Non Vascularised Fibula Strut Graft Augmentation for Fixation of Proximal Humerus 3-Part Fracture using PHILOS Plate and CC Screws in a Young Male
Amit Supe1, Pranay Kondewar2, Eknath Pawar3, Rohit Topno4, Lalkar Gadod5
1 Orthopaedic Surgeon, Department of Orthopaedics, JJ Hospital, Mumbai, Maharashtra, India.
2 Orthopaedic Trainee, Department of Orthopaedics, JJ Hospital, Mumbai, Maharashtra, India.
3 Head, Department of Orthopaedics, JJ Hospital, Mumbai, Maharashtra, India.
4 Orthopaedic Surgeon, Department of Orthopaedics, JJ Hospital, Mumbai, Maharashtra, India.
5 Orthopaedic Surgeon, Department of Orthopaedics, JJ Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pranay Kondewar, 300 Resident Hostel, Mumbai, Maharashtra, India.
E-mail: pranaypk1@gmail.com
Proximal humerus fracture accounts for 4-5% of all fractures. Locking Compression Plate (LCP) Proximal Humerus Internal Locking System (PHILOS) fixation is currently the most widely used method for the management of unstable proximal humerus fractures. LCP system of the proximal humerus is better than other available implants because of better anatomic design, fixed angulated configuration of locking screws, rotational and angular stability. This case report was of a 35-year-old male who presented with pain, swelling and difficulty in movement at the right shoulder, after a road traffic accident. Plain radiograph of right shoulder (anteroposterior) view revealed displaced 3-part proximal humerus fracture (humeral head with lesser tuberosity, greater tuberosity and shaft). It was managed with philos plate, Cannulated Compression (CC) Screws and non vascularised fibular strut graft. At two years follow-up, patient showed good shoulder range of motion with no complication.
Cannulated compression screw, Construct stiffness, Locking compression plate, Medial comminution, Proximal humerus internal locking system
Case Report
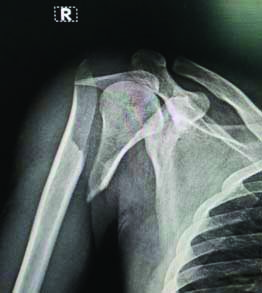
A 35-year-old male presented with pain, swelling and difficulty in movement at the right shoulder for two hours. He had a road traffic accident and sustained trauma to the right shoulder. On physical examination, tenderness, swelling and contusion was present at the right shoulder joint with no wound and distal neurovascular deficit. Plain radiograph of right shoulder (anteroposterior) view revealed displaced 3-part proximal humerus fracture (humeral head with lesser tuberosity, greater tuberosity and shaft) [Table/Fig-1a,b]. A 3D Computed Tomography (CT) scan also showed fracture fragments and medial calcar fracture [Table/Fig-2a,b]. The patient was young, requiring early mobilisation and functions. It was planned augmentation of non vascularised fibular strut graft with Proximal Humerus Internal Locking System (PHILOS) plating and Cannulated Compression (CC) Screws fixation.
X-ray right shoulder (anteroposterior) view showing 3-part proximal humerus fracture with displacement of the fragments.
a) and b) A 3D Computed Tomography (CT) scan images of the right shoulder showing fracture with 3 distinguishing fragments, greater tuberosity, head with lesser tuberosity and shaft.

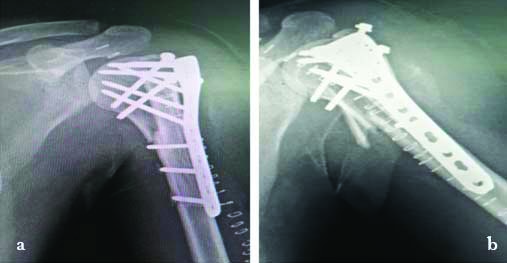
The patient was operated in the beach chair position under general anaesthesia and interscalene block, deltopectoral approach was used, after opening the fracture site there was discontinuity on the medial side. About 8 cm of non vascularised fibular strut graft was harvested from the ipsilateral side using a plane between gastrosoleus and peroneus muscles and 7 cm of distal fibula preserved to prevent the ankle instability. The graft was contoured and telescoped in the shaft, provisional reduction achieved and head fixed with shaft using 2 k wires, 5-0 ethibond non absorbable sutures placed in the tendons of the rotator cuff should be secured to the plate to facilitate compression and counterbalance deforming muscular forces. Tuberosity was fixed with 2 CC screws PHILOS plate was fixed 5 mm below the greater tuberosity and lateral to bicipital groove. Two head screws and one shaft screw was passed through the fibula strut for additional support [Table/Fig-3a,b]. Wound was closed in layers and shoulder immobiliser was given.
