Case Report
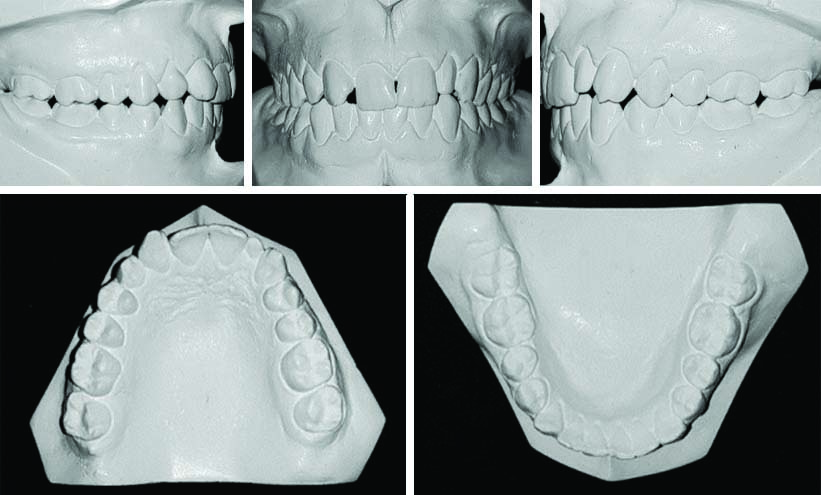
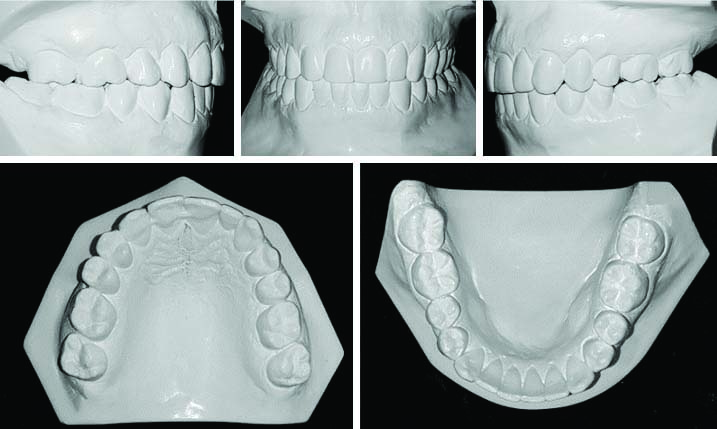
This case described a 18-year-old adult female patient referred by her general practitioner for orthodontic evaluation because of the presence of prolonged retained maxillary right deciduous canine. On examination, she presented with a missing maxillary right lateral incisor, with a permanent canine in its position and a retained deciduous canine in position of the permanent canine. The patient’s initial orthodontic records revealed a convex facial profile and symmetrical face. Her dental arches were in normal parabolic shapes. The maxillary right canine was in place of a missing lateral incisor, maxillary right deciduous canine in place of the permanent canine and was without any signs of mobility. In addition, the maxillary left lateral incisor was a peg-shaped left lateral incisor. Her periodontal examination revealed no bleeding on probing. Her medical and dental histories were noncontributory. There was no history of temporomandibular disorders. Her dental cast analysis showed a Class II, division 1, subdivision malocclusion, both canines (right and left) in Class II relationship with a 2.0 mm overjet and correct overbite on central incisors and an openbite on left lateral incisor, presented a 2.0 mm black space between maxillary central incisors.
