Introduction
Wuhan, China reported the outbreak of a neoteric variant of Coronavirus in December 2019, which was later named as “Coronavirus Disease-2019” (COVID-19) by World Health Organisation (WHO). Seeing the severity and quick spread of the disease across countries and continents, WHO emergently declared it to be a pandemic which has by far infected more than 176 million people and caused around 3.8 million deaths worldwide as on 12 June 2021 [1].
Coronavirus makes up a large family of viruses- Coronaviridae. These viruses have a single stranded, positive-sense Ribonucleic Acid (RNA) genome. These can infect both birds and humans [2]. The transmission of the virus can take place from human-to-human through close contact or transfer of droplets from an infected individual via cough/sneeze. In addition to this, Sushruta Samhit ā, a treatise of Āyurveda talks about the mode of transmission for Aupasargika Roga (Communicable/Infectious Diseases) which includes physical intimacy, touch by body parts, breath (droplet), sharing food/utensils, sleeping/sharing bedding, sitting very close or sharing clothes/jewellery/cosmetics with an infected person/carrier. [3,4]:
Prasangāt Gātrasamsparshāt Nihshvāsāt Sahabhojanāt |
Sahashaiyyāsanāt chāpi Vastramālyānulepanāt || (Su. Ni.5/32-33)
The incubation period for COVID-19 infected subjects varies from 2 to 14 days during which they may have no symptoms and the virus can be transmitted [5]. However, the most common symptoms that subjects present are throat pain, fever, cough, sneezing and shortness of breath [2]. The only way to encounter this virus is to maintain distance from the infected person, take good care of personal hygiene and sanitation, and most importantly develop a stronger immune system.
Immunity is the body’s self defence mechanism to fight against infection, disease or unwanted biological invasions like that of bacteria, virus, parasite and yeast. It comprises of a plethora of cells, tissues and organs that work in tandem, in order to defend the host against any foreign invasions. The immune system can be classified into innate and adaptive, wherein the former is activated by Pathogen Associated Molecular Patterns (PAMPs) while the latter is dependent on antigen specific B and T-lymphocytes [6].
However, even though the pathogen remains to be the same, it’s interaction with host immune system shows great variations that can be dependent upon certain individualistic factors like diet and lifestyle practices. These along with possible preventive measures are therefore indispensable for combatting the spread of COVID-19 and boosting host immunity to fight against this disease.
Risk Factors for Compromised Immunity with Special Reference to Covid-19
Age
There are various age related changes in pulmonary function due to lung infection [7]. Although COVID-19 can affect any age group, a study suggests that older people possess serious risk to COVID-19 mortality and morbidity [8]. Young children may remain asymptomatic and do not present severe disease despite high viral exposures. Due to ageing, lung microenvironment undergoes alterations in dendritic cell maturation and migration to lymphoid organs. Thus, it leads to defects in the process of T-cell activation [9].
General Lifestyle Factors
Lifestyle in general comprises of Āhāra (Dietary Habits), Vihāra (Daily Regimen), Āchāra (Conduct) and Vihcāra (Thoughts) [10]; derangements in which lead to lowered immunity and increased susceptibility to infections. Researchers have assessed the relationship of lifestyle factors like physical activity, smoking and alcohol consumption with the risk of COVID-19 and found that lifestyle modifications can not only diminish the severity of infection but also help to improve the prognosis [11].
Medical Conditions
A study on 41 COVID-19 positive patients reported that 13 (32%) of them had underlying diseases including Hypertension (HTN), Diabetes Mellitus (DM), Chronic Obstructive Pulmonary Disease (COPD) and Cardiovascular Disease (CVD). Another study on 138 cases of COVID-19 reported the presence of co-morbidities in 64 (46.4%) of the subjects. Importantly, it was found that co-morbidities were steep in those admitted to the Intensive Care Unit (ICU) i.e., 72.2% than those who were not (37.3%). This suggests that adverse outcomes may be related to co-morbidities which put the patient at an additional risk. Mortality in COVID-19 patients was elevated in those with co-morbid symptomatology accounting 10.5% for CVD, 7.3% for DM, 6.3% for COPD and 6% for HTN [12].
Hypertension (HTN)
There are several pathophysiological changes in the cardiovascular system including left ventricular hypertrophy and fibrosis in hypertensive subjects. Thus, it makes the hypertensive patient prone to more COVID-19 [13].
Diabetes Mellitus (DM)
In most studies, it was observed that diabetic COVID-19 patients have worst prognosis and increased mortality. Poor glycaemic control abrogates various aspects of the immune response. Also, inappropriate activity of T-cells, natural killer cells and complement system could hamper viral clearance [14]. DM is associated with elevated plasminogen levels, which may increase the virulence of Severe Acute Respiratory Syndrome (SARS). The pre-existing proinflammatory state accentuates the cytokine storm that can further be responsible for multiorgan dysfunction during COVID-19 [15].
Asthma
Decreased immunity has been observed in asthmatic patients which can exaggerate the symptoms of asthma on exposure to respiratory viral infections making them more susceptible to COVID-19 infection [16]. Higher severity, compromised lung function, bronchial hyper reactivity and eosinophilic inflammation have been observed in these patients [17]. Hence, all these factors together make the asthmatic patients more vulnerable.
Effects of Lifestyle on Host Immune System
Lifestyle refers to the way of living of a person, group or culture. As mentioned above, lifestyle comprises of Āhāra, Vihāra, Āchāra and Vichāra which have a direct impact on one’s physical, mental, social and spiritual well-being [10]. Although the aetiopathogenesis of an infection focuses more upon the pathogen involved, but a holistic approach would require us to go a step ahead in understanding the involvement of individualistic factors and the body-mind-soul complex.