a) and b) Immediate postoperative X-rays showing adequate reduction and medial continuity with restored normal neck shaft angle.
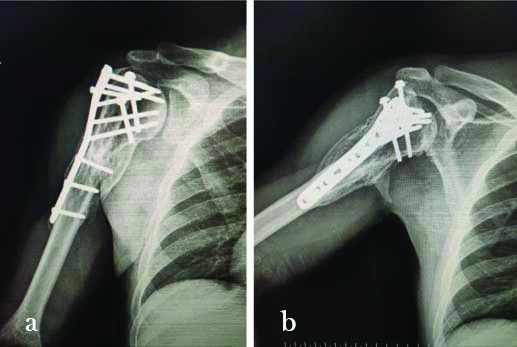
On follow-up pendulum exercises were initiated at postoperative two weeks and increased gradually on further follow-up at two years; the patient was comfortable with no pain and difficulty in abduction and having good shoulder range of motion [Table/Fig-4a-c]. The follow-up X-ray showed union at fracture site and integration of fibular strut graft in shaft and head, there was no evidence of avascular necrosis and head changes on X-rays [Table/Fig-5a,b].
a), b) and c) Two years follow-up clinical picture showing good range of motion and healed scar.

a) and b) two years follow-up X-rays showing abundant callus formation medially on anterior and posterior side, graft is integrated with humerus, there is no varus collapse or head changes in the humerus.
Discussion
Proximal humerus fracture accounts for 4-5% of all fractures. Most of the cases of the fractures seen in elderly population with osteoporosis, result from a low energy trauma; while in the younger age group these are associated with road accident, epilepsy and other high energy trauma [1]. The proximal humerus divided into four anatomical parts based on its epiphyseal lines: the head, the greater tuberosity, the lesser tuberosity, and the proximal shaft. Proximal humerus fracture classified into four types according to Neers CS classification [2]. In this fracture displacement is defined as separation of a fragment >1 cm or angulation of a fragment greater than 45°. The treatment options available for these patients includes philos plate, intramedullary nail, Open Reduction and Internal Fixation (ORIF), shoulder hemiarthroplasty and cannulated cancellous screw fixation. Locking Compression Plate (LCP) (PHILOS) fixation is currently the most widely used method for the management of unstable proximal humerus fractures [3,4]. LCP system of the proximal humerus is better than other available implants because of better anatomic design, fixed angulated configuration of locking screws, rotational and angular stability [5].
According to Bea JH et al., and Mathison C et al., locking compression plating with fibula strut autograft is better when the medial column of proximal humerus collapsed [6,7]. Addition of strut graft increases load capacity and the stiffness of this construct, compared with locking plate alone. Thus, the outcome is better and recovery is early. The strut graft also decreases the movement at the interface.
Maintaining intraoperative reduction and achieving stable fixation is very important aspect in the surgery. Restoration of the medial calcar continuity and support is proven to give good clinical results and reduce the complications like varus collapse and avascular necrosis of head [8,9]. Kim DS et al., reported their experience of treating about 164 patients with 3-part or 4-part proximal humeral fractures with medial comminution using LCP, fibula strut allograft and inferomedial screws. They concluded that strut graft augmentation is an important step in primary surgery for restoration of medial support in 4-part proximal humeral fractures involving medial metaphyseal comminution, along with LCP [10].