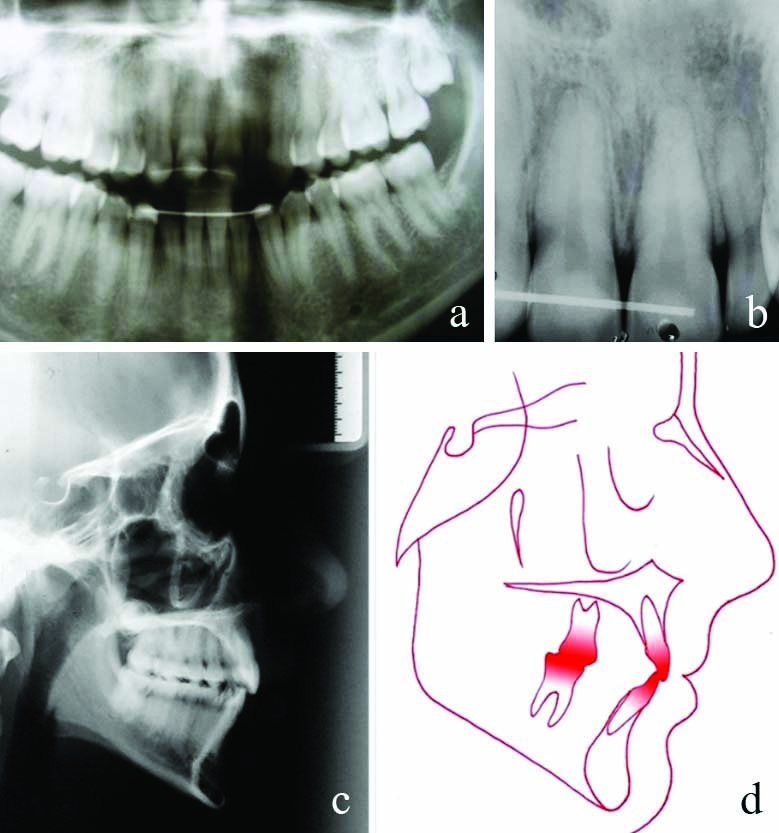
Mandibular midline shifted 3.0 mm to the left in relation to the face. The maxillary and mandibular arches showed a 2.0 mm of misalignment [Table/Fig-1,2]. Panoramic radiographs revealed the absence of a maxillary right lateral incisor, retained maxillary right deciduous canine with satisfactory bone support but with external root resorption in the cervical area, and the presence of maxillary third molars [Table/Fig-3].
Pretreatment facial and intraoral photographs.

Pretreatment examinations: a) panoramic; b) periapical; c) lateral cephalometric film; and d) tracing.
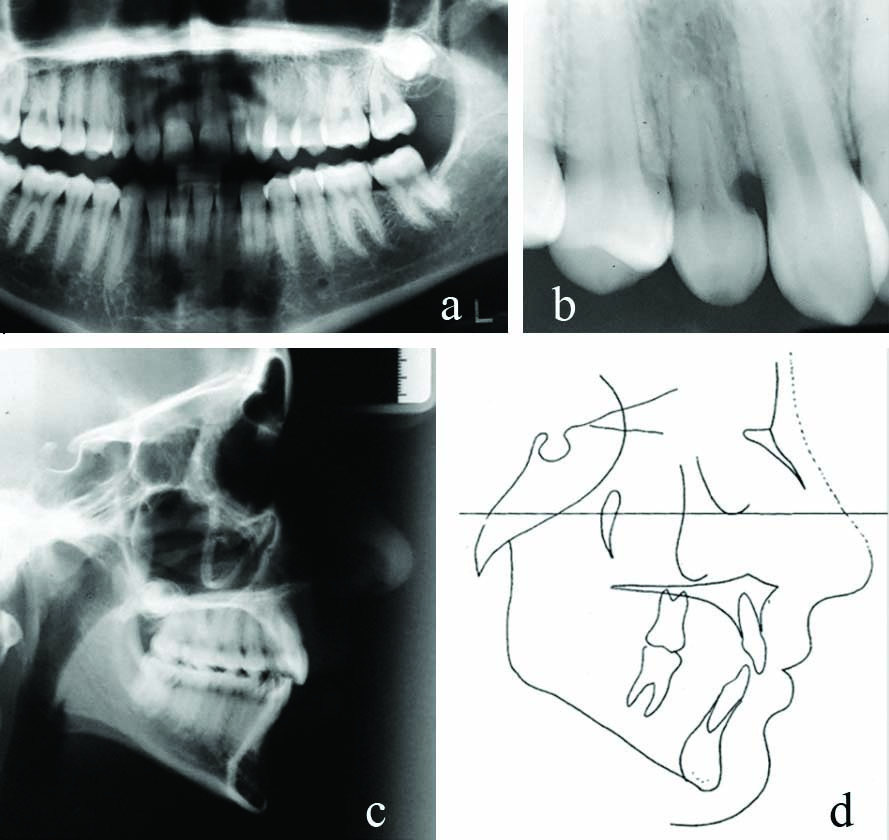
The cephalometric analysis showed a skeletal Class II pattern {A point, nasion, B point (ANB) was 6°}, due to a retrognathic mandible {sella, nasion, B point (SNB) was 74°), palatally inclined maxillary incisor {Angle between upper incisor to NA line (1-NAwas 12°) }, slightly uprighted mandibular incisor {Angle between lower incisor to NB line (1-NB was 21°; Incisor Mandibular Plane Angle (IMPA) was 87°), hyperdivergent growth pattern {Frankfort mandibular angle (FMA) was 33°, Gonion Gnathion to sella-nasion (GoGN-SN) was 37°), with a slightly increased (3.0 mm) lower third of the face [Table/Fig-3,4].
