The Supraglottic Airway Devices (SAD) has a prominent place in the management of patients with difficult airway [1]. The SAD holds an important place in management of both unanticipated and predicted difficult airway in several airway management guidelines by various academic anaesthesia societies [2-5]. According to American Society of Anesthesiologists (ASA) difficult airway management guidelines, SADs have utility in various scenarios of anticipated difficult airway. The SAD can be used after failure of awake intubation attempt. If initial endotracheal intubation attempts after induction of anaesthesia fails, SAD can be used after attempting face mask ventilation. The SAD also has a role in emergency non invasive airway ventilation and after failure of multiple/alternative attempts of intubation [2].
Difficult Airway Society (DAS) and All India Difficult Airway Association (AIDAA) guidelines advocate insertion of SAD as ‘plan B’ or second step after failure of intubation in patients with unanticipated difficult airway [2,3]. Both these guidelines prefer second generation SADs as they have may have better safety and efficacy. DAS has described ideal characteristics of SAD device for difficult airway management as having high insertion rate in first attempt, high oropharyngeal sealing pressure, ability to separate respiratory and gastrointestinal tract and ability to intubate trachea using Fibreoptic Bronchoscope (FOB) [4].
Despite the lack of studies on difficult airway, SAD are widely used and recommended for this purpose [1,2,4]. The present trial was designed to compare the efficacy and safety of LMA classic and I-gel for management of anticipated difficult airway. It was hypothesised that I-gel, with its several design advantages, has better success rate of insertion in patients with anticipated difficult airway. I-gel and LMA were chosen for this trial as these two are one of the most used SADs in India.
Materials and Methods
This prospective, randomised, single blinded clinical trial was conducted in a King George’s Medical University, Lucknow, Uttar Pradesh, India, between February 2019 to January 2020 after taking approval of Ethics Committee (letter number: 39/Ethics/19, date: 16/01/2019). Informed and written consent was taken from all the study participants.
Sample size calculation: The present trial had a power of 0.8 and type I error of 5%. The success of I-gel insertion in patients with anticipated difficult airway was 91.7% according to previous trial [15]. To detect a difference of 25% in success rate of insertion, 41 subjects were needed in each group. Total 50 patients were recruited in each group to account for the patient exclusions and data loss.
Inclusion criteria: The study included 18 to 60-year-old patients of American Society of Anaesthesiologists (ASA) physical status I or II, scheduled to undergo short duration (<2 hours) elective surgical procedure under general anaesthesia. Patients with features suggestive of difficult airway defined as the presence of one or more following features: Mallampati class 3 or 4, thyro-mental distance <6 cm, sterno-mental distance <12 cm, restricted neck movement, micrognathia, retrognathia, short neck or thick neck were included.
Exclusion criteria: Patients who refused to gave consent, having inter-incisor gap <3 cm, with Body Mass Index (BMI) >35 kg/m2, pregnant patients, who required laparoscopic surgery, were at risk for aspiration or other difficult airway features were excluded.
Study Procedure
Patients were randomly divided into either of the two groups using opaque sealed, envelope technique. Patients assigned to group C had their airway managed using cLMA and those assigned to group I had their airway managed using I-gel as the primary airway device. Patients were not aware of their study group allocation.
After arrival of patients in Operation Room, peripheral intravenous access was secured and standard anaesthetic monitors like pulse oximeter, electrocardiogram and non invasive blood pressure were applied. Patients were preoxygenated with 100% oxygen and induced with intravenous 2 microgram/kg fentanyl, titrated doses of propofol and 1.5 mg/kg succinylcholine. The SAD of appropriate size was inserted according to the manufacturer’s recommendations [16,17].
Correct SAD placement was defined as chest movement with ventilation, square waveforms on capnography, bilateral breath sounds on chest auscultation and Leak fraction (LF) (defined as the difference in inspired and expired tidal volume divided by inspired tidal volume) <15%. If device placement was not adequate, minor manipulations were done to achieve correct device placement. In case of unsatisfactory device placement, face mask ventilation was done and SAD placement was re-attempted. Maximum three attempts were allowed for SAD placement, after which endotracheal tube was placed after direct laryngoscopy. These patients were not included in secondary outcome variables of the study. After SAD insertion, patients were ventilated with 7 mL/kg tidal volume and anaesthesia was maintained using oxygen, nitrous oxide, sevoflurane, and intermittent boluses of injection vecuronium. At the end of surgery, the anaesthetic drugs were discontinued, muscle relaxant was reversed, and the SAD was removed.
