Extraosseous Aneurysmal Bone Cyst at Hypothenar Area in an Adult Male- A Case Report
Sheerin Shah1, Vikram Narang2, Rajinder K Mittal3, Ramneesh Garg4, Amandeep Kaur5
1 Associate Professor, Department of Plastic Surgery, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
2 Associate Professor, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
3 Professor and Head, Department of Plastic Surgery, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
4 Professor, Department of Plastic Surgery, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
5 MCh Resident, Department of Plastic Surgery, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sheerin Shah, HJ 103, BRS Nagar, Ludhiana, Punjab, India.
E-mail: sheerinkathpal@gmail.com
Aneurysmal Bone Cyst (ABC) is a benign tumour of bone which develops most frequently in the metaphysis of long bones and the posterior elements of vertebral bodies. The ABC generally occurs during the first two decades of life and has a slight predilection for the female sex. Radiographically, ABC is usually eccentric, lytic and expansile with well defined margins. Soft tissue or extra osseous ABC is extremely rare in occurrence, with only few case reports found in literature. Extraosseous ABC is usually found in soft tissues of lower limb and arm. Its occurrence in soft tissue of hands is extremely rare. Hereby, authors reported a case of a 30-year-old male patient who had swelling of approximately 9×6 cm in hypothenar area of left hand starting proximally from the wrist crease and extending distally till distal palmar crease and from the ulnar border of the palm till the mid palmer area. Authors described this case to highlight this entity, at an uncommon location (hypothenar area of palm) and importance of excisional biopsy in such cases.
Atypical hand cyst, Hand, Hypothenar cyst, Myositis ossificans, Palm
Case Report
A 30-year-old male reported, with the chief complaint of painless swelling over the left palm and inability to extend the ring and little finger following a minor blunt trauma to the hand eight months back. The swelling gradually increased to its present size. There was no history of ulceration, discharge or redness over the swelling. On examination, a single firm non tender swelling of approximately 9×6 cm was present in hypothenar area of left hand starting proximally from the wrist crease and extending distally till distal palmar crease and from the ulnar border of the palm till the mid palmer area. The overlying skin was tense and warm to touch, but the surrounding skin was normal [Table/Fig-1,2]. On his previous outpatient consultation from another hospital, Magnetic Resonance Imaging and Fine Needle Aspiration Cytology (FNAC) were done, which were suggestive of Haemangioma.
Clinical view of swelling in left hypothenar area.

Lateral view of swelling.

After admission to the department, he underwent investigations to establish a definitive diagnosis. Soft tissue ultrasonography of the left hand was done which showed evidence of a heterogenous hypoechoic lesion measuring 7.4×4.6 cm on the palmar aspect of the left hand encasing the 5th metacarpal and extending into inter carpal space between the 4th and 5th metacarpal extending into the dorsal space. No obvious feeding vessel was identifiable.
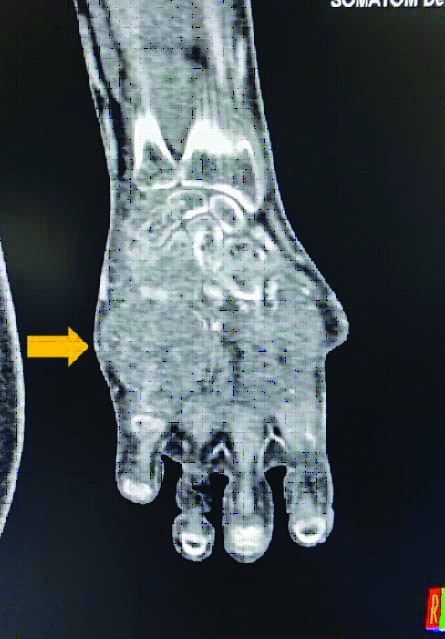
Computed Tomography (CT) of the hand showed heterogeneously enhancing lesion of the left hand with in hypothenar muscles causing erosion of the hamate and rarefaction of the bases of the 4th and 5th metacarpals. On CT angiography, the lesion was diffusely infiltrative low flow vascular malformation of soft tissue of the hand involving the bones. These findings were suggestive of angiomatosis [Table/Fig-3] and possibility of malignancy was not ruled out on CT angiography.
Computed Tomography (CT) image showing swelling in soft tissue.