Cephalometric measurements at the beginning of treatment, at the end of treatment, and follow-up.
| Measurements | Normal | Pretreatment | Post-treatment | Follow-up |
|---|
| SNA angle (°) | 82° | 80 | 79 | 79 |
| SNB angle (°) | 80° | 74 | 73 | 73 |
| ANB angle (°) | 2° | 6 | 6 | 6 |
| Facial angle (°) | 87° | 83 | 80 | 80 |
| Convexity (°) | 0° | 10 | 10 | 8 |
| FMA (°) | 25° | 33 | 34 | 33 |
| GoGn-SN) (°) | 32° | 37 | 39 | 39 |
| Y-Axis (°) | 59° | 67 | 69 | 69 |
| 1-NA (mm) | 4 | 2 | 2 | 2 |
| 1-NA (°) | 22° | 12 | 15 | 16 |
| 1-NB (mm) | 4 | 6 | 7 | 7 |
| 1-NB (°) | 25° | 21 | 27 | 25 |
| IMPA (°) | 90° | 87 | 93 | 92 |
| Interincisal angle (°) | 132° | 141 | 134 | 132 |
| Z-angle (°) | 75° | 72 | 71 | 74 |
SNA angle: Sella-Nasion to A Point Angle; SNB angle: Sella-Nasion to B Point Angle; ANB angle: A point to B Point Angle; FMA angle: Frankfort mandibular plane angle; GoGN-SN: Gonion Gnathion to sella-nasion; Y Axis: Sella Gnathion to Frankfurt Horizontal Plane; 1-NA (°): Angle between upper incisor to NA line; 1-NA (mm): Distance from upper incisor to NA line; 1-NB (°): Angle between lower incisor to NB line; 1-NB (mm): Distance from lower incisor to NB line; IMPA (°): Angle between long axis of lower incisor and mandibular plane angle; Z-angle (°): Angle formed by the intersection of FHP and a line connecting soft tissue pogonion and the most protrusive lip point
Treatment Objectives
To restore the missing maxillary right lateral incisor and the peg-shaped left lateral incisor by achieving good alignment and establishing posterior interdigitation with Class I molar and canine relationships on both sides or Class II relationship on the right side in case of closing the agenesis space, with fixed orthodontic appliance. The biomechanics should not promote the extrusion of posterior teeth to avoid the side-effect of a clockwise rotation of the mandible, and further increase the lower third of the face.
Treatment Alternatives
Considering her retrognathic mandible (ANB angle of 6°) and a convex profile, she was satisfied with her familial facial profile. The following treatment alternatives were established:
1) No treatment- to maintain the maxillary deciduous canine until its exfoliation (there is no way to predict how long the deciduous tooth may remain stable); 2) Extract the deciduous canine and distalise the canine into its location and make room for implant placement into the missing lateral site; 3) Extract the deciduous canine and close the spaces by moving the premolars and molars anteriorly closing all spaces; 4) Extract the deciduous canine to replace the permanent canine. Extract the deciduous canine and open space for implant prosthetic rehabilitation between the maxillary first and second right premolars [1].
The alternatives to maintain the maxillary canines in the position of the missing lateral incisors would require reshaping of the permanent canines into lateral incisors, but the patient did not want to have either stripping or reshaping in any teeth. The patient opted to extract the deciduous canine and close the spaces by moving the premolars and molars anteriorly closing all spaces including mesial and distally to the peg-shaped lateral because patient did not want to reshape it.
Treatment Progress
Before orthodontic treatment, the patient was referred to the general practitioner for routine clinical procedures where the advantages and disadvantages were explained, and mainly her compliance in using elastics would be mandatory. The patient chose to extract the deciduous canine and close the spaces by moving the premolars and molars anteriorly closing all spaces. The first archwire was tied after bonding brackets in the maxillary arch.
