Recurrent Thymoma Mimicking T-Lymphoblastic Lymphoma: An Unusual Case Presentation
Kalasamudram Sravani1, Pranabandhu Das2, Bala Venkat Subramanian3, TC Kalawat4, Nandyala Rukmangadha5
1 Junior Resident, Department of Radiation Oncology, Sri Venkatewara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
2 Associate Professor, Department of Radiation Oncology, Sri Venkatewara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
3 Professor, Department of Radiation Oncology, Sri Venkatewara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
4 Professor, Department of Nuclear Medicine, Sri Venkatewara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
5 Professor, Department of Pathology, Sri Venkatewara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bala Venkat Subramanian, Professor, Department of Radiation Oncology, SVIMS University Cancer Centre, Tirupati, Andhra Pradesh, India.
E-mail: ravibalasubramanian@hotmail.com
Thymoma and T-Lymphoblastic Lymphomas (T-LBL) are primary mediastinal neoplasms that can have similar clinical presentations and overlapping histological features. Because of immature lymphocytes associated with thymoma, it may resemble T-LBL. In this present case report, a 20-year-old male patient with recurrent unresectable thymoma has received definitive chemoradiation therapy. Significant reduction of gross tumour volume was observed while patient underwent weekly image verification before radiotherapy at the end of fourth week, causing the suspicious about the possibility of a highly radiosensitive tumour in mediastinum like lymphoma or extragonadal germ cell tumour. External review of immumohistochemistry features were suggestive of T-LBL.
Common carotid artery, Immunohistochemistry, Trachea
Case Report
A 20-year-old male initially evaluated at Department of General Surgery for complaint of swelling over front of the neck since two months which gradually increased in size. He also complaint of mild difficulty in breathing and swallowing. Contrast Enhanced Computed Tomography (CECT) neck showed well-defined hypodense poorly enhancing lesion in superior mediastinum at retrosternal region measuring 6x5.7x4.2 cm indenting over left brachiocephalic vein/ Superior Vena Cava (SVC) and anterior trachea and there was no evidence of cervical lymphadenopathy.
Fine Needle Aspiration Cytology (FNAC) showed lymphocytic population of cells in sheets and discretely and individual cells having round nucleus with granular chromatin with scanty amount of cytoplasm. Few large atypical lymphocytes in a proteinaceous background and no evidence of thyroid follicular cells and the features suggestive of thymoma. Thereafter, patient underwent thoracotomy and excision of lesion and postoperative histopathology was reported as thymoma type A.
Ultrasound neck was done one and half month after surgery for similar complaint, which showed large ill-defined organised hypoechoic collection in superior and anterior mediastinum on left side extending into left side of neck with few low lying internal echoes and thin internal septae measuring 6.3×4.4×6.4 cms pushing trachea to right side and encasing left common carotid artery. FNAC was suggestive of recurrence of thymoma. Immunohistochemistry (IHC) showed PanCK stained positive cells. CD45, CD3 positive, CD20 positive in scattered small clumps, CD99 and Tdt negative, Ki-67 was negative, suggestive of thymoma type B1.