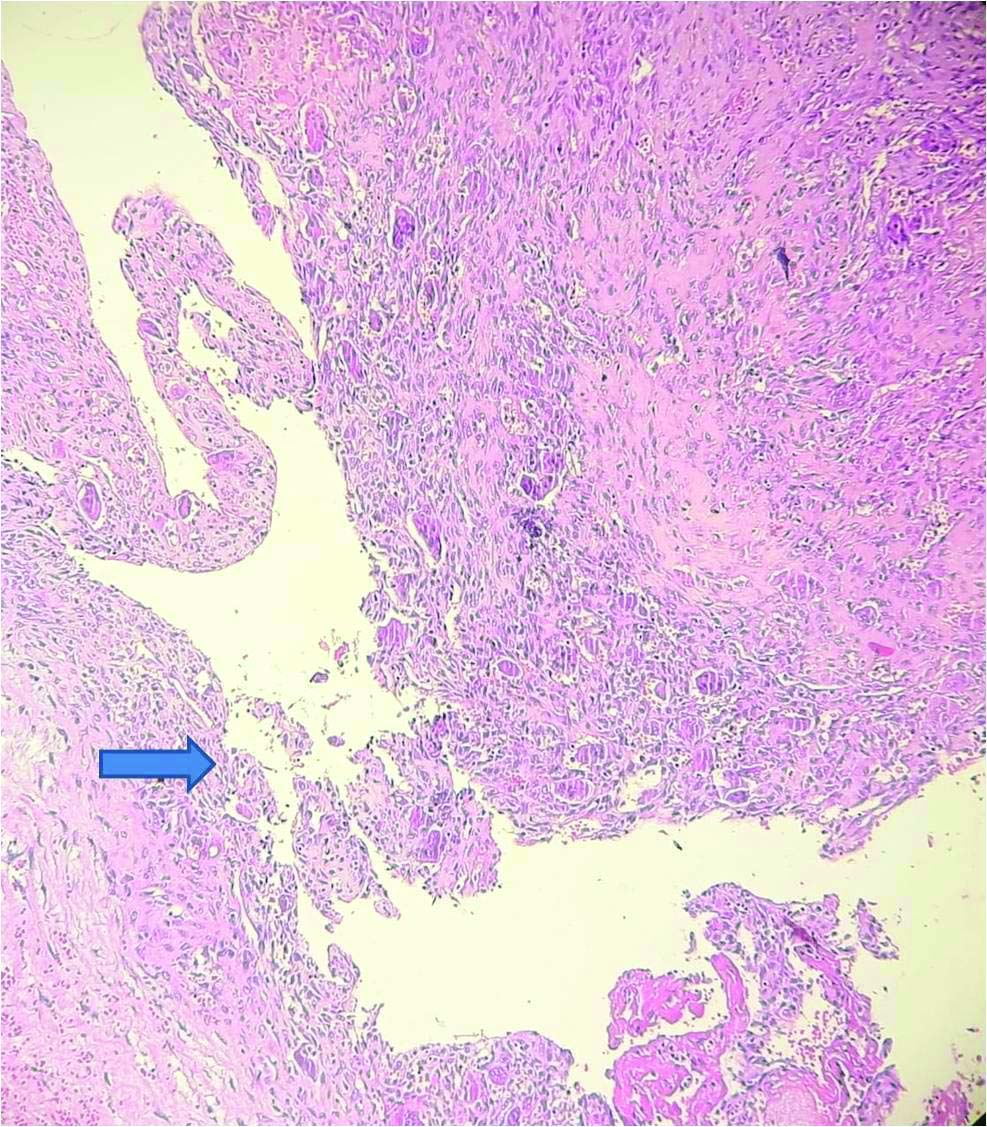
To rule out malignancy, a trucut biopsy was done under ultrasound guidance. It showed cellular tumour with presence of numerous multinucleated giant cells. Back ground showed oval-spindle cells having ill defined cytoplasmic boundaries. No significant nuclear atypia/mitosis was seen in sections. An impression of giant cell tumour of tendon sheath was made on histopathology [Table/Fig-4]. Thus, preoperatively, a diagnostic dilemma with differentials of haemangioma, giant cell tumour and angiomatosis was created.
Microphotograph showing a cellular lesion with vascular space (arrow) lined by numerous multinucleated giant cells . The stroma appears cellular with oval to spindle shaped cells. No significant mitosis was noted (H&E 200X).