A fixed orthodontic appliance 0.022″ × 0.028″ (inches) edgewise standard brackets (Morelli Ortodontia) were bonded in all teeth, except the mandibular second molar which was banded for application of intrusion movement to avoid clockwise rotation of the mandible. The initial levelling and alignment sequence of arches were 0.014″, 0.016″ (inches) NiTi ((Morelli Ortodontia), 0.016″ × 0.022″ (inches) rectangular Stainless Steel (SS) archwires (Morelli Ortodontia) were used for alignment and leveling.
A 0.017″ × 0.025″ (inches) SS archwires (Morelli Ortodontia) were used do add third order bend to move the maxillary right canine palatally to mimic the lateral incisor. The wires were changed approximately one month intervals, and she had about thirty consultation appointments to finish the treatment.
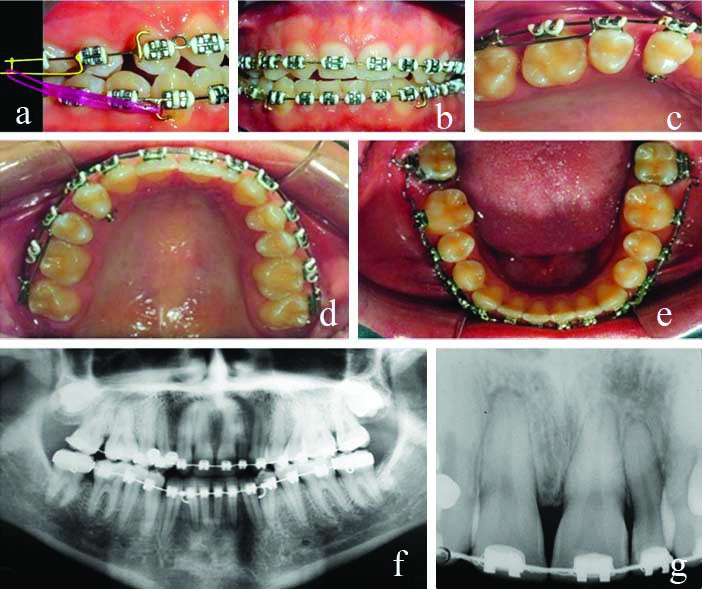
To loose anchorage and move the maxillary right quadrant mesially, a brass wire spurs were welded between the first and right first premolars and canines, and flush in the distal of the maxillary right first premolar in a 0.019" x 0.026" (inches) TP orthodontics SS archwire.
Sliding jig mechanics with Class III ¼ intermaxillary elastics (about 100 g/f) (Morelli Ortodontia) from the brass wire spur soldered distal of the mandibular right canine [Table/Fig-5], in conjunction with a triangular vertical elastics (about 50 g/f) from maxillary right canine and lateral incisor to mandibular right canine, and short elastic chains from first to second bicuspids (Morelli Ortodontia) on the right side were used.
Progress. a,b) Sliding jig in conjunction with Class III intermaxillary elastics pushing the second premolar mesially; c) close view of the spaces between both molars; d,e) maxillary and mandibular arches; f) panoramic; and g) periapical radiographs.