Eating Habits
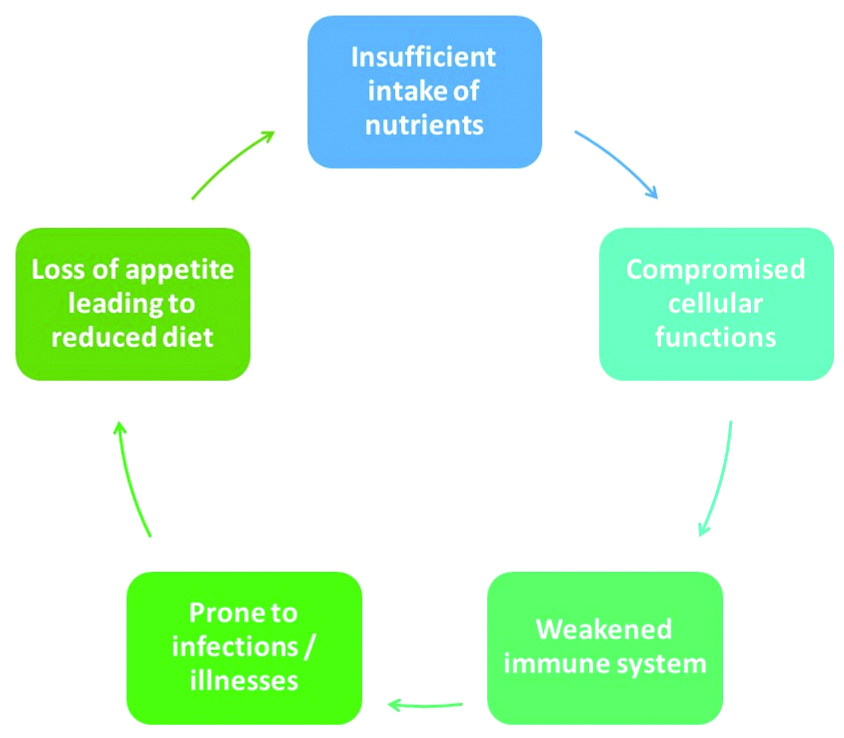
Our body’s defense mechanism is programmed in such a way that it protects us constantly from any foreign particle that enters the body. As an effect, body requires substrates for biosynthesis to meet increased rate of metabolism. This inturn increases the nutrient requirement which can be fulfilled by a healthy balanced diet to overcome and relieve its associated symptoms; otherwise, a vicious cycle continues to run between our diet, health and illness [Table/Fig-1].
Vicious cycle relating diet, health and illness.
What to eat?
Macro and micronutrients are crucial for the optimum growth and functioning of immune cells, this may involve Protein (including the amino acid-glutamine), Iron, Vitamin C, Vitamin D, Zinc and Selenium. Researches indicate that concentrates of vegetable and fruit considerably augment serum levels of antioxidant, provitamins and vitamins (Vitamin C, Vitamin E, β-Carotene, and Folate) and minimise homocysteine [18]. A balanced intake of fresh vegetables, fruits of all variety, grains and pulses offers vitamins, minerals, fibers, phytochemicals and antioxidants. In addition to this, sufficient nuts and oilseeds provide protein, essential fatty acids and magnesium; and an occasional non vegetarian diet, preferably lean fish as it contains zinc that fights against infection. It is advisable to avoid intake of hydrogenated oils, saturated fats and starches in higher proportions, and to reduce consumption of sugar, carbonated drinks as they have been shown to slow the activity of white blood cells in attacking microbes and reduce the efficiency of the immune system for the elderly [19]. Zinc is a general stimulant of antiviral immunity and studies have shown its broad-spectrum antiviral activity [20].
Several researches on efficacy of vitamin supplements suggest that Vitamin C and Zinc help cut down infection, apart from boosting immunity [20,21]. Zinc is required for function of over 300 enzymes, which maintain body’s immunity and repair tissues. Meat, poultry and eggs are good sources of Zinc. Leiden medical researchers in the Netherland reported that Zinc inhibits coronavirus [21]. Recent studies have found that intestinal homeostasis is preserved by probiotics. It modulates the body’s defenses and induces the maturation of T-regulatory cells. Innate immunity gets influenced by specific probiotic strains and postbiotics [22]. Probiotics are live microbes known to facilitate health benefits if consumed in optimum quantity. Lactic acid bacteria and bifido bacteria are most commonly consumed [6]. In a study, it was also suggested that the alkylamines present in apples, tea and wine may provide immunomodulation and enhance immunity [23].
Apart from what to eat/what not to eat, a few more concepts need to be understood for the food to undergo proper ingestion, digestion, absorption, assimilation and excretion as these steps are crucial for strengthening the immune system and cater to a more individualised idea of overall health [24].
When to eat?- “True Hunger” or “Stomach Hunger” can be identified through symptoms like clear belching, feeling of enthusiasm, proper passage of faeces and urine, feeling of lightness in body and stomach, feeling of hunger and feeling of thirst [25].
Udgāra shuddhihi Utsāho Vegotsarga Yathochitaha |
Laghutā Kshut Pipāsācha Jīrna Āhārasya Lakshanam ||
(Yoga Ratnākara, Ajīrna Prakarana)
Care must be taken to avoid eating without the appearance of these symptoms or not eating on the appearance of these symptoms; as both can have dangerous outcomes. Further, the night meal must be consumed atleast 2 hours before the bedtime [26].
How to eat?- Eating is a very pious activity that should have a set protocol [27]. Irrespective of being healthy/unhealthy, one must sit properly with a slight forward bend keeping in mind some basic rules, such as: - Food should be warm, unctuous, in proper quantity, consumed after digestion of previous meal, not having contradictory potencies, consumed at a proper place and with all accessories, not consumed in a hurry or too slow. Food should be consumed with full concentration without talking/laughing/being unmindful and after paying due regard to oneself [28].