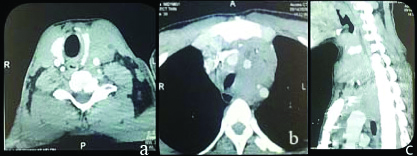
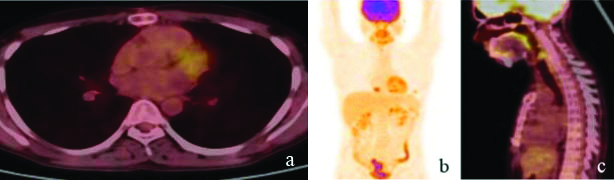
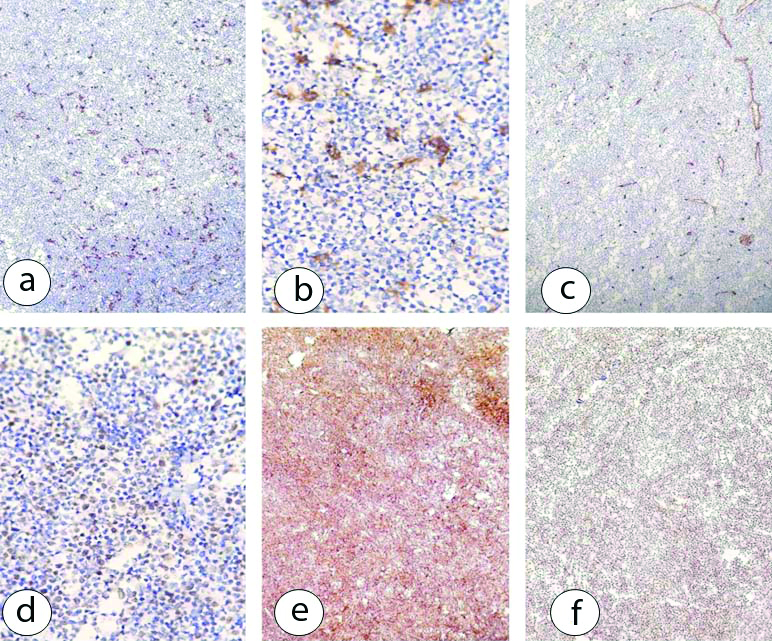
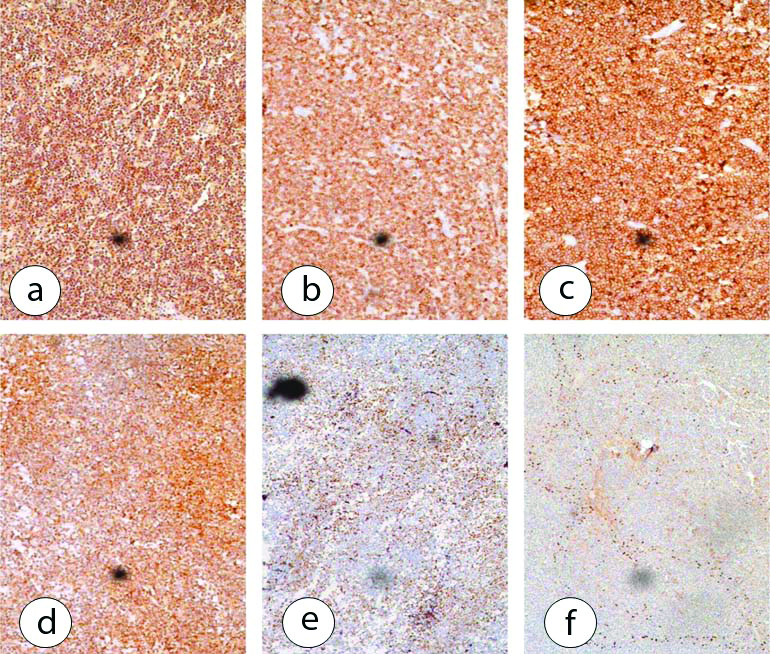
Patient was referred to present centre for further management. Histopathology slide review was advised at present centre and was reported to be thymoma type B2. CT neck [Table/Fig-1] showed mild homogenously enhancing isodense mass lesion measuring 11.2×6.3×5.0 cm seen in left prevascular space of superior mediastinum extending superiorly into infrahyoid neck space. Inferiorly the lesion abutting the arch of aorta encasing left branches of arch of aorta. Medially, the lesion is seen to have encase and displaced trachea and oesophagus to right. Superiorly, the lesion is seen extending upto superior pole of left lobe of thyroid. Laterally, the lesion is seen beneath sternocleidomastoid muscle on left side, the above features were in favour of anterior mediastinal mass likely thymoma. Because of inoperability, patient was planned for definitive radiotherapy with total dose of 60 Gy in 30 fractions at 2 Gy per fraction by Intensity Modulated Radiation Therapy (IMRT) along with four cycles of concurrent weekly cisplatin (40 mg/m2) chemotherapy. During image verification at the end of fourth week by kiloVoltage Cone Beam Computed Tomography (kV-CBCT), patient was found to have significant reduction in the gross tumour volume, which has raised the suspicion regarding possibility of highly radiosensitive tumour like lymphoma such as T-LBL which is not uncommon in such location. External review for a second opinion and immunohistochemical study was suggested along with whole body Positron Emission Tomography and Computed Tomography (PET-CT) scan. The PET-CT showed no abnormal metabolic activity at primary treated site in anterior mediastinum. The [Table/Fig-2] and IHCs (Tdt patchy moderate to intense nuclear positivity in T-lymphocytes. CD5, CD10 and CD20 membranous cytoplasmic positivity, P63 patchy and intense positivity in epithelial cells. CK5 and CK6 patchy intense cytoplasmic positivity in epithelial cells. Ki67% ≤20% cells are showing moderate to intense nuclear positivity in epithelial cells, LCA-intense positivity in lymphocytes, P63-scattered individual cells are showing moderated to intense nuclear positivity, CD34-positive in blood vessels) were done and reported as thymoma type B2 [Table/Fig-3]. External block review IHCs (the lymphoid cell express CD3, CD5, Tdt, CD1a, and CD10. Immunogenic expression for CD20. Ki-67 proliferative index was 70% is highest proliferating areas. Pancytokeratin and P63 are positive in entrapped thymic epithelial cells) suggestive of T-Lymphoblastic lymphoma [Table/Fig-4]. The patient was subsequently delivered the remaining doses of radiation therapy to a total dose of 60 Gy in 30 fractions. Eight weeks after completion of radiation therapy patient was advised to attend medical oncology for initiation for further management. Presently, the patient is on chemotherapy.