Treatment Results
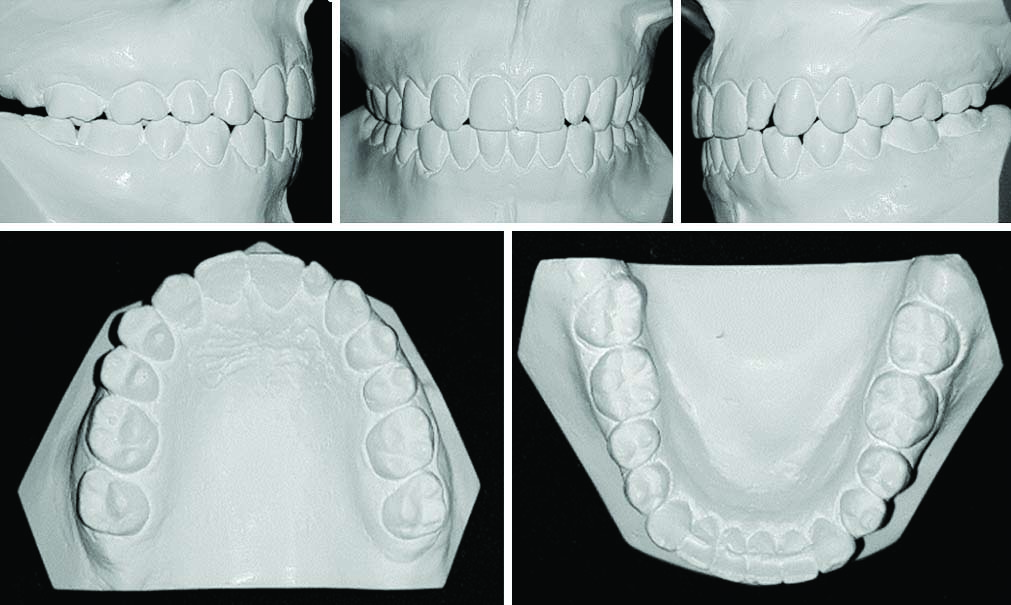
After 38 months of active treatment, the planned results were obtained and the brackets and bands were removed, a segment of 0.017"×0.025" (inches) braided wire was bonded in both maxillary central incisors and right canine associated with a wrap around type removable appliance. A mandibular cuspid to cuspid 0.028" (inches) SS wire (Morelli Ortodontia) was fixed as a retainer. Post-treatment facial photographs showed the maintenance of a balanced profile with a pleasant smile [Table/Fig-6]. The patient was referred to her general dentist for an improvement reshaping and/or performing a bleaching of the colour in the right canine, although she was satisfied with the shape of the maxillary right canine and left peg-shaped lateral incisor since the beginning the treatment for personal reasons.
Post-treatment facial and intraoral photographs.

A molar Class relationship was maintained on the left side and a Class II molar relationship was established on the right side.
Both arches were aligned and levelled, good overbite and overjet were achieved, and her mandibular dental midlines were deviated 2.0 mm to the left.
To perform the coincidence of maxillary midline, the canine should be reshaped in its width to resemble a lateral incisor, move both central incisors to the right side, open space for reshaping to increase the left lateral incisor. To achieve the maxillary and mandibular coincidence it was necessary to move both central incisors to the right side but this was not performed [Table/Fig-7]. She was referred to her general dentist for extraction of the maxillary third molars.
Post-treatment dental casts.
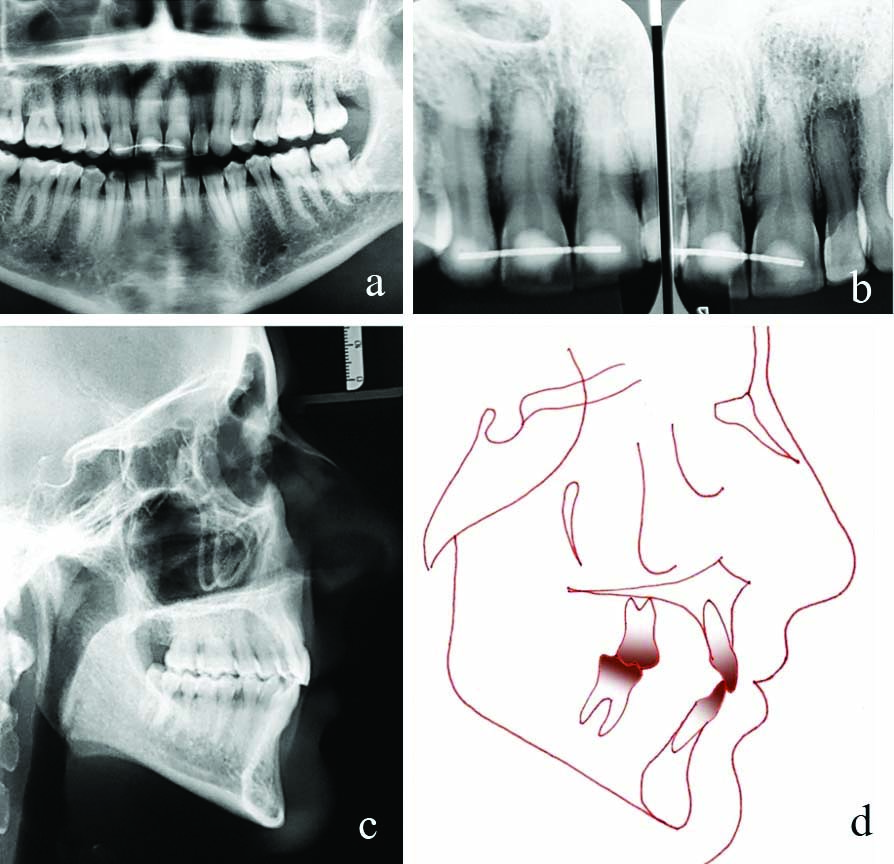
The post-treatment periapical and panoramic radiograph showed appropriate space closure and acceptable root parallelism. There were no significant signs of bone or root resorption when compared with the pretreatment panoramic radiograph [Table/Fig-8]. The post-treatment lateral cephalometric analysis showed no significant skeletal changes (ANB was 6°, SN-GoGn was 39°). The maxillary (1-NB was 15°) and mandibular incisor showed a slight proclination (1-NB was 15°; IMPA was 93°) [Table/Fig-4]. At the 5.9 years retention examination, there was no relapse with good gingival, periodontal health and stability of occlusal outcome [Table/Fig-9].