Ushnam snigdham mātrāvat jīrne vīrya aviruddham ishta deshe ishta sarvopakaranam na ati drutam na ati vilambitam ajalpan na hasan tana manābhunjīt ātmānam abhisamīkshya samyak || (Ch.Vi.1/24)
How much to eat?- There are three basic rules with respect to the proportion of food to be consumed viz., (i) eating according to one’s hunger/digestive capacity, (ii) consuming two meals a day (has exceptions and is subject to change) and (iii) depending on one’s digestive capacity, hypothetically dividing the stomach into four parts; two parts for solid food, one part for fluids and the remaining one part needs to be left for air to move [29]. These are important to prevent over/under nutrition and to give each meal sufficient time for undergoing digestion [30].
What to do before food?- “Havana” and eating are similar processes as both make offerings to fire, wherein the latter offers food to the digestive fire within us, so that it not only nourishes the body, but the mind and soul as well [31]. Bathing/washing hands, feet and face; sitting in solitude; offering the food to Gods, ancestors, elders, guests, children and gurus; feeding all the dependents of the family such as servants and pets; and carefully considering one’s own constitution, likes and dislikes are few of the important things to be kept in mind and paid attention to before consumption of food [29].
What to do after food?- The 30 minutes span after one finishes their meal plays a pivotal role in proper digestion [32]. This is a period of rest which mainly involves three activities i.e., (i) to sit in Vajrāsana/with straight spine for 10 minutes; (ii) walk slowly for 10 minutes/100 steps; and (iii) lie down in left lateral position for 10 minutes [32].
Viruddha Āhāra- Avoid incompatible diet to prevent accumulation of toxins within the body [33]. Example: Consumption of sour/salty food items with milk, consumption of curd at night etc.
Prakruti and Vikruti- The body-mind constitution and diseased condition of an individual [33].
Sleeping Habits
Regular sleeping habit exerts a strong regulatory influence on immune functions. The research study of sleep-wake cycle, has shown that immune parameters like number of undifferentiated naive T-cells and the creation of pro-inflammatory cytokines, peaks during early nocturnal sleep whereas circulating numbers of immune cells with immediate effect or functions, like cytotoxic natural killer cells as well as anti-inflammatory cytokine activity peaks during daytime wakefulness. Sleep deprivation leads to multiple diseases associated with chronic inflammation such as cognitive, cardiovascular, metabolic and other disorders. It was also observed in a study that sleeping less than six hours for a week leads to reduced levels of neutrophil phagocytosis, lower levels of Nicotinamide Adenine Dinucleotide Phosphate (NADPH) oxidase and fewer CD4 T-cells, which are necessary for anti-infective defense and proper vaccination response [34].
The pineal hormone- melatonin shows steep increase in their blood levels during sleep. Growth hormone, prolactin, melatonin and leptin exert remarkably synergistic actions on the immune system [35]. During the sleeping period, immune cells at early stages of differentiation peak in peripheral blood and lymph node immune cells migrate. New cells are constantly released from the bone marrow into the circulation. T and B-cells circulate for up to years until they encounter their associated antigen in secondary lymphatic tissues, whereas other cells, like macrophages and neutrophils, extravagate to peripheral tissues already after a few hours or days [34].
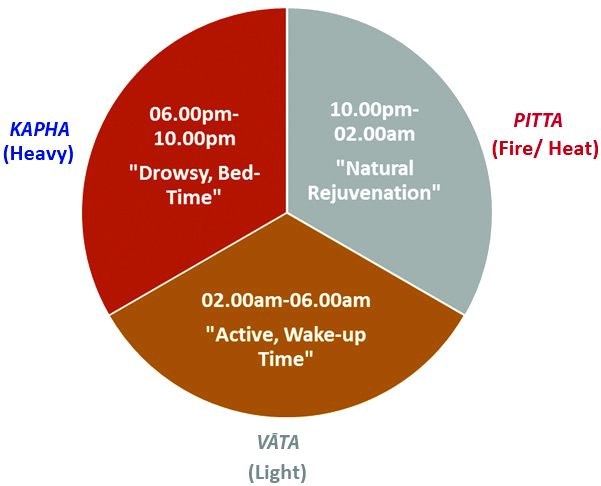
Proper and undisturbed night sleep is one of the most essential factors for health as it imparts happiness, nourishment, strength, virility, knowledge and life; while on the other hand, improper sleep takes away all these pushing one into misery, emaciation, weakness, sterility, ignorance and death [28]. The sleep pattern in general can be understood through the following table with a proper 6-8 hours of night sleep [Table/Fig-2] [36].
Pie diagram depicting 12 hours of night with doshic predominance. 10.00 pm-02.00 am is essentially the time of cell repair and one must be asleep during these hours to facilitate the same
Physical Activity
Physical activity can be defined as those exercises which increase stability and overall strength of the body [28]. Various studies have reported that physical activity significantly reduces the risk of viral infections and levels of stress and anxiety. In addition to its short-term benefits, regular physical activity lowers the risk of chronic health conditions (e.g., diabetes, coronary heart disease and HTN) which are cited as the most frequent co-morbidities in recent studies of COVID-19 [37]. The immune adaptation to physical activity depends on the intensity, duration and kind of exercise, as well as environment, temperature, nutrition, hydration status, body composition and concentration of hormones and cytokine [38]. Moderate intensity physical activity stimulates an increase in the antipathogen activity of macrophages in conjunction with temporary increase in the recirculation of key immune system cells-immunoglobulins and anti-inflammatory cytokines in the blood, resulting in a reduced influx of inflammatory cells into the lungs and decreased pathogen load. Intense exercise before or during viral infection has been associated with greater morbidity and mortality [39]. Exercise also releases various cytokines from the skeletal muscle (i.e., myokines) that can help maintain immune competency. A study indicates that maintaining physical activity has immune benefits in older adults, for example, it reduces the systemic inflammation associated with chronic age-related diseases [40]. However, it’s important to perform any kind of exercise in moderation and according to one’s capacity.
