Obesity has become a public issue that affects health and quality of life, thus increasing healthcare costs worldwide. The health encumbrance of obesity is mainly driven by a higher risk of Non-Communicable Diseases (NCDs), such as hypertension, types 2 diabetes, Cardiovascular Diseases (CVD), and certain type of cancer [1-3]. A prolonged imbalance between calorie intake and expenditure is the main cause of obesity. Several factors contribute to this imbalance, including genetic factors, overeating, and physical inactivity [4]. In addition, dietary patterns, including the time, amount, and frequency of meals consumed per day, have been recognised as a probable contributing factor for obesity by influencing the feeling of satiety [5,6]. Recently, Intermittent Fasting (IF) has been considered an effective weight-loss strategy [7]. It is an ancient practice that includes periods of severe energy restrictions by voluntary abstinence from food and drinks, typically for 1-3 days/week [8]. Caloric restriction by IF has been shown to increase longevity and reduce the incidence of chronic NCDs [9].
Many types of IF exist, such as complete alternate-day fasting, time-restricted feeding, modified fasting regimens, and periodic fasting. In complete alternate-day fasting, energy-containing foods or drinks are not consumed on alternate fasting days. In time-restricted feeding, ad libitum energy intake is allowed within specific time frames persuading consistent, extended fasting intervals. A modified fasting regimen permits the consumption of only 20%-25% of baseline energy requirement on arranged fasting days [10,11], which includes energy intake constraints for only two non-consecutive days/week with ad libitum eating for the other days.
Various fasting regimens are also undertaken for spiritual or religious purposes. Many religions and cultures practice IF; for example, Muslims worldwide fast every year during the holy month of Ramadan, the fourth pillar of Islam. During Ramadan fasting, people mostly take two meals, one large meal after dusk and a lighter meal before dawn. Beside Ramadan fasting, Muslims have the so-called “voluntary IF,” which is fasting for two days per week (i.e., Monday and Thursday) from sunrise to sunset [10,11]. To the best of the authors’ knowledge, none of the previous studies investigated the potential impacts of Muslims voluntary IF on health. Therefore, this study was intended to examine the association between voluntary IF (two days a week; Monday and Thursday) with BMI, PA, and sleep pattern.
Materials and Methods
This was a survey-based study conducted for three months, and a total of 1,242 participants (245 males and 997 females) completed an online questionnaire and were included in the study. The study was approved by the Institutional Review Board and Ethical Committee of King Saud University, Riyadh, Saudi Arabia (KSU-HE-19- 108).
Sample size calculation: The sample size of 385 participants was calculated using Raosoft Sample Size Calculator (Raosoft, Inc 2004, http://www.raosoft.com/samplesize.html), keeping a 5% margin of error and a 95% confidence interval. However, a larger sample size, 1,242 participants, were considered in the study to minimise the errors.
Inclusion criteria: The target population was Saudi adults (Muslims) aged 18 years and above with access to the internet.
Exclusion criteria: The exclusion criteria included individuals below 18 years, and individuals with incomplete responses.
A cross-sectional approch was used to assess the effect of fasting two days/week on BMI, PA, and sleep pattern in Saudi adults. Data were collected using a self-administered questionnaire that had been assembled by the authors and reviewed by experts in the related field. Adjustments were made based on expert input, and pilot test feedback to strengthen the reliability.
Study Questionnaire
The study questionnaire was delivered in Arabic language, as the targeted study participants were Saudi, and it was organised to obtain data about: (1) socio-demographic and anthropometric characteristics; (2) fasting related questions; (3) PA; and (4) sleep pattern. To reach a greater number of participants, the questionnaire was published on an online survey platform (Google Forms), and its designated link was circulated through social media (i.e., Twitter, Instagram, Telegram, and WhatsApp). The snowball sampling was employed to recruit participants.
An introductory paragraph outlining the aim of the study was posted along with the questionnaire. The participants were asked to provide consent of participation. Each participant was guaranteed that the information given was only for study purposes and would be kept confidential. The participants could interrupt or quit the questionnaire at any point without explanation.
Socio-demographic and anthropometric characteristics: The participants were asked to answer the questions regarding their age, gender, marital status, educational level, monthly income of the family. Self-reported height and body weight were also obtained. BMI was calculated using the standard formula wherein body weight divided by the square of height, and is expressed in units of kg/m2.
Fasting related questions: The questions about fasting had three main questions. (1) Do you fast two days (i.e., Monday and Thursday) every week? “yes” or “no”. (2) What is your goal for fasting two days (i.e., Monday and Thursday) every week? “weight loss”, “religious purpose” or “diet for a particular disease”. (3) Did you ever follow any diet other than voluntary IF? “Yes” or “no”.