Post-treatment radiographs: a) panoramic; b) periapical; c) lateral cephalometric; and d) tracing.
A 5.9 years follow-up facial and intraoral photographs.

The patient got the maxillary right canine and left lateral incisor reshaped with composite resin after the 5.9 years follow-up [Table/Fig-9].
The treatment results were well maintained, with good occlusion and aesthetics after 15.8 years at the end of active treatment. Authors observed a slight marginal gingivitis in the now restored maxillary left lateral incisor, and she was referred to her dentist to check the buildup around the lateral incisor.
However, the posterior teeth intercuspation remained excellent, and the patient’s satisfaction remained with high self-esteem [Table/Fig-10,11]. The panoramic radiograph showed the maintenance of health bone and root morphology [Table/Fig-12].
A 15.8 years follow-up facial and intraoral photographs.

A 15.8 years follow-up casts.
A 15.8 years follow-up radiographs: a) panoramic; b) periapical; c) lateral cephalometric; and d) tracing.
Discussion
This case report presented a case with long term stability of the closing space by moving the maxillary right quadrant with sliding jig mechanics toward the midline to achieve the functional and aesthetic results in a young patient with missing maxillary lateral incisor. In her situation, what would be the ideal treatment? Would it have been the maintenance with crown lengthening of the deciduous canine, and porcelain veener in the permanent canine [2]. Alternatively, shorten the treatment time using implant prosthesis rehabilitation in place of canines [3].
The main advantages of closing the maxillary canine deciduous space and moving the posterior teeth mesially was a lower treatment cost because implants or prosthetic replacements were not required. One disadvantage was the difference in the maxillary right canine and maxillary left maxillary lateral incisor, but the patient had no complaint about this issue.
Because of high incidence of agenesis and its prominence in the aesthetic zone, the maxillary lateral incisor is arguably the most frequently restored or replaced missing tooth [4]. Three common treatment options for replacing this tooth are canine substitution (space closure), a tooth supported resin bonded fixed dental prosthesis, or a single implant. Auto transplantation, a less common approach, has also been reported to be a successful and cost effective alternative [5,6]. The option with the best long term aesthetic and functional outcome should be the treatment of choice.
The missing maxillary lateral incisors are not always bilateral. However, it is not rare to find peg-shaped lateral incisors when the contralateral incisor is congenitally missing [7], which was also observed in the current clinical case. The peg-shaped laterals are predominantly genetically determined and can also be caused due to endocrinal disturbances [8]. If the agenesis occurs in skeletal Class I or Class III patients, the conventional protocol is to maintain the conically shaped incisor, which subsequently undergoes prosthetic or conservative recontouring [9], as in the current clinical case.
In the current clinical case, it should be emphasised that the closing space biomechanical control, with sliding jig, combined with a high patient compliance in using intermaxillary elastics were some of the essentials in establishing a Class II relationship in the right side, proper overbite and overjet, occlusal contacts in all teeth, and a coincident centric relation with centric occlusion. The forces applied ranged between 50 cN and 100 cN with patient comfort, and potentially exhibiting fewer side effects [10].