Alcohol Consumption
People consuming alcohol have underlying medical conditions that place them at high risk for severe COVID-19 infection, including obesity with metabolic syndrome, chronic kidney disease, and/or being immunocompromised due to corticosteroid therapy for alcoholic hepatitis [41]. According to a research study, it was observed that alcohol consumers have almost three times the rate of sleep problems, twice the rate of presumptive heart problems, injuries and chronic lung infections than non users [42]. In a study, it was mentioned that with chronic alcohol ingestion, oxidative stress pathways in the alveolar macrophages are stimulated, thereby impairing alveolar macrophage’s immune capacity and pathogen clearance [43].
Smoking
According to reports by WHO, smoking being the most important risk factor for COPD, that causes swelling and rupturing of the air sacs in lungs, reducing the lung’s capacity and building up mucus, resulting into painful coughing and breathing difficulties makes smokers highly susceptible to COVID-19 infection and mortality. Smoking impacts both innate and adaptive immunity and plays dual roles in regulating immunity by either exacerbation of pathogenic immune responses or attenuation of defensive immunity. Smoking is additionally related to increased development of acute respiratory distress syndrome, a key complication for severe cases of COVID-19, among people with severe respiratory infections [44].
Smoking and e-cigarette increase the risk and severity of pulmonary infections because of damage to upper airways and a decrease in pulmonary immune function [45]. It has been observed that smokers are 1.4 times more likely to have severe symptoms of COVID-19 and approximately 2.4 times more likely to be admitted to the ICU, who further need mechanical ventilation or die compared to non smokers. Hence, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19 [46]. Adaptive immune cells affected by smoking mainly include T-helper cells (Th1/Th2/Th17), CD4+ CD25+ regulatory T-cells, CD8+ T-Cells, B-cells and memory T/B lymphocytes while innate immune cells impacted by smoking are mostly dendritic cells, macrophages and natural killer cells [47]. A study found that active smoking increases the percentage of CD8+ T-cells but lowers CD4+ T-cells in humans while passive smoking generally augments human CD3+ T-cells [48].
Mental Health
The mental urges like greed, grief, fear, anger, ego, jealousy, attachment etc. must be under one’s control for better concentration, retention, intelligence, memory and overall mental health [28]. Various research studies have shown that cytokines are important for regulation of the immune system. Also, they act as neurotransmitter molecules, and a mental disorder like schizophrenia or depression can affect the functioning of cytokines and vice versa. As a result, there will be insufficient production of cytokines that will further reduce the neural transmission that can cause various mental disorders [49,50]. It has been reported in studies that anxiety or stress leds to the release of hormones like adrenaline, which in the long term can result into a weakened immune system that can expose the host to attacks of viruses such as SARS-CoV2. Insomnia, fatigue and other physical changes lead by a depressed state of mind can further weaken the immune system rendering the host susceptible to foreign pathogens. It can even lead to Type-II diabetes that can further compromise the immunity level. Stress affects hormones from various glands like thyroid, pancreas, adrenal etc., which influence the immune response; like serotonin causes delay of the primary immune response and lowers the primary and secondary antibody response intensity [51].
The mind and the soul need to be given equal importance as the body since they play a major role in the cycle of disease causation, treatment and prevention. The Yamas and Niyamas of Ashtānga Yoga as enlisted below can be treated as the stepping stones towards mental, social and spiritual health [Table/Fig-3] [52].
Yamas (Social Restraints) and Niyamas (Personal Observances) mentioned under AshtāngaYoga.
| Yamas | Niyamas |
|---|
| Ahimsā (Non violence) | Shaucha (Cleanliness) |
| Satya (Truthfullness) | Santosha (Contentment) |
| Asteya (Non stealing) | Tapa (Target/Penance) |
| Brahmacharya (Conduct like brahma) | Svādhyāya (Self Study) |
| Aparigraha (Non accumulation) | Īshwar Pranidhāna (Surrenderance) |
Approaches to Cope Up with Covid-19
The public advisory released by WHO for COVID-19 specifies washing hands regularly and thoroughly with soap and water, using hand sanitiser that contains atleast 60% alcohol especially after visiting a public place, or after blowing nose, sneezing or coughing, maintaining social distancing of atleast 1 meter or 3 feet, avoiding close contact with people who are sick/showing symptoms like coughing or sneezing, strictly avoiding large events and mass gatherings. Alongside this many countries have come up with protocols revolving around their traditional systems of medicine. In India, extensive work is being done to utilise the inherent yet unrealised benefits of Āyurveda and Yoga. The Ministry of AYUSH (MoAYUSH), Govt. of India (GOI); has released guidelines and self-care measures based on Āyurvedic and Yogic principles for enhancing immunity.
Āyurveda, the science of life, suggests measures for maintenance of health, harmony and happiness at the level of body, mind, senses and soul. It has an extensive knowledge based on preventive care and health promotion, which mainly revolves around the concepts of “Dinacharyā” - Daily Regimen, “Rā tricharyā ” - Night Regimen, “Ritucharyā” - Seasonal Regimen and “Sadvrutta” - Good Conduct [53]. Āyurveda is not merely a medical system that prescribes medicines, but a science that educates on happy and healthy living. Charaka Samhitā, a classical textbook of Āyurveda, describes epidemic management under Janapadodhwamsa and defines immunity as the ability to fight against manifested diseases along with resisting the process of pathogenesis to maintain homeostasis [54]. Āyurveda suggests to strengthen the mind and body for coping up with various stressors, including infection. This strength/immunity (Bala) is classified as natural (Sahaja), chronobiological (Kālaja) and acquired (Yuktikrut). The A_yurvedic approach for health promotion is holistic and personalised based on host and environmental factors. The remedies include Svasthavrutta (healthy regimen), Panchakarma (therapeutic cleansing procedures) [55] and Rasāyana (immunomodulators) [56]. An individual’s genetic composition known as Prakruti (Vāta, Pitta, Kapha, a combination of two or all the three) helps in deciding the specific therapeutic agents and practices to be employed [57].