Physical Activity (PA): A short-modified version of the International PA Questionnaire (IPAQ) was used to evaluate the PA levels of the participants [12]. The IPAQ collects information pertaining to the time (i.e., the number of days and average time per day) spent on PA and the intensity of this activity (vigorous or moderate; walking or sitting).
Sleep pattern: Data on sleep pattern were collected through the following questions: (1) How many hours do you sleep per day? “2-3 hours,” “3-5 hours,” “5-7 hours,” or “more than 7 hours”. (2) Your sleep period is usually “morning” or “evening”? (3) How often do you wake up during sleep? “None,” “one,” “2 times,” or “more than 2 times.” (4) How much time do you spend trying to sleep? “15 minutes or less,” “16-30 minutes,” “31-45 minutes,” “46-60 minutes,” or “more than 60 minutes.” In addition to these questions, the Epworth Sleep Scale was used to assess participants’ sleepiness [13].
Statistical Analysis
The obtained data were cleaned, organised, coded, and analysed using Statistical Package for Social Sciences, version 21 (IBM Corp., Armonk, NY, USA). Continuous data were checked for normality using the Kolmogorov-Smirnov test. Descriptive statistics was performed using frequencies and percentages (%) for categorical variables and mean±Standard Deviation (SD) for continuous variables. The differences between fasting and non fasting groups were tested using Chi-square test or an exact probability test (for small frequencies) for categorical data and unpaired t-test for continuous data. A p-value of less than 0.05 was considered statistically significant.
Results
Participant’s characteristics: Socio-demographic and anthropometric characteristics of the study participants are shown in [Table/Fig-1]. Most participants (n=997; 80.3%) were female, and the age of 79.5% (n=988) of the overall participants ranged from 18 to 30 years. Further, the majority of them were unmarried (n=776; 62.5%) and had a bachelor’s degree (n=752; 60.5%). Total 541 (43.6%) participants had a family income of SR 5,000-15,000. In addition, 18.44% (n=229) of the overall participants used to fast for two days/week and their BMI was slightly higher than that of the non fasting group (26.56±6.41 kg/m2 and 25.18±6.41 kg/m2, respectively) (p<0.05). Significant associations between fasting and socio-demographic and anthropometric characteristics (gender, age, marital status, educational level, monthly income, weight and BMI) were observed.
Socio-demographic and anthropometric characteristics of study participants.
| Variables | Total N=1242 | Non fasting n=1013 | Fasting n=229 | p-value* |
|---|
| Gender |
| Male | 245 (19.7%) | 212 (20.93%) | 33 (14.41%) | 0.025 |
| Female | 997 (80.3%) | 801 (79.07%) | 196 (85.59%) |
| Age (years) |
| 18-30 | 988 (79.5%) | 819 (80.85%) | 169 (73.80%) | <0.001 |
| 31-50 | 241 (19.4%) | 189 (18.66%) | 52 (22.71%) |
| Older than 51 | 13 (1.05%) | 5 (0.49%) | 8 (3.49%) |
| Marital status |
| Single | 776 (62.5%) | 644 (63.57%) | 132 (57.64%) | 0.004 |
| Married | 426 (34.3%) | 341 (33.66%) | 85 (37.12%) |
| Divorced | 30 (2.4%) | 24 (2.38%) | 6 (2.62%) |
| Widow | 10 (0.8%) | 4 (0.39%) | 6 (2.62%) |
| Educational level |
| Intermediate level or less | 28 (2.3%) | 14 (1.38%) | 14 (6.12%) | <0.001 |
| High school | 300 (24.2%) | 248 (24.48%) | 52 (22.70%) |
| Bachelor degree | 752 (60.5%) | 619 (61.11%) | 133 (58.08%) |
| Post graduate | 162 (13.0%) | 132 (13.03%) | 30 (13.1%) |
| Family monthly income (SR) |
| Less than 5,000 | 440 (35.4%) | 345 (34.06%) | 95 (41.48%) | 0.037 |
| From 5,000 to 15,000 | 541 (43.6%) | 456 (45.01%) | 85 (37.12%) |
| From 15,000 to 30,000 | 195 (15.7%) | 163 (16.09%) | 32 (13.98%) |
| More than 30,000 | 66 (5.3%) | 49 (4.84%) | 17 (7.42%) |
| Height (m) | 1.61±0.085 | 1.61±0.084 | 1.61±0.088 | 0.538 |
| Weight (Kg) | 66.10±18.26 | 65.50±18.22 | 68.71±18.24 | 0.016 |
| BMI (kg/m2) | 25.43±6.43 | 25.18±6.41 | 26.56±6.41 | 0.003 |