CECT neck and chest showed mass present in left prevascular space of superior mediastinum; a) Axial section of CT- superior extension upto superior pole of left lobe of thyroid; b) Inferiorly lesion abutting the arch of aorta; c) Sagittal section of CT.
Whole body PET-CT scan (a) Axial; b) Coronal; c) Sagittal sections showed no evidence of abnormal metabolic activity at anterior mediastinum.
a&b) CD20-Intense membranous positivity seen in scattered B-lymphocytes (IHC, 10x); c) CD34-positive in blood vessels (IHC, 10x); d) Ki67-≤20% of lesional cells are showing moderate to intense nuclear positivity (IHC, 10x); e) LCA-Intense positivity in lymphocytes (IHC, 10x); f) TDT-Moderate to intense nuclear positivity in T-lymphocytes (IHC, 10x).
External review IHCs: a) CD5; b) Ki67; c) P63; d) CD3; e) CD1a; and f) CD10 (IHC, 10x).
Discussion
T-Lymphoblastic Lymphomas are primary mediastinal neoplasms that can have similar clinical presentations. Thymomas are epithelial tumours associated with an exuberant lymphoid component composed of immature cortical thymocytes and are more indolent neoplasms arising in middle aged patients [1]. In contrast T-LBL is a neoplasm of immature T-lymphoblasts which usually occurs as a mediastinal mass or lymphadenopathy in young men in their teens to early twenties [2]. Microscopic distinction between thymoma and T-LBL is sometimes difficult because the immature lymphocytes associated with thymoma may resemble those in T-LBL, both morphologically and immunohistochemically. An accurate diagnosis is critical since the two entities carry distinct prognosis and their management includes different therapeutic approaches. Surgery is the mainstay of management in thymoma while systemic chemotherapy is recommended for management of T-LBL [3].
The present case has been staged as per the WHO histological classification system as thymoma type B2. Thymoma type AB, B1, and B2 are associated with abundant T-lymphocytes [4]. In recurrent thymoma, aggressive local approaches to localised recurrent disease may result in prolonged survival in carefully selected patients. Isolated resectable recurrent tumours are treated by complete surgical resection with or without radiation therapy and unresectable recurrent tumours are treated with definitive RT or Stereotactic Body Radiation Therapy (SBRT) [5]. In present case, the tumour was potentially unresectable, so that patient has been planned for external beam radiation therapy along with concurrent cisplatin chemotherapy. In a patient with a mediastinal mass, the differential diagnosis of lymphocyte rich thymoma versus T-LBL can be challenging. Immunohistochemical study is an important tool in differentiating T-LBL from thymoma by distinguishing thymocytes from T-LBL lymphoblasts. Features favouring T-LBL over thymoma include a tight cluster of lymphoblasts positive for CD45, frequent co-expression of CD10 and/or CD34, and lack of discrete subpopulations or smearing patterns for CD45 and CD3 typically seen in thymomas [6,7]. The lymphoid cells of T-LBL can express CD3, CD5, TDT, CD1a and CD10. Pan-cytokeratin, p63, and Ki67 index, which can be useful in identifying and differentiating thymomas from T-LBL. There may be a chance of abundant T-cell thymoma mimicking the lymphoma.