Local Prophylaxis
The main gateways for entry of droplets carrying the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) are eyes, nose and mouth. Āyurvedic texts describe few local therapies that provide symptomatic relief in mild cases such as consuming hot water, warm food, medicated water gargles, steam inhalation etc., [58].
Nasya/Nasal instillations: Nose is the doorway to our head [59] and head is the central processing unit of our body. Hence, anything instilled through the nose would not only nourish the head but the body as a whole. Nasya can be practiced by applying sesame oil/coconut oil/Anutaila in both the nostrils, twice a day for clearing the nasal passage to enable proper breathing and ward off diseases especially affecting head and neck [60].
Kavala and Gandāsha/Gargles and mouth rinse: Warm liquids, ghee and oils are used for gargling or rinsing mouth to thoroughly cleanse the mouth, throat [61], oral cavity, pharynx, and tonsillar area. Additionally, they induce immunomodulatory, antioxidant, and antimicrobial benefits by coating the mucosa as a biofilm [62]. They can be practiced 1-2 times a day using sesame oil/coconut oil/ghee/warm water.
Steam inhalation: Several clinical studies have reported the role of steam inhalation and hot fomentation in enhancing nasal conditioning and nasal mucus velocity while decreasing congestion and inflammation. They are known to provide significant relief in nasal and throat congestion, bronchoconstriction, headache and sinusitis [63].
Beverages
Several beverages made at home can be used for promoting immunity like warm water; herbal tea/decoction made from Tulsi (Basil), Dālchīni (Cinnamon), Kālimirch (Black Pepper), Shunthi (Dry Ginger) and Munakkā (Raisin); and Golden Milk i.e., 150 mL of warm milk with half a teaspoon of Haldi (Turmeric) [53].
Chyawanprāsha
Chyawanprāsha is an A_yurvedic health supplement which is made up of a super-concentrated blend of 50 nutrient-rich herbs and minerals. It is meant to restore drained reserves of life force (Ojas) and to preserve strength, stamina, and vitality, while stalling the course of ageing. It is known to protect and strengthen the respiratory system. It has antioxidant, adaptogenic, immune-booster, nootropic and cardiotonic activity. About 10g (1tsf) of Chyawanprāsha can be taken in the morning along with warm water/milk [64].
Systemic Prophylaxis
A_yurveda promotes several non pharmacological methods that are critical to overall health including diet, sleep, mental relaxation, lifestyle, behaviour and Yoga. Diet, Sleep and Conduct have rather been referred to as the Trayopastambha i.e., The Three Pillars of Health [65]. Several studies have endorsed the role of Yoga’s breathing techniques (Prānāyāma), postures (A_sanas) and procedures (Yogic Kriyās)) in improving lung health and exercise tolerance [66].
Ashtānga Yoga
Practicing Yoga helps in achieving a higher level of immunity to face the virus, as it is a discipline which creates balance at the physical, mental, social and spiritual spheres of life. It lowers stress hormones that compromise the immune system, while also conditioning the lungs and respiratory tract, stimulating the lymphatic system to toxins from the body and carrying oxygenated blood to the various organs to ensure their optimal function. The eight classes of Yoga viz., - Yama, Niyama, A_sana, Prānāyamā, Pratyāhāra, Dhārana, Dhyāna and Samādhi [67]; each contribute to immunity building and overall health. Yogaāsanas like Bhujangāsana, Sarvāngāsana, Tādāsana, Gomukhāsana, Ardhamatsyendrāsana, Sārya Namaskār etc. are highly beneficial in respiratory disorders. The Yogic prānāyāma and kriyās which help to keep the airways clean include Kapālabhāti, Anuloma-Viloma, Ujjāyi, Nādi Shodhana, Bhrāhmari and Sama Vrutti. There are three types of breathing - abdominal, thoracic and clavicular. Complete breathing also called as Yogic breathing is done by unifying these three types of breathing that is intended to take advantage of all/maximum lung capacity. Furthermore, a reduction in markers of inflammation and virus-specific immune response is observed on practicing regular meditation and mind-body relaxation techniques [68].
Rasāyana/Rejuvenants
Ashwagandhā(Withania somnifera) is a highly revered herb in the A_urvedic pharmacopeia and is considered to be the “King of A_yurvedic Herbs”. Being a Rasā yana (adaptogen) it supports the body’s ability to withstand stress and anxiety. Rasāyanas in general, help replenish the tissues of the body and are recommended in conditions like weakness, debility or decrease in Ojas (strength and vigor). Ashwagandhā helps to tranquil the nervous system and ease out the feeling of anxiousness. It is known to help bring cortisol (a steroid hormone which reaches an abnormal level whenever one becomes stressed or anxious) back to normalcy. It strengthens the body’s natural resistance by improving cell-mediated immunity and providing protection against cellular damage (caused by free radicals) through its effective antioxidant properties. Antibacterial, antitumoural, immune-modulating and anti-inflammatory properties have been observed by isolation of Withaferin A and 3-b-hydroxy-2,3-dihydrowithanolide F from Withania somnifera [69]. The government has also instigated a research study on Ashwagandhā to assess if it can be used alternatively to the existing antimalarial drug Hydroxychloroquine (HCQ) as a potential COVID-19 preventive. Other Rasā yana drugs such as Tinospora cordifolia (Guduchi), Asparagus racemosus (Shatāvari), Phyllanthus embelica (Āmalaki) and Glycyrrhiza glabra (Yashtimadhu) are also potential immunomodulators and being researched for their future applications.