About the Class II relationship in some Class II malocclusions, the molars could be finished without unfavorable collateral effects [11], and there is no evidence for implications for treatment stability [12]. Another issue is the first premolar in the canine position. If desired, even a “canine-protected” occlusion can be established with the buildup on the first premolar, or the first premolar can be intruded during orthodontic treatment to move the gingival margin apically and built up incisally with hybrid composite [13]. Our patient did not want to perform either intrusion or buildup once she started the treatment.
Tuverson DL has treated cases closing spaces for missing maxillary lateral incisors that provided long term results that are as good as [14], or superior to, treatment with space opening for prosthetic replacements [15]. Progress in orthodontics and restorative treatments evidenced that quality treatment can be reached matching proper orthodontics and recent advances in aesthetic dentistry [16].
There is no clear evidence relating patients submitted to orthodontic space opening and prosthetic replacements have long term better results than those treated with orthodontic space closure. According to Zachrisson BU and Stenvik A the question to be answered by some controlled clinical studies is what is preferable in a life-long perspective for the patient, either a natural “living” root or an ankylosed foreign body in the site of the missing maxillary lateral incisor [13]. This was answered by Rosa M et al., who concluded that when referring to TMJ problems and periodontal tissue deterioration, orthodontic space closure in patients with missing lateral incisors does not bring risks for those regions, including intrusion and extrusion of the canine [17].
The main challenge of the treatment is to plan according to the patient’s diagnosis and needs, no assumption such as that implants are superior when compared to orthodontically positioned and reshaped natural teeth should be taken and all the options must be considered. The current clinical case presented a successful outcome in the long term not only in dental relation, gingival, and alveolar architecture but mainly because the patient’s opinion and expectations in canine substitution and maintaining the peg-shaped lateral were fully considered to her satisfaction. One limitation was the difficulty to achieve the midline coincidence.
The major advantages in closing spaces with canine substitution are seen in the present case report after 15-years and 8-months follow-up permanent and biologically compatible results, eliminating the need for prosthetic and/or implants or aesthetic maintenance. In contemporary orthodontics with the use of Temporary Anchorage Devices (TADs) the patient compliance is not needed in using intermaxillary elastics.
Conclusion(s)
The results achieved in this case, as shown by the 15-year 8-months follow-up examination, in terms of the patient’s clinical, radiographic, and psychological aspects, lead to the conclusion that the conservative approach was predictable. The movement of all maxillary right posterior teeth to mesial for closing the missing lateral space and restoration treatment of peg-shaped left lateral incisor achieved a stable result with gingival and periodontal health and good dental and functional occlusion, in a long term follow-up.
SNA angle: Sella-Nasion to A Point Angle; SNB angle: Sella-Nasion to B Point Angle; ANB angle: A point to B Point Angle; FMA angle: Frankfort mandibular plane angle; GoGN-SN: Gonion Gnathion to sella-nasion; Y Axis: Sella Gnathion to Frankfurt Horizontal Plane; 1-NA (°): Angle between upper incisor to NA line; 1-NA (mm): Distance from upper incisor to NA line; 1-NB (°): Angle between lower incisor to NB line; 1-NB (mm): Distance from lower incisor to NB line; IMPA (°): Angle between long axis of lower incisor and mandibular plane angle; Z-angle (°): Angle formed by the intersection of FHP and a line connecting soft tissue pogonion and the most protrusive lip point