Primary outcome measure of this trial was the rate of successful insertion of SAD. Secondary outcomes were first attempt success rate, number of attempts taken to insert the SAD, manipulations needed to insert the device, insertion time, LF, Oropharyngeal leak pressure (OLP), best view of larynx {Fiberoptic View (FOV)} through FOB, and side-effects.
The time gap between picking up the SAD and successful placement of the device was recorded as the time to insert the device. For measuring the OLP, fresh gas flow was set at three litres/minute, ventilator was placed in manual/spontaneous mode and adjustable pressure limiting valve of breathing circuit was set at 40 cm of water. The pressure at which leak could be auscultated using a stethoscope placed lateral to thyroid cartilage was recorded as OLP [18]. After measurement of OLP, FOB was inserted through the SAD and FOV was recorded as: (1) full view of glottis obtained; (2) partial view of glottis obtained; (3) only epiglottis visible; and (4) no recognisable laryngeal structures visible [18]. Side effects including, but not limited to sore throat, airway obstruction, desaturation (defined as oxygen saturation of arterial blood below 90%), airway injury, haemodynamic disturbances (>25% change from baseline value) and regurgitation were also recorded.
Statistical Analysis
Parametric continuous quantitative data were compared using Student’s t-test. Non parametric continuous/discrete, and ordinal variables were compared using Mann-Whitney U test. Nominal variables were analysed using chi-squared test. A two-sided p<0.05 were considered significant for all the tests. Analysis was performed using Statistical Package for Social Sciences (SPSS) version 25.0 for windows.
Results
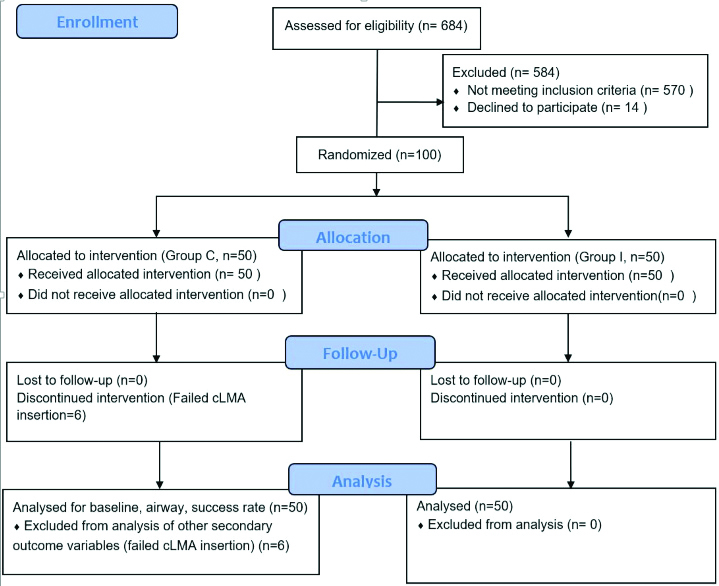
The flow of patients in the present trial is shown in [Table/Fig-1]. The baseline and demographic characteristics of the two groups are compared in [Table/Fig-2] and were statistically similar. Airway characteristics were also comparable between the two groups [Table/Fig-3].
Comparison of baseline characteristics.
| Variables | Group C (n=50) | Group I (n=50) | p-value |
|---|
| Age (years) | 40.38±12.96 | 37.94±11.77 | 0.327 |
| Weight (kg) | 65.50±9.61 | 67.34±9.52 | 0.338 |
| Height (cm) | 160.94±7.01 | 162.56±8.22 | 0.292 |
| BMI (kg/m2) | 25.35±3.89 | 25.52±3.40 | 0.824 |
| Gender (M/F) | 22 (44%)/28 (56%) | 29 (58%)/21 (42%) | 0.161 |
| ASA(I/II) | 32 (64%)/18 (36%) | 26 (52%)/24 (48%) | 0.224 |
Data are expressed as mean±SD or number (percent); BMI: Body mass index in Kg/m2; M: Male; F: Female; ASA: American society of anesthesiologists physical status
Comparison of airway characteristics.