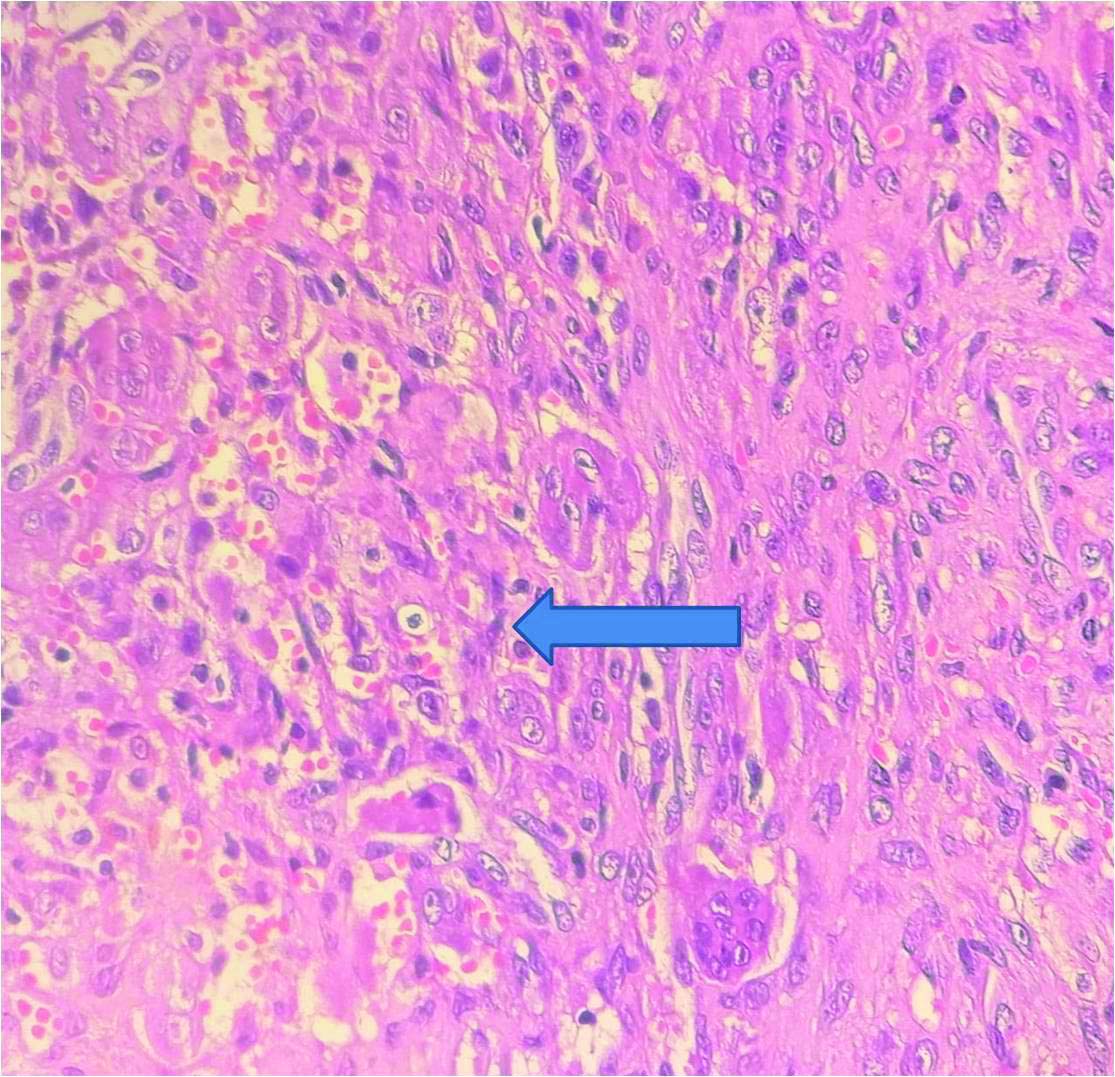
In view of this swelling being between the arterial arches of the palm and extending to the dorsum, the plan of excision the swelling and eroded hamate bone, from the palmer side was made. The chances of injury to the superficial and the deep palmer arch, encasement of tendons and tendon defect reconstruction were well explained to the patient. After taking a well informed preoperative consent, an “S” shaped incision was made over the left hand and excision of the swelling was done under supraclavicular block. The swelling was removed sparing deep palmer arch. The ulnar artery and nerve were identified and preserved [Table/Fig-5]. The eroded hamate bone was removed. Tendons of little and ring finger were found free from the swelling. The tumour was found to have pressure effects on tendons causing difficulty in its sliding moment. Pin prick was arterial in the digits at the end of the surgery and oxygen saturation of all the involved digits was normal. The incision was closed with ethilon 3-0 and the hand was splinted in resting position. The specimen was sent for biopsy. Patient was discharged on 5th postoperative day. To authors surprise, the histopathology of entire lesion came out to be extraosseous Aneurysmal Bone Cyst (ABC) [Table/Fig-6]. On follow-up visits, hand physiotherapy was encouraged for tendon gliding. Close monitoring and regular follow-up was advised by oncologist, to look for any recurrence.