It is a well-known fact that “Prevention is better than Cure”. Thus, one has to take precautionary measures to ensure health of self and others. People with metabolic syndromes should take extra care during this pandemic as they are highly prone to the infection. However, with little yet strict modification in daily routine one can easily cope up with this stressful time. Even after the development of vaccines and large-scale immunisation drives across the globe, individuals must still abide by the public advisory released by WHO for COVID-19. In addition to this, the public guidelines released by Ministry of AYUSH and the A_yurvedic and Yogic practices must be incorporated for having an upper hand in developing immunity against COVID-19 or any future infections. An individual’s level of infection and onset of symptoms may vary depending on their immunity level. The invasion of pathogen, its interaction with the host immune system and manifestation of the disease are dependent upon various factors and lifestyle practices that affect immunity and are of great significance in the present context of COVID-19. So, every attempt should be made to increase immunity by opting nutritious eating habits and being physically active.
Conclusion(s)
A bad lifestyle is like any other pathogen that can weaken the body’s defense mechanism making way for other infections to creep in. In case of COVID-19, cytokines get activated due to an impaired immune response that cause widespread lung inflammation. This increased level of cytokines can result into septic shock and multiorgan failure. In few patients, it can even lead to circulatory failure and myocardial damage. Therefore, it becomes crucial and imperative to not only study but implement various lifestyle practices that can positively impact the host immunity. The need of the hour is for people to stay updated with information on COVID-19 and religiously follow the directions of WHO and local health authorities to prevent any secondary infections.
[1]. Worldometer. Coronavirus Cases and Deaths Worldwide Data: Worldometer; [Accessed on 12th June 2021] [Google Scholar]
[2]. Hafeez A, Ahmad S, Siddqui S, Ahmad M, Mishra S, A review of COVID-19 (Coronavirus Disease-2019) Diagnosis, treatments and preventionEJMO 2020 4(2):116-25.10.14744/ejmo.2020.90853 [Google Scholar] [CrossRef]
[3]. T AJ, Susruta Samhita of Susruta, Nidana Sthana, Chapter 5, Verse No. 32-33 2013 VaranasiChaukhambha Sanskrit Sansthan [Google Scholar]
[4]. Khhcayurveda. Breaking the Chain of Transmission [Internet]. khhcayurveda.com. 2020 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/breaking-the-chain-of-transmission/ [Google Scholar]
[5]. Prompetchara E, Ketloy C, Palaga T, Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemicAsian Pac J Allergy Immunol 2020 38(1):01-09. [Google Scholar]
[6]. Bermudez-Brito M, Plaza-Diaz J, Munoz-Quezada S, Gomez-Llorente C, Gil A, Probiotic mechanisms of actionAnn Nutr Metab 2012 61(2):160-74.10.1159/00034207923037511 [Google Scholar] [CrossRef] [PubMed]
[7]. Miller EJ, Linge HM, Age-related changes in immunological and physiological responses following pulmonary challengeInt J Mol Sci 2017 18(6):129410.3390/ijms1806129428629122 [Google Scholar] [CrossRef] [PubMed]
[8]. Covid-19 and your health Older Adults [Internet]. prevention CfDCa, editor. USA: Centers for Disease Control and prevention, USA. [Accessed on 12th June 2021] [Google Scholar]
[9]. Boe DM, Boule LA, Kovacs EJ, Innate immune responses in the ageing lungClin Exp Immunol 2017 187(1):16-25.10.1111/cei.1288127711979 [Google Scholar] [CrossRef] [PubMed]
[10]. khhcayurveda. “Rule-of-4-for-4” [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/rule-of-4-for-4/ [Google Scholar]
[11]. Hamer M, Kivimaki M, Gale CR, Batty GD, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UKBrain Behav Immun 2020 87:184-87.10.1016/j.bbi.2020.05.05932454138 [Google Scholar] [CrossRef] [PubMed]
[12]. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, ChinaLancet 2020 395(10223):497-506.10.1016/S0140-6736(20)30183-5 [Google Scholar] [CrossRef]
[13]. Kulkarni S, Jenner BL, Wilkinson I, COVID-19 and hypertensionJ Renin Angiotensin Aldosterone Syst 2020 21(2):147032032092785110.1177/147032032092785132431227 [Google Scholar] [CrossRef] [PubMed]
[14]. Nyambuya TM, Dludla PV, Mxinwa V, Nkambule BB, T-cell activation and cardiovascular risk in adults with type 2 diabetes mellitus: A systematic review and meta-analysisClin Immunol 2020 210:10831310.1016/j.clim.2019.10831331765833 [Google Scholar] [CrossRef] [PubMed]
[15]. Singh AK, Gupta R, Ghosh A, Misra A, Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerationsDiabetes Metab Syndr 2020 14(4):303-10.10.1016/j.dsx.2020.04.00432298981 [Google Scholar] [CrossRef] [PubMed]
[16]. Message SD, Laza-Stanca V, Mallia P, Parker HL, Zhu J, Kebadze T, Rhinovirus-induced lower respiratory illness is increased in asthma and related to virus load and Th1/2 cytokine and IL-10 productionProc Natl Acad Sci U S A 2008 105(36):13562-67.10.1073/pnas.080418110518768794 [Google Scholar] [CrossRef] [PubMed]