| Variables | Group C (n=50) | Group I (n=50) | p-value |
|---|
| Inter-incisor gap (cm) | 4.15±0.81 | 4.33±0.76 | 0.260 |
| MPG | 3 (2-4) | 3 (3-4) | 0.433 |
| TMD (<6 cm/≥6 cm) | 18 (36%)/32 (64%) | 15 (30%)/35 (70%) | 0.523 |
| SMD (<12 cm/≥12 cm) | 16 (32%)/34 (68%) | 13 (26%)/37 (74%) | 0.509 |
| Yes/No (n,%) | Yes/No (n,%) | |
| Limited NM | 14 (28%)/36 (72%) | 10 (20%)/40 (80%) | 0.349 |
| Thick neck | 17 (34%)/33 (66%) | 13 (26%)/37 (74%) | 0.383 |
| Short neck | 16 (32%)/34 (68%) | 12 (24%)/38 (76%) | 0.373 |
| Micrognathia | 9 (18%)/41 (82%) | 5 (10%)/45 (90%) | 0.249 |
| Retrognathia | 6 (12%)/44 (88%) | 5 (12%)/45 (88%) | 0.749 |
Data are expressed as mean±SD or number (percent); MPG: Mallampati grade; NM: Neck movement; TMD: Thyromental distance; SMD: Sterno-mental distance
The difference in success rate of SAD insertion was statistically significant (p-value=0.012) with cLMA placement successful in 44 (88%) patients and I-gel placement successful in all the 50 (100%) patients. Six patients in whom cLMA insertion was not successful were not included for further analysis. Other insertion and maintenance characteristics are compared in [Table/Fig-4]. First attempt success rate and OLP were statistically higher in I-gel group. Time to insert the device, number of attempts, manipulations needed and LF were statistically lower with I-gel. FOV was statistically better with I-gel. Side-effects are compared in [Table/Fig-5]. Episodes of desaturation, hypertension, tachycardia, and postoperative sore throat were lower with I-gel, but other side-effects were similar. Airway obstruction, regurgitation or injury was not observed in any of the patients.
Comparison of clinical performance ofI-gel and cLMA.
| Variables | Group C (n=44) (n, %) | Group I (n=50) (n, %) | p-value |
|---|
| Success in 1st attempt | 10 (22.73) | 40 (80.00) | <0.001* |
| Attempts (1/2/3) (n,%) | 10 (22.73)/28 (63.63)/6 (13.63) | 40 (80)/6 (12.00)/4 (8) | <0.001* |
| OLP | 21.39±5.52 | 26.96±6.66 | <0.001* |
| Manipulations | 4 (2-6) | 0.5 (0-1.75) | <0.001* |
| Time to insert (seconds) | 69.93±24.19 | 41.28±22.24 | <0.001* |
| LF (%) | 11.27±1.96 | 8.08±2.35 | <0.001* |
| FOV (1/2/3/4) (n,%) | 6 (13.64)/16 (36.36)/14 (31.82)/8 (18.18) | 26 (52.00)/13 (26)/6 (12)/5 (10) | 0.001* |
Data are expressed as mean±SD, median (interquartile range) or number (percent); OLP: Oropharyngeal leak pressure in cm H2O; LF: Leak fraction; FOV: Fiberoptic view; *: Statistically significant difference
Comparison of side effects.
| Side-effect | Group C (n=44) (n, %) | Group I (n=50) (n, %) | p-value |
|---|
| Desaturation | 8 (18.18) | 1 (2) | 0.008* |
| Sore throat | 11 (25.00) | 3 (6) | 0.010* |
| Blood on device | 3 (6.82) | 2 (4) | 0.544 |
| Tachycardia | 9 (20.45) | 2 (4) | 0.013* |
| Bradycardia | 2 (4.55) | 0 | 0.128 |
| Hypertension | 7 (15.91) | 1 (2) | 0.016* |
| Hypotension | 3 (6.82) | 5 (10) | 0.581 |
Hypertension/tachycardia was defined as rise in mean blood pressure/heart rate by >25% from baseline; Hypotension/bradycardia was defined as decrease in mean blood pressure/heart rate by >25% from baseline; *: Statistically significant difference
Discussion
The present study was undertaken to compare the safety and efficacy of I-gel and cLMA for management of difficult airway. I-gel had higher overall insertion success rate, with higher first attempt success and OLP in present study. I-gel needed fewer insertion attempts, manipulations, time for insertion, and had lower LF. The FOV was better with I-gel. Desaturation, hypertension, tachycardia, and postoperative sore throat were more frequent in patients whose airway was managed using cLMA.
Several SADs including cLMA, I-gel, proseal LMA, laryngeal tube and Ambu auragain are used worldwide for management of airway in anaesthesia, critical care, emergency medicine and cardiopulmonary resuscitation [6-8,18,19]. However, high quality evidence for utility of SAD for difficult airway management is limited. Several case reports have demonstrated the utility of SAD devices in restoring the ventilation of lungs in situations where conventional airway management techniques have failed [9,10]. Successful placement of the SAD gives time to plan for further airway management options including tracheal intubation through the SAD, using SAD as device for full length of surgical procedure, surgical airway access or awakening the patient [3].