Intraoperative image of superficial palmar arch with swelling beneath it.

Microscopic image showing numerous giant cells (arrow) along with vascular spaces containing red cells (H&E 400X).
Discussion
Aneurysmal Bone Cyst (ABC) is a benign tumour of bone that was first described by Jaffe HL and Lichtenstein L in 1942 [1]. It most frequently develops in the metaphysis of long bones and the posterior elements of vertebral bodies [2]. These swelling are more common in females and in 2nd decade of life. Soft-tissue ABC are rare [3,4]. The first case of soft tissue ABC was reported by Salm R and Sissons HA in 1972 [5].
Among various primary bone lesions of hand, ABCs (osseous or extraosseous) are infrequent and when present, they occur most frequently in the metacarpals [6]. So far, not more than 25 cases of extraosseous ABCs have been reported in literature, out of which palm is a rare site for its occurrence [7]. The most common site of involvement has been described to be lower extremity, followed by the arm and the shoulder. The pathogenesis of ABC is poorly understood. Trauma is not a reported risk factor [7]. There are two types of extraosseous ABCs namely primary and secondary. Primary ABCs have recurrent translocations involving the Ubiquitin Specific Peptidase 6 (USP6) gene where an abnormal expression of this protein leads to tumour growth [8]. Secondary ABCs do not have this genetic anomaly and are believed to be reactive in nature. We presume our case is an example of secondary ABC, which was reactive in nature. There have been reports of the USP6 mutations in cases of myositis ossificans. Lesions diagnosed as myositis ossificans may represent an early form of what may become a cystic ABC [2]. The natural history of ABCs has been documented radiographically [2] with characteristic findings of the bony shell and osseous septa called the "soap bubble appearance” [4]. Pathologically the other differential diagnosis include giant cell tumour of the soft tissue, tenosynovial giant cell tumour, nodular fasciitis, brown tumour of hypoparathyroidism, telangiectatic osteosarcoma and metastatic lesions [9]. In the present case, keeping ABC (extraosseous and osseous) as one of the early diagnosis was difficult because our patient was a 30 years male with post traumatic swelling at hypothenar area. The trucut biospsy probably took the material where giant cells were rich in number. The complete excision specimen clarified the final diagnosis as soft tissue ABC. On final histopathology it show large blood filled cystic spaces surrounded by fibroblastic proliferation along with many multinucleated osteoclast type giant cells and reactive bone formation at the periphery.
The literature demonstrates that extraosseous ABC at other locations are very well diagnosed radiologically. Computed tomography has been suggested to be superior to magnetic resonance for diagnosis, due to heterogenous signals and edema being perceived as an aggressive process on magnetic resonance [10,11]. On CT scan, these cysts are heterogenous in nature due to varying amounts of blood, fluid and fibrous tissue [10]. They may produce a honeycomb appearance on post contrast images if septations are present. Such diagnostic findings were absent in our case perhaps due to unusual site and presentation. On technetium bone scintigraphy [3] there cysts may produce fluid-fluid levels and if mature enough, immature bone may be visualized a “doughnut” sign. This test could not be done in the present patient as the facility is unavaibale in our hospital. In the present case, excision biopsy of swelling was diagnostic to establish the final diagnosis. Sahu A et al., also concluded that excision biopsy is the only means to establish diagnosis of these rare cysts at atypical sites like palm [12].
Due to its rarity, there is a paucity of literature regarding the management of this disease. Surgical excision is the most appropriate management for this swelling [7]. Recent discoveries about the genetic basis of its pathophysiology have allowed us to better understand the disease. A number of anti-cancer agents have been proposed for reducing the size of the swelling and reduce its risk for recurrence but no consensus exists on its use [13]. The astute clinician must rely, not only on clinical and radiological assessment but also on pathological reporting for an accurate diagnosis and management thereafter.