[1]. Tanaka OM, Guimarães LK, Bastos SQ, Miyoshi CS, Niwa MF, An orthodontic-prosthetic approach for a missing maxillary lateral incisorJ Clin Diagn Res 2020 14:ZD03-06.10.7860/JCDR/2020/42655.13411 [Google Scholar] [CrossRef]
[2]. Lameira C, Mestrener SR, Pini N, Salomao FM, Pesqueira AA, Fagundes TC, Conservative approach for treatment of maxillary lateral incisor agenesis with the deciduous tooth retained: 18-month follow-upOper Dent 2018 43(2):121-27.10.2341/17-015-T29337645 [Google Scholar] [CrossRef] [PubMed]
[3]. Bizetto MS, Tessarollo FR, Jimenez EE, Guariza-Filho O, Camargo ES, Tanaka OM, Implant rehabilitation of canines in case of bilaterally missing maxillary lateral incisorsAm J Orthod Dentofacial Orthop 2013 144(1):110-18.10.1016/j.ajodo.2012.06.02023810052 [Google Scholar] [CrossRef] [PubMed]
[4]. Priest G, The treatment dilemma of missing maxillary lateral incisors-Part I: Canine substitution and resin-bonded fixed dental prosthesesJ Esthet Restor Dent 2019 31(4):311-18.10.1111/jerd.1248431033185 [Google Scholar] [CrossRef] [PubMed]
[5]. Simeone P, De Paoli C, De Paoli S, Leofreddi G, Sgro S, Interdisciplinary treatment planning for single-tooth restorations in the esthetic zoneJ Esthet Restor Dent 2007 19(2):79-88.discussion 910.1111/j.1708-8240.2007.00071.x17374112 [Google Scholar] [CrossRef] [PubMed]
[6]. Forgie AH, Thind BS, Larmour CJ, Mossey PA, Stirrups DR, Management of hypodontia: Restorative considerations. Part IIIQuintessence Int 2005 36(6):437-45. [Google Scholar]
[7]. Buyuk SK, Ozkan S, Benkli YA, Arslan A, Celik E, Evaluation of the skeletal and dental effects in orthodontic patients with maxillary lateral incisor agenesisJ Esthet Restor Dent 2017 29(4):284-90.10.1111/jerd.1230628560844 [Google Scholar] [CrossRef] [PubMed]
[8]. Chanchala HP, Nandlal B, Coexistent peg-shaped mandibular central incisors along with maxillary lateral incisors: A rare caseInt J Oral Maxillofac Pathol 2012 3:65-68. [Google Scholar]
[9]. Amm EW, Antoszewska-Smith J, Boley J, Canine substitution of congenitally missing maxillary lateral incisors in Class I and Class III malocclusions by using skeletal anchorageAm J Orthod Dentofacial Orthop 2019 156(4):512-21 e6.10.1016/j.ajodo.2018.10.02731582123 [Google Scholar] [CrossRef] [PubMed]
[10]. Theodorou CI, Kuijpers-Jagtman AM, Bronkhorst EM, Wagener F, Optimal force magnitude for bodily orthodontic tooth movement with fixed appliances: A systematic reviewAm J Orthod Dentofacial Orthop 2019 156(5):582-92.10.1016/j.ajodo.2019.05.01131677666 [Google Scholar] [CrossRef] [PubMed]
[11]. Bishara SE, Cummins DM, Jakobsen JR, The morphologic basis for the extraction decision in Class II, division 1 malocclusions: A comparative studyAm J Orthod Dentofacial Orthop 1995 107(2):129-35.10.1016/S0889-5406(95)70127-3 [Google Scholar] [CrossRef]
[12]. Owman G, Bjerklin K, Kurol J, Mandibular incisor stability after orthodontic treatment in the upper archEur J Orthod 1989 11(4):341-50.10.1093/oxfordjournals.ejo.a0360052591482 [Google Scholar] [CrossRef] [PubMed]
[13]. Zachrisson BU, Stenvik A, Single implants-optimal therapy for missing lateral incisors?Am J Orthod Dentofacial Orthop 2004 126(6):A13-15. [Google Scholar]
[14]. Tuverson DL, Close space to treat missing lateral incisorsAm J Orthod Dentofacial Orthop 2004 125(5):17A10.1016/j.ajodo.2003.12.01114765049 [Google Scholar] [CrossRef] [PubMed]
[15]. Thordarson A, Zachrisson BU, Mjor IA, Remodeling of canines to the shape of lateral incisors by grinding: A long-term clinical and radiographic evaluationAm J Orthod Dentofacial Orthop 1991 100(2):123-32.10.1016/S0889-5406(05)81519-7 [Google Scholar] [CrossRef]
[16]. Rosa M, Zachrisson BU, Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisorsJ Clin Orthod 2001 35(4):221-34. [Google Scholar]
[17]. Rosa M, Lucchi P, Ferrari S, Zachrisson BU, Caprioglio A, Congenitally missing maxillary lateral incisors: Long-term periodontal and functional evaluation after orthodontic space closure with first premolar intrusion and canine extrusionAm J Orthod Dentofacial Orthop 2016 149(3):339-48.10.1016/j.ajodo.2015.08.01626926021 [Google Scholar] [CrossRef] [PubMed]