Data are presented as frequency and percentage (%) for categorical variables and mean±Standard Deviation (SD) for continuous variables; *p-value significant <0.05; p-value tested by Chi square test or an exact probability test (for small frequencies) for categorical data and unpaired t-test for continuous data; BMI: Body mass index; SAR: Saudi Riyal
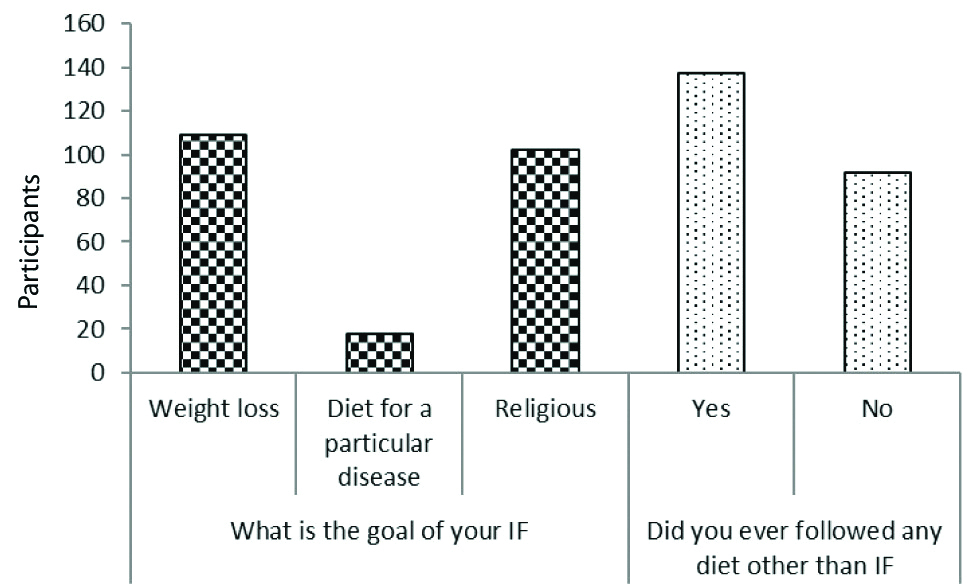
Participant’s response to questions on fasting [Table/Fig-2]: Regarding the reasons for IF, almost half of the participants (47.59%) reported that the main reason for IF was the desire to lose weight, followed by religious views (44.54%) and treatment of any disease (7.87%). Furthermore, 137 (59.82%) participants followed diets other than IF.
Participants response to the IF questions.
IF: Intermittent fasting
Levels of Physical Activity (PA) and sleep pattern [Table/Fig-3]: It shows the PA levels and sleep pattern of fasting participants compared with non fasting participants. A significant difference in PA levels was observed between the two groups (p<0.05), but overall, the participants were engaged in a low PA level as it was 58.8% for fasting participants and 49.78% for those who are not fasting. No significant difference in sleep pattern, such as sleepiness during the day and sleep duration was found between the two groups. On the other hand, significant differences in the time needed to fall asleep and frequency of waking up during sleep were observed between the two groups (p<0.05).
Levels of physical activity and sleep pattern of fasting participants compared with those of non fasting participants.
| Variables | All (n=1242) | Non fasting (n=1013) | Fasting (n=229) | p-value* |
|---|
| PA level | Low | 710 (57.17) | 596 (58.8) | 114 (49.78) | 0.001 |
| Moderate | 276 (22.22) | 228 (22.6) | 48 (20.96) |
| High | 256 (20.61) | 189 (18.6) | 67 (29.26) |
| Sleepiness | Normal | 620 (49.92) | 506 (49.95) | 114 (49.7) | 0.94 |
| Average amount | 214 (17.23) | 176 (17.37) | 38 (16.7) |
| Excessive sleepy | 408 (32.85) | 331 (32.68) | 77 (33.6) |
| Duration of sleep | 2 to 3 hours | 17 (1.37) | 11 (1.1) | 6 (2.62) | 0.21 |
| 3 to 5 hours | 171 (13.76) | 136 (13.4) | 35 (15.28) |
| 5 to 7 hours | 675 (54.35) | 550 (54.3) | 125 (54.59) |
| More than 7 hours | 379 (30.52) | 316 (31.2) | 63 (27.51) |
| Frequency of waking up | Never | 216 (17.39) | 188 (18.5) | 28 (12.23) | 0.03 |
| Once | 353 (28.42) | 273 (26.9) | 80 (34.93) |
| Twice | 363 (29.23) | 296 (29.3) | 67 (29.26) |
| Thrice or more | 310 (24.96) | 256 (25.3) | 54 (23.58) |
| Time required to sleep | 0-15 min | 459 (36.96) | 356 (35.15) | 103 (44.8) | 0.02 |
| 16-30 min | 427 (34.38) | 357 (35.25) | 70 (30.7) |
| 31-45 min | 190 (15.30) | 166 (16.38) | 24 (10.6) |
| 45-60 min | 77 (6.19) | 65 (6.42) | 12 (5.2) |
| More than 60 min | 89 (7.17) | 69 (6.80) | 20 (8.7) |
Data are presented as frequency and percentage (%); *p-value significant <0.05; p-value tested by Chi-square test
Discussion
In this study, the association between voluntary IF (twice/week; i.e., Monday and Thursday) and BMI, PA, and sleep pattern among Saudi adults has been explored. The study results have shown that the BMI of those who used to fast for two days/week was slightly higher than that of the other group. Unlike calorie-restrictive diet protocols, IF requires deprivation of food mostly on alternate days during the week [14]. Various studies have revealed that IF may be an effective tool for losing weight in overweight or obese people [15-17]. However, in this study, the mean BMI of the participants who were fasting was higher than that of those who were not fasting. Soeters MR et al., have reported that the decrease in resting energy expenditure after IF indicates an increase in weight during IF when caloric intake is not adjusted [18]. In addition, Lima CHR et al., and Catenacci VA et al., did not notice any substantial fasting effects on the body weight of overweight and obese individuals in the IF group [19,20]. Azizi F et al., have mentioned that the effects of Ramadan