There are several case reports describing the utility of I-gel and cLMA for management of difficult airway patients, but these two devices have been compared in very few trials. Singh J et al., conducted a crossover study comparing these two devices in 48 patients with post-burn contracture of neck [15]. The insertion success was better with I-gel (91.7%) as compared to cLMA (83.33%), but the difference was not statistically significant. FOV, time of insertion and OLP were statistically better with I-gel. Arévalo-Ludeña J et al., conducted a trial to evaluate success rate of FOB guided endotracheal intubation using I-gel as conduit in patients with anticipated difficult airway [20]. I-gel was inserted in 85 patients under local anaesthesia and sedation (Ramsey sedation scale: 2-4). I-gel insertion was successful in 69 patients in first attempt and 16 patients in second attempt. FOB guided endotracheal tube was successfully placed in all the patients. Cough and sore throat were observed in six and two patients, respectively. The trials by Singh J et al., and Arévalo-Ludeña J et al., indicate that I-gel and cLMA are useful in managing anticipated difficult airway [15,20].
Success rate of I-gel insertion in present study was same as seen in study by Arévalo-Ludeña J et al., [20]. In contrast to the observations of Singh J et al., success rate of insertion was statistically better with I-gel as compared to cLMA in the present study [15]. This can be due to inclusion of patients with different airway characteristics in the present study. Patients with at least one of the several characteristics of difficult airway were included in the present study, while Singh J et al., included patients with restricted neck movement only.
Higher first attempt success rate and lower number of attempts needed to insert the device were seen with I-gel in the present study. I-gel, being a relatively recent device, has several design features that facilitate easy, rapid insertion and use. These include a non inflatable cuff which anatomically mirrors the peri-laryngeal anatomy, an integrated bite block and a buccal cavity stabiliser, an epiglottic rest and a gastric channel [21]. These design differences may be responsible for better insertion and maintenance characteristics in difficult airway also. The time needed to insert SAD was lower with I-gel due to lack of an inflatable cuff. Also, as the number of attempts taken were more with cLMA, the time to insertion also increased due to need for mask ventilation between the insertion attempts.
Trials have consistently demonstrated higher OLP with I-gel than cLMA [22,23]. The anatomically shaped, soft, and non inflatable cuff may be responsible for higher OLP in I-gel. The higher OLP suggests better safety and ability to provide positive pressure ventilation withI-gel as compared to cLMA [24]. Observations of the present study indicate that presence of difficult airway does not affect the efficacy of seal achieved by the two devices.
Better FOV indicates better alignment of the SAD cuff with the laryngeal inlet and potentially greater probability of endotracheal intubation through the SAD. Due to its design, endotracheal intubation through cLMA is not preferred, even in patients without difficult airway [25]. Glottis was visible (FOV grade 1 and 2) in 39 (78%) of I-gel patients, suggesting that FOV guided endotracheal intubation through I-gel should be feasible in patients with difficult airway. Glottis was visible in only 22 (50%) of patients whose airway was managed using cLMA, indicating less optimal position of its cuff for endotracheal intubation. Other factors that make cLMA less suitable as conduit for endotracheal intubation include: 1) long and narrow airway tube; 2) narrow connector; and 3) presence of aperture bars [25].
Episodes of desaturation, hypertension and tachycardia were higher in cLMA group as the number of attempts, manipulations and time needed for insertion were higher for cLMA. As observed in other studies, inflatable cuff of cLMA caused higher incidence of postoperative sore throat than soft, non inflatable cuff of I-gel [26,27].
Limitation(s)
There are several airway characteristics that predict difficult airway. The limitation of present study was that patients with only some of the airway characteristics were recruited in the present study. TheI-gel or cLMA may not have same efficacy as observed in the present study if other airway conditions are encountered.
Conclusion(s)
The higher success rate of I-gel along with other favourable insertion and maintenance characteristics make it a more suitable SAD for management of patients with anticipated difficult airway. However, more large scale studies are needed to recommend the routine use of I-gel over cLMA in patients with anticipated difficult airway.
Data are expressed as mean±SD or number (percent); BMI: Body mass index in Kg/m2; M: Male; F: Female; ASA: American society of anesthesiologists physical status
Data are expressed as mean±SD or number (percent); MPG: Mallampati grade; NM: Neck movement; TMD: Thyromental distance; SMD: Sterno-mental distance
Data are expressed as mean±SD, median (interquartile range) or number (percent); OLP: Oropharyngeal leak pressure in cm H2O; LF: Leak fraction; FOV: Fiberoptic view; *: Statistically significant difference
Hypertension/tachycardia was defined as rise in mean blood pressure/heart rate by >25% from baseline; Hypotension/bradycardia was defined as decrease in mean blood pressure/heart rate by >25% from baseline; *: Statistically significant difference