Initially, the case was treated at outside facility as thymoma. After, that patient developed recurrence within one and half month after surgery. FNAC and IHCs (positive PanCK, CD45, CD3, CD20. CD99, Tdt and Ki-67 were negative) were done and reported as thymoma type B1. Because of unresectability of tumour at the time of recurrence patient has been planned for definitive concurrent chemoradiotherapy. In the present case, the unexpectedly high radiosensitivity of mediastinal tumour which was evident during the course of radiotherapy by regular weekly CBCT image verification technique. This has prompted for an external review in order to exclude a potential co-existence of a lymphoma.
In this present case, we did panel of IHCs for both thymoma and T-LBL. Thymoma panel included Tdt, CD5, CD10, CD20, P63, CK5, CK6, LCA, and Ki67%. External IHC review showed the lymphoid cell expresses CD3, CD5, Tdt, CD1a, and CD10. Immunogenic for CD20 Ki-67 proliferative index was 70% is highest proliferating areas. Pancytokeratin and P63 are positive in entrapped thymic epithelial cells and the features suggestive of T-TBL.
Initially, the above markers were not taken into consideration, so we have treated this case as recurrent unresectable thymoma with external beam radiation therapy with total dose of 60 Gy in 30 fractions at 2 Gy per fraction by IMRT along with concurrent weekly cisplatin chemotherapy. During image verification at the end of fourth week by kV-CBCT he was found to have significant reduction in the gross tumour volume, which results in the suspicious regarding possibility of highly radiosensitive tumour like lymphoma. Hence, if T-LBL is suspected, further histological examination such as external review and IHC of the regressed specimen should be sought to differentiate this from thymoma, which appeared as the cornerstone in management of the present case.
Conclusion(s)
In a scenario of the superior mediastinal mass such as thymoma, the possibilities of lymphoma to be contemplated by its usually an anticipated nature of high radiosensitivity during the course of treatment. Thereby, demands prompt interventions such as external review with extensive IHC panels as well as functional imaging (whole body PET-CT scan) as part of clinical interventions even during the course of treatment to reach at proper diagnosis and further management.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 08, 2021
Manual Googling: Jul 30, 2021
iThenticate Software: Aug 28, 2021 (6%)
[1]. Safieddine N, Liu G, Cuningham K, Ming T, Hwang D, Brade A, Prognostic factors for cure, recurrence and long-term survival after surgical resection of thymomaJournal of Thoracic Oncology 2014 1 9(7):1018-22.10.1097/JTO.000000000000021524926546 [Google Scholar] [CrossRef] [PubMed]
[2]. Chiaretti S, Vitale A, Cazzaniga G, Orlando SM, Silvestri D, Fazi P, Clinico-biological features of 5202 patients with acute lymphoblastic leukemia enrolled in the Italian AIEOP and GIMEMA protocols and stratified in age cohortsHaematologica 2013 98(11):170210.3324/haematol.2012.08043223716539 [Google Scholar] [CrossRef] [PubMed]
[3]. Ito J, Yoshida A, Maeshima AM, Nakagawa K, Watanabe SI, Kobayashi Y, Concurrent thymoma, thymic carcinoma, and T lymphoblastic leukemia/lymphoma in an anterior mediastinal massPathology-Research and Practice 2015 211(9):693-96.10.1016/j.prp.2015.06.00226150396 [Google Scholar] [CrossRef] [PubMed]
[4]. Board PD, PDQ Cancer Information SummariesPDQ Adult Treatment Editorial Board- National Cancer Institute 2002 [Google Scholar]
[5]. Falkson CB, Bezjak A, Darling G, Gregg R, Malthaner R, Maziak DE, The management of thymoma: a systematic review and practice guidelineJournal of Thoracic Oncology 2009 1 4(7):911-19.10.1097/JTO.0b013e3181a4b8e019557895 [Google Scholar] [CrossRef] [PubMed]
[6]. Boddu P, Thakral B, Alhuraiji A, Pemmaraju N, Kadia T, Ohanian M, Distinguishing thymoma from T-lymphoblastic leukaemia/lymphoma: A case-based evaluationJournal of Clinical Pathology 2019 72(3):251-57.10.1136/jclinpath-2018-20539930467242 [Google Scholar] [CrossRef] [PubMed]
[7]. Rovera F, Billo P, Capella C, Dominioni L, Concurrent epithelial thymoma and T-cell lymphoblastic lymphomaInteractive Cardiovascular and Thoracic Surgery 2003 2(4):537-40.10.1016/S1569-9293(03)00136-1 [Google Scholar] [CrossRef]