[17]. Liu S, Zhi Y, Ying S, COVID-19 and asthma: Reflection during the pandemicClin Rev Allergy Immunol 2020 59(1):78-88.10.1007/s12016-020-08797-332468411 [Google Scholar] [CrossRef] [PubMed]
[18]. Esfahani A, Wong JM, Truan J, Villa CR, Mirrahimi A, Srichaikul K, Health effects of mixed fruit and vegetable concentrates: A systematic review of the clinical interventionsJ Am Coll Nutr 2011 30(5):285-94.10.1080/07315724.2011.1071997122081614 [Google Scholar] [CrossRef] [PubMed]
[19]. Ali HI ASS, Habib HN, The effect of nutrition on immune system review paperFood Science and Quality Management 2019 90:31-35. [Google Scholar]
[20]. Read SA, Obeid S, Ahlenstiel C, Ahlenstiel G, The role of zinc in antiviral immunityAdv Nutr 2019 10(4):696-710.10.1093/advances/nmz01331305906 [Google Scholar] [CrossRef] [PubMed]
[21]. te Velthuis AJW, van den Worm SHE, Sims AC, Baric RS, Snijder EJ, van Hemert MJ, Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culturePLoS Pathog 2010 6(11):e1001176-e.10.1371/journal.ppat.100117621079686 [Google Scholar] [CrossRef] [PubMed]
[22]. Giorgetti G, Brandimarte G, Fabiocchi F, Ricci S, Flamini P, Sandri G, Interactions between innate immunity, microbiota, and probioticsJ Immunol Res 2015 2015:50136110.1155/2015/50136126090492 [Google Scholar] [CrossRef] [PubMed]
[23]. Bukowski JF, Morita CT, Brenner MB, Human gamma delta T cells recognize alkylamines derived from microbes, edible plants, and tea: Implications for innate immunityImmunity 1999 11(1):57-65.10.1016/S1074-7613(00)80081-3 [Google Scholar] [CrossRef]
[24]. Khhcayurveda. “Ahaara”: Food for Holistic Health [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/ahaara-food-for-holistic-health/ [Google Scholar]
[25]. Raghuram SY, How to know that your digestion system is working fine?IndiaEasy Ayurveda: India: Easy Ayurveda[Accessed on Apr 14, 2016] [Google Scholar]
[26]. Khhcayurveda. When to Eat?! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/when-to-eat/ [Google Scholar]
[27]. Khhcayurveda. How to Eat?! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/how-to-eat/ [Google Scholar]
[28]. Sastri K CGN, The Charaka Samhita of Agnivesa 2009 VaranasiChaukhambha Sanskrit Sansthan [Google Scholar]
[29]. Gupta A UY, Astangahrdayam of Vagbhata, Sutrasthana, Chapter 8, Verse no. 47 2011 VaranasiChaukhambha Prakashan [Google Scholar]
[30]. Khhcayurveda. How Much to Eat?! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/how-much-to-eat/ [Google Scholar]
[31]. Khhcayurveda. What to do Before Food?! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/what-to-do-before-food/ [Google Scholar]
[32]. Khhcayurveda. What to do After Food?! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/what-to-do-after-food/ [Google Scholar]
[33]. Khhcayurveda. What/What-not to Eat?! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/whatwhat-not-to-eat/ [Google Scholar]
[34]. Besedovsky L, Lange T, Born J, Sleep and immune functionPflugers Arch 2012 463(1):121-37.10.1007/s00424-011-1044-022071480 [Google Scholar] [CrossRef] [PubMed]
[35]. Shneider A, Kudriavtsev A, Vakhrusheva A, Can melatonin reduce the severity of COVID-19 pandemic?Int Rev Immunol 2020 39(4):153-62.10.1080/08830185.2020.175628432347747 [Google Scholar] [CrossRef] [PubMed]
[36]. Khhcayurveda. “Nidra”: The Sleep Pattern [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/nidra-the-sleep-pattern/ [Google Scholar]
[37]. Jurak G, Morrison SA, Leskosek B, Kovac M, Hadzic V, Vodicar J, Physical activity recommendations during the coronavirus disease-2019 virus outbreakJ Sport Health Sci 2020 9(4):325-27.10.1016/j.jshs.2020.05.00332426171 [Google Scholar] [CrossRef] [PubMed]
[38]. Romeo J, Warnberg J, Pozo T, Marcos A, Physical activity, immunity and infectionProc Nutr Soc 2010 69(3):390-99.10.1017/S002966511000179520569522 [Google Scholar] [CrossRef] [PubMed]
[39]. Martin SA, Pence BD, Woods JA, Exercise and respiratory tract viral infectionsExerc Sport Sci Rev 2009 37(4):157-64.10.1097/JES.0b013e3181b7b57b19955864 [Google Scholar] [CrossRef] [PubMed]
[40]. Duggal NA, Niemiro G, Harridge SDR, Simpson RJ, Lord JM, Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity?Nat Rev Immunol 2019 19(9):563-72.10.1038/s41577-019-0177-931175337 [Google Scholar] [CrossRef] [PubMed]
[41]. Da BL, Im GY, Schiano TD, Coronavirus Disease 2019 hangover: A rising tide of alcohol use disorder and alcohol-associated liver diseaseHepatology 2020 72(3):1102-08.10.1002/hep.31307 [Google Scholar] [CrossRef]
[42]. Benegal V, Patterns and consequences of Alcohol Misuse in India- an epidemiological surveyBangaloreNational Institute of Mental Health and Nuerosciences (NIMHANS) [Google Scholar]
[43]. Yeligar SM, Chen MM, Kovacs EJ, Sisson JH, Burnham EL, Brown LA, Alcohol and lung injury and immunityAlcohol 2016 55:51-59.10.1016/j.alcohol.2016.08.00527788778 [Google Scholar] [CrossRef] [PubMed]
[44]. Mehta H, Nazzal K, Sadikot RT, Cigarette smoking and innate immunityInflamm Res 2008 57(11):497-503.10.1007/s00011-008-8078-619109742 [Google Scholar] [CrossRef] [PubMed]