Conclusion(s)
Hand can be one of the rare sites for occurrence of extraosseous aneurysmal bone cyst. Authors strongly recommend excisional biopsy, along with other imaging modalities to reach to a final diagnosis. A complete excision of ABC is the treatment of choice.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 14, 2021
Manual Googling: Aug 26, 2021
iThenticate Software: Sep 14, 2021 (6%)
[1]. Jaffe HL, Lichtenstein L, Solitary unicameral bone cyst: With emphasis on the roentgen picture, the pathologic appearance and the pathogenesisArch Surg 1942 44(6):100410.1001/archsurg.1942.01210240043003 [Google Scholar] [CrossRef]
[2]. Song W, Suurmeijer AJH, Bollen SM, Cleton-Jansen AM, Bovée JVMG, Kroon HM, Soft tissue aneurysmal bone cyst: Six new cases with imaging details, molecular pathology, and review of the literatureSkeletal Radiol 2019 48(7):1059-67.10.1007/s00256-018-3135-x30603771 [Google Scholar] [CrossRef] [PubMed]
[3]. AlAqeel M, Nooh A, Wang CK, Turcotte R, An extraosseous aneurysmal bone cyst in a 59-year-old man: A case report: A case reportJBJS Case Connect 2020 10(2):e049310.2106/JBJS.CC.18.0049332649103 [Google Scholar] [CrossRef] [PubMed]
[4]. Sherman RS, Soong KY, Aneurysmal bone cyst: Its roentgen diagnosisRadiology 1957 68(1):54-64.10.1148/68.1.5413401015 [Google Scholar] [CrossRef] [PubMed]
[5]. Salm R, Sissons HA, Giant-cell tumours of soft tissuesJ Pathol 1972 107(1):27-39.10.1002/path.17110701064262633 [Google Scholar] [CrossRef] [PubMed]
[6]. Platt AJ, Klugman DJ, Aneurysmal bone cyst of the capitateJ Hand Surg Br 1995 20(1):08-11.10.1016/S0266-7681(05)80005-1 [Google Scholar] [CrossRef]
[7]. Hao Y, Wang L, Yan M, Jin F, Ge S, Dai K, Soft tissue aneurysmal bone cyst in a 10-year-old girlOncol Lett 2012 3(3):545-48.10.3892/ol.2011.53022740948 [Google Scholar] [CrossRef] [PubMed]
[8]. Oliveira AM, Hsi BL, Weremowicz S, Rosenberg AE, Dal Cin P, Joseph N, USP6 (Tre2) fusion oncogenes in aneurysmal bone cystCancer Res 2004 64(6):1920-23.10.1158/0008-5472.CAN-03-282715026324 [Google Scholar] [CrossRef] [PubMed]
[9]. Chung IAY, Petelin K, Pižem J, Luzar B, Cutaneous aneurysmal bone cyst-First report of a case and literature reviewJ Cutan Pathol 2019 46(11):858-63.10.1111/cup.1352631206756 [Google Scholar] [CrossRef] [PubMed]
[10]. Reddy O, Gafoor J, Suresh B, Prasad P, Extraosseous aneurysmal bone cyst: A rare presentationJ Dr NTR Univ Health Sci 2014 3(3):19910.4103/2277-8632.140948 [Google Scholar] [CrossRef]
[11]. López-Barea F, Rodríguez-Peralto JL, Burgos-Lizaldez E, Alvarez-Linera J, Sánchez-Herrera S, Primary aneurysmal cyst of soft tissue. Report of a case with ultrastructural and MRI studiesVirchows Arch 1996 428(2):125-29.10.1007/BF001939418925126 [Google Scholar] [CrossRef] [PubMed]
[12]. Sahu A, Gujral SS, Gaur S, Extraosseous aneurysmal cyst in hand: A case reportCases Journal 2008 1:26810.1186/1757-1626-1-26818950488 [Google Scholar] [CrossRef] [PubMed]
[13]. Dubory A, Missenard G, Domont J, Court C, Interest of denosumab for the treatment of giant-cells tumours and aneurysmal bone cysts of the spine. About nine casesSpine (Phila Pa 1976) 2016 41(11):E654-60.10.1097/BRS.000000000000135027244112 [Google Scholar] [CrossRef] [PubMed]