fasting on weight differs between individuals [21]. It ranges from weight loss to increases in weight, depending mostly on energy consumption in the non fasting period. The focal pathophysiological mechanism of the decrease in weight due to an IF diet is the reduction in the consumption of calories [10]. Other factors responsible for these discrepancies may be the differences in socio-economic status, fasting hours, gender, ethnicity, medical history, and health status [22,23]. In this study, a statistically significant difference in PA levels was observed between the two groups. Ben Salma F et al., investigated the effects of Ramadan IF and revealed that, fasting reduced the physical performance of fasting high-school Tunisian students in both 100-m and 800-m races [24]. In another study, the time taken by footballers to complete a dribbling test increased by approximately 9% during Ramadan [25]. Moderate to high PA levels with a moderate diet are a useful tool for losing weight in people with excess weight [26]. IF regimens are hypothesised to influence the metabolic regulation via their effects on circadian biology, gut microbiome, and modifiable lifestyle behaviour [27].
Each cell, tissue, and organ is under the control of a biological clock, which maintains the normal tissue functioning by regulating the expression of tissue-specific genes and following a circadian pattern [28]. The central biological clock, also known as the Suprachiasmatic Nucleus (SCN), is located in the hypothalamus and is entrained mainly by light. However, every single cell in the body has Peripheral Clocks (PCs) [28], which are influenced by neurohormonal factors and mealtime [29,30]. It has been suggested that desynchronisation between PCs and the SCN affects energy balance and increases the risk of chronic diseases. During Ramadan fasting, and involuntary fasting by Muslims, the times of meals shift between sunset and dawn. Some studies that accounted for sleep duration, sleep-wake schedule, energy expenditure, caloric consumption, light exposure, and meal timings have demonstrated no changes in the circadian rhythm during fasting if the meals were served early at night and if the participants sleep early according to their usual routine and then wake up for a pre-dawn meal in the early morning [31-34]. In this study, no significant difference in sleepiness and sleep duration was observed between the two groups. The results conform to those reported in other studies [35,36]. The main strength of this study is that it is, to the best of the authors’ knowledge, the first study that demonstrated the interest of participants from the Saudi community in voluntary IF and identified the potential impacts of this type of IF. This allows it to be applied as a pilot study in Saudi Arabia.
Limitation(s)
The study has several limitations. Among those one of the key limitations was that data, such as anthropometric measurement, were self-measured and self-reported online, which may have a measurement error. In addition, based on the study recruitment technique, it is more likely that mainly younger and educated individuals accessed the online questionnaire. Therefore, the study did not represent the overall Saudi population.
Conclusion(s)
This study shows that fasting two days/week does not affect BMI when meal timings are restrained to the early evening and pre-dawn periods, with adequate night sleep. It may be an appropriate beginning point to further develop strategies to sustain any beneficial effects of the IF on obesity.
Data are presented as frequency and percentage (%) for categorical variables and mean±Standard Deviation (SD) for continuous variables; *p-value significant <0.05; p-value tested by Chi square test or an exact probability test (for small frequencies) for categorical data and unpaired t-test for continuous data; BMI: Body mass index; SAR: Saudi Riyal
Data are presented as frequency and percentage (%); *p-value significant <0.05; p-value tested by Chi-square test