[45]. Arcavi L, Benowitz NL, Cigarette smoking and infectionArch Intern Med 2004 164(20):2206-16.10.1001/archinte.164.20.220615534156 [Google Scholar] [CrossRef] [PubMed]
[46]. Vardavas CI, Nikitara K, COVID-19 and smoking: A systematic review of the evidenceTob Induc Dis 2020 18:2010.18332/tid/119324 [Google Scholar] [CrossRef]
[47]. Qiu F, Liang CL, Liu H, Zeng YQ, Hou S, Huang S, Impacts of cigarette smoking on immune responsiveness: Up and down or upside down?Oncotarget 2017 8(1):268-84.10.18632/oncotarget.1361327902485 [Google Scholar] [CrossRef] [PubMed]
[48]. Zhang MQ, Wan Y, Jin Y, Xin JB, Zhang JC, Xiong XZ, Cigarette smoking promotes inflammation in patients with COPD by affecting the polarization and survival of Th/Tregs through up-regulation of muscarinic receptor 3 and 5 expressionPLoS One 2014 9(11):e11235010.1371/journal.pone.011235025375131 [Google Scholar] [CrossRef] [PubMed]
[49]. Santoft F, Hedman-Lagerlöf E, Salomonsson S, Lindsäter E, Ljótsson B, Kecklund G, Inflammatory cytokines in patients with common mental disorders treated with cognitive behavior therapyBrain, Behavior, & Immunity-Health 2020 3:10004510.1016/j.bbih.2020.10004534589836 [Google Scholar] [CrossRef] [PubMed]
[50]. Zhang JM, An J, Cytokines, inflammation, and painInt Anesthesiol Clin 2007 45(2):27-37.10.1097/AIA.0b013e318034194e17426506 [Google Scholar] [CrossRef] [PubMed]
[51]. Solomon GF, Psychoneuroimmunology: Interactions between central nervous system and immune systemJ Neurosci Res 1987 18(1):01-09.10.1002/jnr.490180103 [Google Scholar] [CrossRef]
[52]. Yoga DC. Denver: CorePower Yoga [Internet] Yoga DC, editor. Denver: CorePower Yoga: Denver: CorePower Yoga. [Accessed on Oct 20, 2020] [Google Scholar]
[53]. Ayush Mo. Ayurveda’s immunity boosting measures for self-care during COVID-19 crises Ministry of Ayush: Ministry of Ayush; 2020 [Google Scholar]
[54]. A Y. Charaka Samhita, Sustrasthana, Chapter 28, Verse no. 7 Varanasi, India: Chaukhamba Surbharati1992 [Google Scholar]
[55]. Vinjamury SP, Vinjamury M, Sucharitakul S, Ziegler I, Panchakarma: Ayurvedic detoxification and allied therapies-is there any evidence? 2012 BerlinSpringer10.1007/978-3-642-24565-7_7 [Google Scholar] [CrossRef]
[56]. Balasubramani SP, Venkatasubramanian P, Kukkupuni SK, Patwardhan B, Plant-based rasayana drugs from ayurvedaChin J Integr Med 2011 17(2):88-94.10.1007/s11655-011-0659-521390573 [Google Scholar] [CrossRef] [PubMed]
[57]. Patwardhan B, Bodeker G, Ayurvedic genomics: Establishing a genetic basis for mind-body typologiesJ Altern Complement Med 2008 14(5):571-76.10.1089/acm.2007.051518564959 [Google Scholar] [CrossRef] [PubMed]
[58]. Sumantran VN, Tillu G, Cancer, inflammation, and insights from ayurvedaEvid Based Complement Alternat Med 2012 2012:30634610.1155/2012/30634622829853 [Google Scholar] [CrossRef] [PubMed]
[59]. Gupta A UY, Astangahrdayam of Vagbhata, Sutrasthana, Chapter 20, Verse no. 1 2011 VaranasiChaukhambha Prakashan [Google Scholar]
[60]. Khhcayurveda. Nose – The Door to your Head! [Internet]. khhcayurveda.com. 2018 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/nose-the-door-to-your-head/ [Google Scholar]
[61]. Amruthesh S, Dentistry and Ayurveda-IV: Classification and management of common oral diseasesIndian J Dent Res 2008 19(1):52-61.10.4103/0970-9290.3893318245925 [Google Scholar] [CrossRef] [PubMed]
[62]. Shanbhag VK, Oil pulling for maintaining oral hygiene-A reviewJ Tradit Complement Med 2017 7(1):106-09.10.1016/j.jtcme.2016.05.00428053895 [Google Scholar] [CrossRef] [PubMed]
[63]. Abbott DJ, Baroody FM, Naureckas E, Naclerio RM, Elevation of nasal mucosal temperature increases the ability of the nose to warm and humidify airAm J Rhinol 2001 15(1):41-45.10.2500/10506580178132946411258654 [Google Scholar] [CrossRef] [PubMed]
[64]. Sharma R, Martins N, Kuca K, Chaudhary A, Kabra A, Rao MM, Chyawanprash: A traditional Indian bioactive health supplementBiomolecules 2019 9(5):16110.3390/biom905016131035513 [Google Scholar] [CrossRef] [PubMed]
[65]. Khhcayurveda. Trayopstambha: The 3 Pillars of Health [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/__trashed/ [Google Scholar]
[66]. Kaminsky DA, Guntupalli KK, Lippmann J, Burns SM, Brock MA, Skelly J, Effect of yoga breathing (pranayama) on exercise tolerance in patients with chronic obstructive pulmonary disease: A randomized, controlled trialJ Altern Complement Med 2017 23(9):696-704.10.1089/acm.2017.010228714735 [Google Scholar] [CrossRef] [PubMed]
[67]. Khhcayurveda. Power Yoga….Unveiled! [Internet]. khhcayurveda.com. 2017 [cited 2020 Sep 10]. Available from: https://khhcayurveda.com/power-yoga-unveiled/ [Google Scholar]
[68]. Morgan N, Irwin MR, Chung M, Wang C, The effects of mind-body therapies on the immune system: Meta-analysisPLoS One 2014 9(7):e10090310.1371/journal.pone.010090324988414 [Google Scholar] [CrossRef] [PubMed]
[69]. Singh A, Duggal S, Singh H, Singh J, Katekhaye S, Withanolides: Phytoconstituents with significant pharmacologoical activitiesInternational Journal of Green Pharmacy 2010 :410.4103/0973-8258.74130 [Google Scholar] [CrossRef]