T, Eccrine porocarcinoma: Clinical and pathological report of eight casesCase Rep Dermatol 2013 5:259-66.10.1159/00035560624403888 [Google Scholar] [CrossRef] [PubMed]
[15]. Nazemi A, Higgins S, Swift R, In G, Miller K, Wysong A, Eccrine porocarcinoma: New insights and a systematic review of the literatureDermatologic Surgery 2018 44(10):1247-61.10.1097/DSS.000000000000156629894433 [Google Scholar] [CrossRef] [PubMed]