Chow RM et al., reported their experience of simulating proximal humerus fracture in cadaver by creating fracture at surgical neck and later it was fixed on one side with LCP and on other side by LCP and fibula strut graft. They found that the combined use of a LCP and fibular allograft could increase the initial stiffness and sustain a higher ultimate failure load [11]. According to Gardner M et al., the fibular strut graft enhances the pull-out strength of the screws of the LCP [12]. In this case, screws also have purchase of cortex of strut graft which gives better stability and early union of fracture. The fibula strut fits in the medullary cavity specially in osteoporotic fractures, preventing abnormal movements at fracture site.
Conclusion(s)
Proximal humerus fracture with posteromedial calcar comminution, metadiaphyseal fracture extension and non union cases are best managed with LCP and fibula strut graft. The use of a fibular strut graft which helps in improvement of construct stiffness and decrease the chances of humeral head screw penetration. It also increases the pull-out strength of the screws and allows early range of motion exercises and thus improved clinical outcome.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 25, 2021
Manual Googling: Aug 04, 2021
iThenticate Software: Sep 18, 2021 (15%)
[1]. Neer CS, Displaced proximal humeral fractures: Part I. Classification and evaluation. 1970Clin Orthop Relat Res 2006 442:77-82.10.1097/01.blo.0000198718.91223.ca16394743 [Google Scholar] [CrossRef] [PubMed]
[2]. Codman E, The Shoulder BostonThomas Todd 1934 :123-77. [Google Scholar]
[3]. Walsh S, Reindl R, Harvey E, Berry G, Beckman L, Steffen T, Biomechanical comparison of a unique locking plate versus a standard plate for internal fixation of proximal humerus fractures in a cadaveric modelClin Biomech (Bristol, Avon) 2006 21(10):1027-31.10.1016/j.clinbiomech.2006.06.00516919375 [Google Scholar] [CrossRef] [PubMed]
[4]. Stableforth PG, Four-part fractures of the neck of the humerusJournal of Bone and Joint Surgery 1984 66:104-08.10.1302/0301-620X.66B1.66934666693466 [Google Scholar] [CrossRef] [PubMed]
[5]. Jung WB, Moon ES, Kim SK, Kovacevic D, Kim MS, Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate?BMC Musculoskeletal Disorders 2013 14(1):01-01.10.1186/1471-2474-14-10223517539 [Google Scholar] [CrossRef] [PubMed]
[6]. Bae JH, Oh JK, Chon CS, Oh CW, Hwang JH, Yoon YC, The biomechanical performance of locking plate fixation with intramedullary fibular strut graft augmentation in the treatment of unstable fractures of the proximal humerusJ Bone Joint Surg Br. British 2011 93(7):937-41.10.1302/0301-620X.93B7.2612521705567 [Google Scholar] [CrossRef] [PubMed]
[7]. Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M, Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograftClinical Biomechanics 2010 25(7):642-46.10.1016/j.clinbiomech.2010.04.00620483189 [Google Scholar] [CrossRef] [PubMed]
[8]. Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS, Predicting failure after surgical fixation of proximal humerus fracturesInjury 2011 42:1283-88.10.1016/j.injury.2011.01.01721310406 [Google Scholar] [CrossRef] [PubMed]
[9]. Lee CW, Shin SJ, Prognostic factors for unstable proximal humeral fractures treated with locking-plate fixationJ Shoulder Elb Surg 2009 18:83-88.10.1016/j.jse.2008.06.01419095180 [Google Scholar] [CrossRef] [PubMed]
[10]. Kim DS, Lee DH, Chun YM, Shin SJ, Which additional augmented fixation procedure decreases surgical failure after proximal humeral fracture with medial comminution: fibular allograft or inferomedial screws?J Shoulder Elb Surg 2018 27(10):S105827461830229510.1016/j.jse.2018.03.02029735375 [Google Scholar] [CrossRef] [PubMed]
[11]. Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ, Proximal humeral fracture fixation: locking plate construct±intramedullary fibular allograftJ Shoulder Elb Surg 2011 21(7):894-901.10.1016/j.jse.2011.04.01521782474 [Google Scholar] [CrossRef] [PubMed]
[12]. Gardner M, Boraiah S, Helfet D, Lorich D, Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implantJ Orthop Trauma 2008 22:195-200.10.1097/BOT.0b013e31815b392218317054 [Google Scholar] [CrossRef] [PubMed]